Etravirine (Monograph)
Brand name: Intelence
Drug class: HIV Nonnucleoside Reverse Transcriptase Inhibitors
Introduction
Antiretroviral; HIV nonnucleoside reverse transcriptase inhibitor (NNRTI).1
Uses for Etravirine
Treatment of HIV Infection
Treatment of HIV-1 infection in adults and pediatric patients ≥2 years of age who are treatment-experienced; used in conjunction with other antiretrovirals.1 2 3 300 301 302 303
Used as part of a fully suppressive antiretroviral regimen in treatment-experienced patients.200 201 202
Safety and efficacy not systematically evaluated in treatment-naïve patients.1 200
Postexposure Prophylaxis following Occupational Exposure to HIV
Postexposure prophylaxis of HIV infection following occupational exposure† [off-label] (PEP) in health-care personnel and other individuals.199
USPHS recommends 3-drug regimen of raltegravir in conjunction with emtricitabine and tenofovir disoproxil fumarate (tenofovir DF) as the preferred regimen for PEP following occupational exposures to HIV.199 Etravirine and 2 NRTIs is one of several alternative regimens.199
Management of occupational exposures to HIV is complex and evolving; consult infectious disease specialist, clinician with expertise in administration of antiretroviral agents, and/or National Clinicians’ Postexposure Prophylaxis Hotline (PEPline at 888-448-4911) whenever possible.199 Do not delay initiation of PEP while waiting for expert consultation.199
Etravirine Dosage and Administration
General
Patient Monitoring
-
Monitor for signs or symptoms of severe skin reactions or hypersensitivity reactions (e.g., severe rash or rash accompanied by fever, general malaise, fatigue, muscle or joint aches, blisters, oral lesions, conjunctivitis, facial edema, hepatitis, eosinophilia, angioedema).1
Dispensing and Administration Precautions
-
The Institute for Safe Medication Practices (ISMP) list of error-prone abbreviations, symbols, and dose designations states that the use of abbreviations for antiretroviral medications (e.g., DOR, TAF, TDF) during the medication use process should be avoided as their use has been associated with serious medication errors.304
Administration
Oral Administration
Administer orally twice daily after a meal.1
Swallow tablets whole with a liquid (e.g., water); do not chew.1
For patients unable to swallow tablets whole, place dose of etravirine tablets in 5 mL of water (enough to cover tablets) and stir until a uniform, milky dispersion occurs.1 Add 15 mL (1 tablespoon) of liquid; water may be used, but orange juice or milk may improve taste.1 Do not use carbonated beverages or warm (>40°C) water.1 Consume dispersion immediately; rinse glass several times with water, orange juice, or milk and swallow.1
Dosage
Pediatric Patients
Treatment of HIV Infection
Antiretroviral-experienced
OralChildren 2 years to <18 years of age weighing ≥10 kg: Dosage is based on weight and should not exceed recommended adult dosage.1 (See Table 1.)
|
Body Weight |
Dosage |
|---|---|
|
10 to <20 kg |
100 mg twice daily |
|
20 to <25 kg |
125 mg twice daily |
|
25 to <30 kg |
150 mg twice daily |
|
≥30 kg |
200 mg twice daily |
Adults
Treatment of HIV Infection
Antiretroviral-experienced
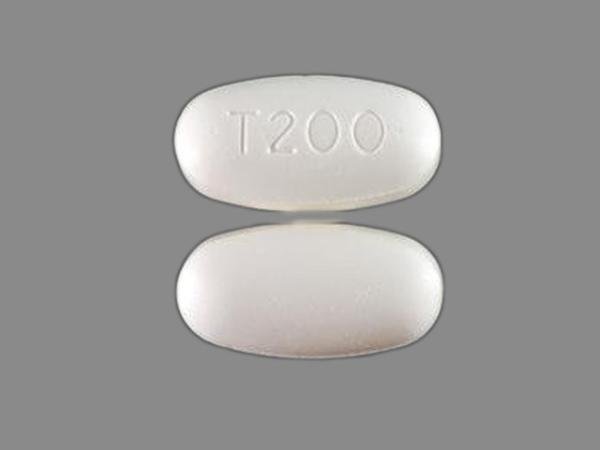
Oral200 mg twice daily.1 Give dose as a single 200-mg tablet or two 100-mg tablets.1
Postexposure Prophylaxis following Occupational Exposure to HIV† [off-label]
Oral
200 mg twice daily.199 Use in conjunction with 2 NRTIs.199
Initiate PEP as soon as possible following occupational exposure to HIV (preferably within hours); continue for 4 weeks, if tolerated.199
Special Populations
Hepatic Impairment
Dosage adjustments not necessary in patients with mild or moderate hepatic impairment (Child-Pugh class A or B).1 Pharmacokinetics not studied in patients with severe hepatic impairment (Child-Pugh class C).1
Dosage adjustments not necessary in HIV-infected adults coinfected with HBV and/or HCV.1
Renal Impairment
Dosage adjustments not necessary.1
Geriatric Patients
No specific dosage recommendations.1 Select dosage with caution because of age-related decreases in hepatic, renal, and/or cardiac function and concomitant disease and drug therapy.1
Cautions for Etravirine
Contraindications
-
None.1
Warnings/Precautions
Severe Skin and Hypersensitivity Reactions
