Clofazimine (Monograph)
Brand name: Lamprene
Drug class:
Introduction
Phenazine dye with antimycobacterial and anti-inflammatory activity.
Uses for Clofazimine
Leprosy
Treatment of lepromatous leprosy, including dapsone-resistant lepromatous leprosy and leprosy complicated by erythema nodosum leprosum (ENL) reactions. Used in conjunction with other anti-infectives active against Mycobacterium leprae.
Treatment of multibacillary leprosy (>5 lesions or skin smear positive for acid-fast bacteria) in rifampin-based multiple-drug regimens. WHO recommends a 12-month multiple-drug regimen that includes rifampin, clofazimine, and dapsone.
Treatment of paucibacillary leprosy (1–5 lesions) when dapsone cannot be used. WHO recommends a 6-month multiple-drug regimen of rifampin and dapsone; if dapsone must be discontinued because of severe adverse effects, WHO recommends that clofazimine be substituted.
Rifampin-based multiple-drug regimens are recommended for the treatment of all forms of leprosy; multiple-drug regimens may reduce infectiousness of the patient more rapidly and delay or prevent emergence of rifampin-resistant M. leprae.
Alternative for treatment and prevention of erythema nodosum leprosum (ENL) reactions (lepra type 2 reactions) in leprosy patients. Not as effective or as rapidly acting as other agents used in the treatment of ENL (e.g., corticosteroids, thalidomide); do not use alone for treatment of severe ENL.
Has been used for treatment of reversal (type 1) reactions† [off-label] in patients with borderline or tuberculoid leprosy. Efficacy not fully evaluated; may aggravate the reactional state in some patients.
Not effective in the treatment of other leprosy-associated inflammatory reactions (e.g., Lucio’s phenomenon, downgrading reactions).
Not commercially available in the US, but may be obtained for treatment of leprosy from the National Hansen’s Disease Program (NHDP) of the US Department of Health and Human Services, Health Resources and Services Administration (HRSA). In rare circumstances, also may be made available from NHDP for other uses. (See Restricted Distribution under Dosage and Administration.)
Treatment of leprosy and management of leprosy reactional states is complicated and should be undertaken in consultation with a specialist familiar with the disease. For information, consult NHDP by phone at 225-578-9861 or 800-642-2477, by fax at 225-578-9856, or on the Internet at .
Mycobacterium Avium Complex (MAC) Infections
Has been used in multiple-drug regimens for treatment of pulmonary and localized extrapulmonary Mycobacterium avium complex (MAC) infections† [off-label], but safety and efficacy not established. ATS and IDSA state the role of clofazimine in the treatment of MAC lung disease is not established.
Should not be used for treatment of disseminated MAC infections† [off-label], including infections that have failed to respond to or are resistant to other drugs. There is some evidence clofazimine is ineffective in these infections and may even be associated with reduced survival.
Use of clofazimine for the treatment of any disease other than leprosy is discouraged by WHO and the manufacturer since indiscriminate use may promote emergence of resistant strains of M. leprae. (See Restricted Distribution under Dosage and Administration.)
Treatment of MAC infections is complicated and should be directed by clinicians familiar with mycobacterial diseases; consultation with a specialist is particularly important when the patient cannot tolerate first-line drugs or when the infection has not responded to prior therapy or is caused by macrolide-resistant MAC.
Multidrug-resistant Tuberculosis (MDRTB)
Has been used in multiple-drug regimens for the treatment of MDRTB† [off-label], but safety and efficacy not established. Not included in current CDC, ATS, and IDSA recommendations for treatment of tuberculosis.
Use of clofazimine for the treatment of any disease other than leprosy is discouraged by WHO and the manufacturer since indiscriminate use may promote emergence of resistant strains of M. leprae. (See Restricted Distribution under Dosage and Administration.)
Inflammatory or Pustular Dermatoses
Has been used in a variety of inflammatory or pustular dermatoses† [off-label], but safety and efficacy not established.
Use of clofazimine for the treatment of any disease other than leprosy is discouraged by WHO and the manufacturer since indiscriminate use may promote emergence of resistant strains of M. leprae. (See Restricted Distribution under Dosage and Administration.)
Clofazimine Dosage and Administration
Administration
Restricted Distribution
Not commercially available in the US, but may be obtained for treatment of leprosy from the National Hansen’s Disease Program (NHDP) of the US Department of Health and Human Services, Health Resources and Services Administration (HRSA). In rare circumstances, may also may be made available from NHDP for other uses.
For treatment of leprosy, clofazimine is distributed under an Investigational New Drug (IND) application held by NHDP and is available at no cost after the clinician has registered as an investigator under the IND protocol. Clinicians requiring clofazimine for a patient with leprosy should contact the Administrative Officer of the Laboratory Research Branch at NHDP by mail at Skip Berman Drive, Baton Rouge, LA 70803, by phone at 225-578-9861 or 800-642-2477, or by fax at 225-578-9856.
If use of clofazimine is considered necessary in situations where there are no other comparable or satisfactory treatments available (e.g., treatment of MDRTB), the drug can be distributed by NHDP under a single-patient treatment IND protocol administered by FDA. To obtain the drug for any use other than treatment of leprosy, clinicians must first contact the Division of Special Pathogen and Immunologic Drug Products (HFD-590), Center for Drug Evaluation and Research of the FDA by phone at 301-796-1600 to register as an investigator under the single-patient treatment IND protocol. After FDA approval of the single-patient treatment IND, FDA will request NHDP to distribute clofazimine directly to the prescriber.
Oral Administration
Administer orally. To maximize absorption, give with a meal.
Dosage
Pediatric Patients
Leprosy
Multibacillary Leprosy
OralChildren ≤10 years of age†: Appropriately adjust dosage (e.g., clofazimine 50 mg twice weekly plus 100 mg once monthly given in conjunction with rifampin [300 mg once monthly] and dapsone [25 mg daily]). Continue multiple-drug regimen for 12 months.
Children 10–14 years of age: 50 mg once every second day plus 150 mg once monthly given in conjunction with rifampin (450 mg once monthly) and dapsone (50 mg once daily). Continue multiple-drug regimen for 12 months.
Adolescents ≥15 years of age: 50 mg once daily plus 300 mg once monthly given in conjunction with rifampin (600 mg once monthly) and dapsone (100 mg once daily). Continue multiple-drug regimen for 12 months.
An additional 12 months of therapy may be indicated for patients with a high bacteriologic index who demonstrate no improvement (with evidence of worsening) following completion of the initial 12 months of treatment.
Adults
Leprosy
Multibacillary Leprosy
Oral50 mg once daily plus 300 mg once monthly given in conjunction with rifampin (600 mg once monthly) and dapsone (100 mg once daily). Continue multiple-drug regimen for 12 months.
An additional 12 months of therapy may be indicated for patients with a high bacteriologic index who demonstrate no improvement (with evidence of worsening) following completion of the initial 12 months of treatment.
Paucibacillary Leprosy in Patients Unable to Take Dapsone
Oral50 mg once daily plus 300 mg once monthly given in conjunction with rifampin (600 mg once monthly). Continue multiple-drug regimen for 6 months.
Erythema Nodosum Leprosum (ENL) Reactions
OralDosage and duration of clofazimine treatment depend on severity of symptoms.
100–300 mg daily given in 2 or 3 divided doses for up to 3 months or longer may reduce or eliminate corticosteroid requirements. Severe, corticosteroid-dependent ENL may require more prolonged treatment (up to 7 months) and extended treatment (an additional 9–24 months) may be necessary to prevent recurrence.
Although dosages up to 400 mg daily have been used to control ENL in some adults, manufacturer states dosage >200 mg daily not recommended.
Reduce clofazimine dosage to lowest effective level (e.g., 100 mg daily) as soon as possible after reactive episode is controlled.
Prescribing Limits
Pediatric Patients
Leprosy
Oral
Dosage >100 mg daily should be given for as short a period as possible and only under close medical supervision. (See Cautions.)