Severe, potentially life-threatening and fatal skin reactions, including Stevens-Johnson syndrome, toxic epidermal necrolysis, and erythema multiforme, reported.1 Hypersensitivity reactions, including drug rash with eosinophilia and systemic symptoms (DRESS) characterized by rash and systemic symptoms (sometimes involving organ dysfunction such as hepatic failure), also reported.1
If severe hypersensitivity reactions (e.g., severe rash or rash with fever, malaise, fatigue, muscle or joint pain, blisters, oral lesions, conjunctivitis, facial edema, hepatitis, eosinophilia, angioedema) occur, immediately discontinue etravirine and initiate appropriate therapy.1 Monitor clinical status and liver transaminase concentrations.1
Rash of mild to moderate intensity also reported; generally occurs within first few weeks of therapy and resolves with continued therapy (median duration 12–16 days).1 2 3
Manufacturer states that history of rash while receiving other NNRTIs does not appear to increase the risk for etravirine-related rash.1
Drug Interactions
Risk of potentially significant drug interactions; may lead to loss of therapeutic effect or clinically significant adverse reactions.1
Consider potential for drug interactions prior to and during etravirine therapy and review concomitant medications during therapy.1
Fat Redistribution
Possible redistribution or accumulation of body fat, including central obesity, dorsocervical fat enlargement (“buffalo hump”), peripheral wasting, facial wasting, breast enlargement, and general cushingoid appearance.1 Mechanisms and long-term consequences of fat redistribution unknown; causal relationship not established.1
Immune Reconstitution Syndrome
During initial treatment, patients who respond to antiretroviral therapy may develop an inflammatory response to indolent or residual opportunistic infections (e.g., Mycobacterium avium, M. tuberculosis, cytomegalovirus [CMV], Pneumocystis jirovecii [formerly P. carinii]); may necessitate further evaluation and treatment.1
Autoimmune disorders (e.g., Graves' disease, polymyositis, Guillain-Barré syndrome, autoimmune hepatitis) reported to occur in the setting of immune reconstitution; time to onset is more variable and can occur many months after initiation of antiretroviral therapy.1
Specific Populations
Pregnancy
Antiretroviral Pregnancy Registry (APR) at 800-258-4263 or [Web].1
Limited human data indicate 1 birth defect in 66 first trimester exposures to etravirine-containing regimens.1 In animal studies, etravirine was not associated with adverse developmental effects.1
Lactation
Based on limited data, etravirine shown to be present in human breast milk.1 No data on effects on the breastfed infant or the effects on milk production.1
The HHS perinatal HIV transmission guideline provides updated recommendations on infant feeding.202 The guideline states that patients with HIV should receive evidence-based, patient-centered counseling to support shared decision making about infant feeding.202 During counseling, patients should be informed that feeding with appropriate formula or pasteurized donor human milk from a milk bank eliminates the risk of postnatal HIV transmission to the infant.202 Additionally, achieving and maintaining viral suppression with antiretroviral therapy during pregnancy and postpartum reduces the risk of breastfeeding HIV transmission to <1%, but does not completely eliminate the risk.202 Replacement feeding with formula or banked pasteurized donor milk is recommended when patients with HIV are not on antiretroviral therapy and/or do not have a suppressed viral load during pregnancy (at a minimum throughout the third trimester), as well as at delivery.202
Pediatric Use
Safety and efficacy not established in pediatric patients <2 years of age.1
Safety, efficacy, and pharmacokinetics evaluated in antiretroviral-experienced pediatric patients 2 years to <18 years of age weighing ≥10 kg; adverse effects similar to those reported in adults, although rash reported more frequently in pediatric patients.1 Postmarketing cases of Stevens-Johnson syndrome reported.1
Geriatric Use
Insufficient experience in patients ≥65 years of age to determine whether they respond differently than younger adults.1 Etravirine pharmacokinetics not considerably different within the age range (18–77 years) evaluated.1
Hepatic Impairment
Pharmacokinetics not altered in patients with mild or moderate hepatic impairment (Child-Pugh class A or B).1 12 Pharmacokinetics not studied in patients with severe hepatic impairment (Child-Pugh class C).1
Renal Impairment
Minimal renal clearance; decrease in clearance not expected in patients with renal impairment.1
Common Adverse Effects
Most common adverse effects (≥2%) of moderate to severe intensity in adults: rash and peripheral neuropathy.1
Most common adverse effects (≥2%) in pediatric patients: rash and diarrhea.1
Drug Interactions
Metabolized by CYP isoenzymes 3A, 2C9, and 2C19.1 Induces CYP3A; inhibits 2C9 and 2C19.1 Inhibits P-glycoprotein (P-gp).1
Drugs Affecting or Affected by Hepatic Microsomal Enzymes
Potential pharmacokinetic interactions with drugs that induce or inhibit CYP3A, 2C9, or 2C19 with possible altered metabolism of etravirine.1
Potential pharmacokinetic interaction with drugs that are substrates for CYP3A, 2C9, or 2C19 with possible altered metabolism of such drugs.1
Drugs Affected by P-gp Transport
Potential pharmacokinetic interaction with drugs that are substrates for P-gp.1
Specific Drugs
|
Drug |
Interaction |
Comments |
|---|---|---|
|
Abacavir |
No in vitro evidence of antagonistic antiretroviral effects 1 |
|
|
Antiarrhythmics (amiodarone, disopyramide, flecainide, systemic lidocaine, mexiletine, propafenone, quinidine) |
Possible decreased antiarrhythmic agent concentrations1 |
Use concomitantly with caution; monitor antiarrhythmic agent concentrations1 |
|
Anticoagulants, oral |
Possible increased warfarin concentrations1 |
Monitor INR; adjust warfarin dosage if needed1 |
|
Anticonvulsants (carbamazepine, phenobarbital, phenytoin) |
Possible decreased etravirine concentrations and decreased antiretroviral efficacy; decreased anticonvulsant concentrations1 |
Concomitant use not recommended1 |
|
Antifungals, azoles |
Fluconazole: Substantially increased etravirine concentrations and AUC; no clinically important change in fluconazole concentrations or AUC1 Itraconazole: Possible increased etravirine concentrations and decreased itraconazole concentrations1 Ketoconazole: Possible increased etravirine concentrations and decreased ketoconazole concentrations1 Posaconazole: Possible increased etravirine concentrations; no change in posaconazole concentrations1 Voriconazole: Substantially increased etravirine concentrations and AUC; increased voriconazole concentration and AUC1 |
Fluconazole: Dosage adjustments not needed for either drug; use caution because of limited safety data regarding increased etravirine concentrations1 Itraconazole: Adjustment of itraconazole dosage may be needed depending on other concomitantly administered drugs1 Ketoconazole: Adjustment of ketoconazole dosage may be needed depending on other concomitantly administered drugs1 Posaconazole: Manufacturer of etravirine states adjustment of posaconazole dosage may be needed depending on other concomitantly administered drugs1 Voriconazole: Use caution because of limited safety data regarding increased etravirine concentrations dosage adjustments not needed1 |
|
Antimalarials |
Fixed combination of artemether and lumefantrine (artemether/lumefantrine): Decreased concentrations and AUC of artemether, active metabolite of artemether (dihydroartemisinin), and lumefantrine; no clinically important effect on etravirine concentrations or AUC1 |
Artemether/lumefantrine: Dosage adjustments not needed; use concomitantly with caution since effect on antimalarial efficacy not known1 |
|
Antimycobacterials (rifabutin, rifampin, rifapentine) |
Rifabutin: Decreased concentrations of etravirine and rifabutin1 Rifampin: Substantially decreased etravirine concentrations possible1 Rifapentine: Substantially decreased etravirine concentrations possible1 |
Rifabutin: Recommended rifabutin dosage is 300 mg daily in patients receiving etravirine without a ritonavir-boosted PI; rifabutin not recommended in patients receiving etravirine with a ritonavir-boosted PI1 Rifampin: Concomitant use not recommended1 Rifapentine: Concomitant use not recommended1 |
|
Benzodiazepines (diazepam) |
Diazepam: Possible increased diazepam concentrations1 |
Diazepam: Decreased diazepam dosage may be needed1 |
|
Clarithromycin |