Dosage >200 mg daily not recommended.
Adults
Leprosy
Oral
Dosage >100 mg daily should be given for as short a period as possible and only under close medical supervision. (See Cautions.)
Dosage >200 mg daily not recommended.
Special Populations
No special population dosage recommendation at this time.
Cautions for Clofazimine
Contraindications
Manufacturer states no known contraindications.
Warnings/Precautions
Warnings
GI Effects
Severe GI effects (e.g., splenic infarction, bowel obstruction, GI bleeding) reported rarely. Exploratory laparotomies were necessary in some patients; several fatalities reported. Although exact cause unknown, autopsies revealed massive deposits of clofazimine crystals in various tissues (e.g., intestinal mucosa, liver, spleen, mesenteric lymph nodes).
Many patients (40–50%) experience abdominal and epigastric pain, diarrhea, nausea, vomiting, and GI intolerance.
GI effects are dose related and occur most frequently with dosage >100 mg daily. Dosage >100 mg daily should be used for as short a period as possible and only under close medical supervision.
Use with caution in patients with GI problems such as abdominal pain and diarrhea.
If patient complains of colicky or burning abdominal pain, nausea, vomiting, or diarrhea, reduce clofazimine dosage and, if necessary, increase interval between doses or discontinue the drug.
General Precautions
Dermatologic Effects
Pink to brownish-black discoloration of skin occurs in most patients (75–100%) and is evident within 1-4 weeks after initiation of clofazimine. Degree of discoloration is dose related and is most pronounced on exposed body parts (e.g., hairless facial skin in periorbital and perinasal areas, hairless hypopigmented skin on palms and soles) and in areas with leprosy lesions. Gradually disappears within 6-12 months after drug discontinued, but traces of color may remain for ≥4 years in some individuals.
Clofazimine is a bright-red dye and skin discoloration apparently occurs because drug crystals distribute to and accumulate in tissues and fluids. May be particularly disturbing to light-skinned individuals; may cause substantial compliance problems in certain patients or populations. Depression secondary to skin discoloration reported; may have contributed to at least 2 suicides. Warn patients that skin discoloration, as well as discoloration of the conjunctiva and body fluids, may occur. (See Ocular Effects under Cautions.) Appropriate counseling (e.g., advantages of clofazimine, reversibility of discoloration) may be sufficient to encourage patients to continue treatment.
Melanosis, similar to that reported with phenothiazines, also has caused skin discoloration in patients receiving clofazimine. Discoloration is blue-grey or blackish brown to black; resolves gradually following discontinuance of the drug but may persist as circumscribed hyperpigmented areas in some patients. During treatment, leprosy nodules may be replaced by scar tissue in the form of shiny, jet black, circular macules.
Ichthyosis and dry skin (especially on legs and forearms) generally occurs as leprosy resolves. May be relieved by applying oil, petrolatum, or an emollient lotion containing 25% urea to affected areas. Desquamation may occur.
Ocular Effects
Reversible, dose-related, red-brown discoloration of the conjunctiva, cornea, and lacrimal fluid may occur. Bilateral, linear or branched, brownish lines or streaks in the cornea reported in some patients receiving clofazimine dosages of 100–400 mg daily for ≥2 months; these lines slowly disappeared after clofazimine treatment was completed. Discoloration in the macular areas of the eye and bluish discoloration of the lens also reported rarely.
Discoloration of the conjunctiva and other parts of the eye does not appear to affect visual acuity, but diminished vision reported rarely.
Dryness, burning, itching, irritation, and watering of the eyes also reported.
Discoloration of Body Fluids
Reversible, dose-related, red-brown discoloration of sweat, sputum, urine, feces, nasal secretions, semen, and breast milk may occur.
Specific Populations
Pregnancy
Category C.
Crosses the placenta. Deeply pigmented skin reported in infants born to women who received clofazimine during pregnancy; discoloration gradually faded over the first year. No evidence of teratogenicity in these infants.
Use during pregnancy only if potential benefits justify risk to fetus.