Increased etravirine concentrations; decreased clarithromycin concentrations and increased concentrations of the major metabolite (14-hydroxyclarithromycin)1 |
Consider an alternative to clarithromycin (e.g., azithromycin) for treatment or prophylaxis of MAC1 |
|
Clopidogrel |
Possible decreased concentrations of the active metabolite of clopidogrel1 |
Avoid concomitant use if possible; consider alternatives to clopidogrel1 |
|
Corticosteroids (dexamethasone) |
Dexamethasone: Possible decreased etravirine concentrations and decreased antiretroviral efficacy1 |
Use concomitantly with caution; consider alternatives to dexamethasone, especially when long-term corticosteroid use anticipated1 |
|
Digoxin |
Possible increased digoxin concentrations; no change in etravirine concentrations1 |
If digoxin and etravirine are initiated at the same time, initiate digoxin at the lowest dosage1 If etravirine is initiated in a patient already receiving digoxin, dosage adjustments not needed for either drug1 Monitor serum digoxin concentrations and adjust digoxin dosage to achieve desired clinical effect1 |
|
Emtricitabine |
No in vitro evidence of antagonistic antiretroviral effects1 |
|
|
Estrogens/progestins |
Hormonal contraceptives: Slight increase in ethinyl estradiol concentrations; no change in norethindrone concentrations1 |
Dosage adjustments not needed with oral contraceptives containing ethinyl estradiol and norethindrone1 |
|
Hepatitis C Antivirals (dacalastavir, elbasvir/grazoprevir |
Daclatasvir: Coadministration of etravirine with daclatasvir may decrease daclatasvir concentrations1 Elbasvir/grazoprevir: Coadministration of etravirine with elbasvir/grazoprevir may decrease concentrations of elbasvir and grazoprevir, leading to reduced therapeutic effect of elbasvir/grazoprevir1 |
Daclatasvir: Increase the dosage of daclatasvir to 90 mg once daily1 Elbasvir/grazoprevir: Avoid coadministration1 |
|
HMG-CoA reductase inhibitors (statins) |
Atorvastatin: Decreased atorvastatin concentrations; no change in etravirine concentrations1 Fluvastatin: Possible increased fluvastatin concentrations; no change in etravirine concentrations1 Lovastatin: Possible decreased lovastatin concentrations1 Pitavastatin: Possible increased pitavastatin concentrations1 Simvastatin: Possible decreased simvastatin concentrations1 |
Atorvastatin: Usual etravirine and atorvastatin dosages can be used; however, may need to adjust atorvastatin dosage based on clinical response1 Fluvastatin: May need to adjust fluvastatin dosage1 Lovastatin: May need to adjust lovastatin dosage based on clinical response1 Pitavastatin: May need to adjust pitavastatin dosage1 Simvastatin: May need to adjust simvastatin dosage based on clinical response1 |
|
HIV Entry and Fusion Inhibitors (enfuvirtide, maraviroc) |
Enfuvirtide: No in vitro evidence of antagonistic antiretroviral effects1 Maraviroc: Decreased maraviroc concentrations and AUC; no clinically important effect on etravirine concentrations or AUC1 No in vitro evidence of antagonistic antiretroviral effects1 |
Enfuvirtide: Dosage adjustments not needed1 Maraviroc: Recommended maraviroc dosage is 600 mg twice daily with usual etravirine dosage, provided regimen does not include a potent CYP3A inhibitor1 Recommended maraviroc dosage is 150 mg twice daily with the usual etravirine dosage if etravirine used in regimen that contains maraviroc and a ritonavir-boostedPI1 |
|
HIV Integrase Inhibitors (INSTIs; dolutegravir, raltegravir) |
Dolutegravir: Substantially decreased dolutegravir concentrations and AUC; no apparent effect on etravirine1 Effect on dolutegravir pharmacokinetics is mitigated if etravirine and dolutegravir used concomitantly with lopinavir/ritonavir or ritonavir-boosted darunavir; effect expected to be mitigated if etravirine and dolutegravir used concomitantly with ritonavir-boosted atazanavir1 Raltegravir: Decreased raltegravir concentrations and AUC; no clinically important effect on etravirine pharmacokinetics1 No in vitro evidence of antagonistic antiretroviral effects1 |
Dolutegravir: Do not use etravirine and dolutegravir concomitantly unless ritonavir-boosted atazanavir, ritonavir-boosted darunavir, or lopinavir/ritonavir also included in the regimen1 Raltegravir: Dosage adjustments not needed1 |
|
HIV Nonnucleoside Reverse Transcriptase Inhibitors (NNRTIs; delavirdine, efavirenz, nevirapine, rilpivirine) |