Lactation
Distributed into human milk. Red-brown discoloration of breast milk may occur. Do not use in nursing women unless clearly indicated.
Pediatric Use
Safety and efficacy not established in children ≤12 years.
Has been used in pediatric patients; included in WHO guidelines for treatment of multibacillary leprosy in children.
Geriatric Use
Insufficient experience in patients ≥65 years of age and older to determine whether geriatric patients respond differently than younger adults. Clinical experience has not identified differences in response relative to younger adults.
Select dosage with caution, usually initiating therapy at the low end of the dosage range, because of age-related decreases in hepatic, renal, and/or cardiac function and concomitant disease and drug therapy.
Common Adverse Effects
Discoloration of skin, eyes, urine, feces, sputum, sweat, tears; GI effects (abdominal and epigastric pain, diarrhea, nausea, vomiting, GI intolerance); eye irritation, itching, dryness, burning.
Drug Interactions
Specific Drugs
|
Drug |
Interaction |
Comments |
|---|---|---|
|
Dapsone |
Concomitant use of dapsone and clofazimine does not have a clinically important effect on dapsone pharmacokinetics Some evidence suggests dapsone may decrease or nullify some anti-inflammatory effects of clofazimine and theoretically might adversely affect clofazimine’s efficacy in patients with ENL reactions; several borderline leprosy and lepromatous leprosy patients with severe, recurrent ENL reactions reportedly required higher clofazimine dosage to control these reactions when dapsone therapy was given concomitantly than when clofazimine was given alone |
Manufacturer states that an interaction between dapsone and clofazimine that adversely affects clofazimine’s anti-inflammatory effects has not been confirmed and advises that treatment with both drugs be continued in patients who develop leprosy-associated inflammatory reactions, including ENL, during concomitant therapy |
|
Isoniazid |
Possible increased clofazimine plasma and urine concentrations and decreased clofazimine skin concentrations |
|
|
Rifampin |
Although one study indicated that concomitant use of clofazimine in leprosy patients receiving rifampin alone or in conjunction with dapsone may decrease plasma concentrations and AUC of rifampin, concomitant use of clofazimine in another study in lepromatous leprosy patients receiving dapsone (100 mg daily) and rifampin (600 mg daily) did not affect rifampin pharmacokinetics |
Clofazimine Pharmacokinetics
Absorption
Bioavailability
Incompletely absorbed from GI tract following oral administration. Extent of absorption exhibits considerable interindividual variation and depends on several factors (e.g., particle size, dosage form, dosage, presence of food in GI tract).
When clofazimine capsules are used, 45-70% of dose is absorbed.
Peak serum concentrations usually attained within 4-12 hours when dose is given with food.
Food
Food increases rate and extent of absorption. If administered with food containing fat and protein, AUC increased by 60% and peak serum concentrations increased by 30%.
Plasma Concentrations
Steady-state serum concentrations average 0.7 and 1 mcg/mL after dosages of 100 mg and 300 mg once daily, respectively.
Multiple-dose studies indicate steady-state serum concentrations may not be attained until ≥30 days after initiation after clofazimine therapy.
Distribution
Extent
Highly lipophilic. Distributed principally to fatty tissue and cells of the reticuloendothelial system; taken up by macrophages throughout the body.
Accumulates in highest concentrations in mesenteric lymph nodes, adipose tissue, adrenals, liver, lungs, gallbladder, bile, and spleen. Lower concentrations in skin, small intestine, lungs, heart, kidneys, pancreas, muscle, omentum, and bone.
Does not distribute into brain or CSF.
Crosses human placenta.
Distributed into human milk.
Elimination
Metabolism
Metabolic fate not fully elucidated. Appears to be partially metabolized; at least 3 metabolites appear to be eliminated in urine.
Elimination Route
Principally excreted in feces, both as unabsorbed drug and via biliary elimination. Following a single oral dose, 35–74% of dose may be excreted unchanged in feces over the first 72 hours.
Elimination of unchanged clofazimine and its metabolites in urine is negligible during the first 24 hours. Following multiple oral doses, <1% of daily dose is excreted in urine over a 24-hour period.
Small amounts excreted in sputum, sebum, and sweat.
Half-life
Following a single oral dose, there is an initial distribution phase followed by a slow elimination phase with a terminal elimination half-life of approximately 8 days.
Tissue half-life following multiple oral doses is estimated to be ≥70 days. Remains in body tissues for prolonged periods; has been found in skin and in mesenteric lymph nodes 2 and 4 years, respectively, after the drug was discontinued.
Stability
Storage
Oral
Capsules
≤30ºC in airtight container; protect from moisture.
Actions and Spectrum
-
Phenazine dye with antimycobacterial and anti-inflammatory activity. Commercially available as capsules containing micronized clofazimine suspended in an oil-wax base.
-
Mechanism of action against mycobacteria not fully elucidated. Appears to exert antimycobacterial effect by binding preferentially to mycobacterial DNA and inhibiting replication and growth.
-
Exerts anti-inflammatory and immunosuppressive effects in vitro and in vivo. Precise mechanisms of these effects not fully elucidated, but appears to cause dose-dependent inhibition of neutrophil motility and also inhibits mitogen-induced lymphocyte transformation. May enhance phagocytic activity of polymorphonuclear cells and macrophages and enhance membrane-associated oxidative metabolism in these cells.
-
Clofazimine’s anti-inflammatory and immunosuppressive effects, in addition to antimycobacterial effects, appear to contribute to efficacy in the treatment and prevention of ENL reactions.
-
Slowly bactericidal against Mycobacterium leprae in vivo. Bactericidal against M. tuberculosis and M. marinum in vitro, but appears to be only bacteriostatic in vitro against other mycobacteria, including M. avium complex (MAC).
-
M. leprae resistant to clofazimine reported only rarely.
-
Cross-resistance between clofazimine and dapsone or rifampin not reported to date. However, there are rare reports of M. leprae resistant to both clofazimine and dapsone, but susceptible to rifampin.
Advice to Patients
-
Importance of taking with meals.
-
Advise patients that clofazimine may cause pink to brownish-black discoloration of skin and also may cause red-brown discoloration of eyes and body fluids (e.g., tears, sweat, sputum, urine, feces). Counsel patients that such discoloration is reversible, but may take several months or years to disappear after treatment is finished; advise them of the importance of continuing treatment.
-
Importance of immediately informing clinician if abdominal symptoms (colicky or burning pain in the abdomen, nausea, vomiting, diarrhea) occur.
-
Importance of taking only as prescribed; do not increase dosage or duration of therapy unless otherwise instructed by a clinician.
-
Advise patients that if skin dryness and ichthyosis occur, these effects may be relieved by applying oil to the skin.
-
Importance of women informing their clinician if they are or plan to become pregnant or plan to breast-feed.
-
Importance of informing patients of other important precautionary information. (See Cautions.)
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
Clofazimine is no longer commercially available in the US. However, the drug may be obtained for treatment of leprosy by contacting the National Hansen’s Disease Program (NHDP) of the US Department of Health and Human Services, Health Resources and Services Administration (HRSA) at 225-578-9861 or 800-642-2477. In rare circumstances, the drug also may be made available from NHDP for other uses by contacting the FDA Division of Special Pathogen and Immunologic Drug Products (HFD-590), Center for Drug Evaluation and Research at 301-796-1600. (See Restricted Distribution under Dosage and Administration.)
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
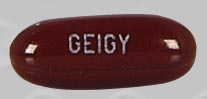
Oral |
Capsules |
50 mg |
Lamprene |
Novartis |
AHFS DI Essentials™. © Copyright 2024, Selected Revisions April 10, 2024. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
† Off-label: Use is not currently included in the labeling approved by the US Food and Drug Administration.
Reload page with references included
More about clofazimine
- Check interactions
- Compare alternatives
- Side effects
- Dosage information
- During pregnancy
- Drug class: leprostatics
- Breastfeeding