Delavirdine: Possible increased etravirine concentrations1 Efavirenz: Possible decreased etravirine concentrations1 Nevirapine: Decreased etravirine concentrations and loss of antiretroviral efficacy1 Rilpivirine: Possible decreased rilpivirine concentrations; no change in etravirine concentrations1 |
Delavirdine: Do not use concomitantly1 Efavirenz: Do not use concomitantly1 Nevirapine: Do not use concomitantly1 Rilpivirine: Do not use concomitantly1 |
|
HIV Nucleoside and Nucleotide Reverse Transcriptase Inhibitors (NRTIs; didanosine, tenofovir) |
Didanosine: No effect on didanosine or etravirine concentrations1 Tenofovir: Decreased etravirine concentrations; no change in tenofovir concentrations1 |
Didanosine: Dosage adjustments not needed1 Tenofovir: Dosage adjustments not needed1 |
|
HIV Protease Inhibitors (atazanavir, darunavir, fosamprenavir, indinavir, lopinavir, nelfinavir, ritonavir, saquinavir, tipranavir) |
Atazanavir: Atazanavir or ritonavir-boosted atazanavir: Increased etravirine concentrations; decreased atazanavir concentrations and possible decreased antiretroviral efficacy1 No in vitro evidence of antagonistic antiretroviral effects1 Atazanavir/cobicistat: Potential loss of therapeutic effect and development of resistance to atazanavir1 Darunavir: Ritonavir-boosted darunavir: Decreased etravirine AUC; no change in darunavir concentrations; safety and efficacy of concomitant use established in phase 3 clinical studies1 2 3 No in vitro evidence of antagonistic antiretroviral effects1 Darunavir/cobicistat: Potential loss of therapeutic effect and development of resistance to darunavir1 Fosamprenavir: Fosamprenavir or ritonavir-boosted fosamprenavir: Substantially increased concentrations of amprenavir (active metabolite of fosamprenavir)1 No in vitro evidence of antagonistic antiretroviral effects1 Indinavir: Indinavir (without low-dose ritonavir): Possible decreased indinavir concentrations1 No in vitro evidence of antagonistic antiretroviral effects1 Lopinavir/ritonavir: Decreased etravirine concentrations and AUC; decreased lopinavir concentrations and AUC1 No in vitro evidence of antagonistic antiretroviral effects1 Nelfinavir: Nelfinavir (without low-dose ritonavir): Possible increased nelfinavir concentrations1 No in vitro evidence of antagonistic antiretroviral effects1 Ritonavir: Full-dose ritonavir (600 mg twice daily): Substantial decrease in etravirine concentrations and possible loss of antiretroviral efficacy1 Saquinavir: Ritonavir-boosted saquinavir: Decreased etravirine AUC; no change in saquinavir concentrations1 Decrease in systemic exposure to etravirine is similar to that in patients receiving etravirine in conjunction with ritonavir-boosted darunavir (a combination found to be safe and effective)1 No in vitro evidence of antagonistic antiretroviral effects1 Tipranavir: Ritonavir-boosted tipranavir: Decreased etravirine concentrations and possible decreased antiretroviral efficacy; increased tipranavir concentrations1 No in vitro evidence of antagonistic antiretroviral effects1 |
Atazanavir:Do not use concomitantly without low-dose ritonavir.1 Atazanavir/cobicistat: Do not use concomitantly with etravirine1 Darunavir: Ritonavir-boosted darunavir: Dosage adjustments not needed1 Darunavir/cobicistat: Do not use concomitantly with etravirine1 Fosamprenavir: Fosamprenavir (with or without low-dose ritonavir): Do not use concomitantly1 Indinavir: Do not use concomitantly without low-dose ritonavir1 Lopinavir/ritonavir: Because decrease in etravirine systemic exposure in patients receiving concomitant lopinavir/ritonavir is similar to that in patients receiving etravirine and concomitant ritonavir-boosted darunavir (a combination found to be safe and effective), manufacturer states that dosage adjustments not needed for either drug1 Nelfinavir: Do not use concomitantly with etravirine without low-dose ritonavir1 Ritonavir: Full-dose ritonavir (600 mg twice daily): Do not use concomitantly with etravirine1 Low-dose ritonavir (usually 100 mg once or twice daily): Etravirine may be used concomitantly with certain ritonavir-boosted PI regimens (i.e., ritonavir-boosted darunavir, lopinavir/ritonavir, ritonavir-boostedsaquinavir); concomitant use withritonavir-boosted fosamprenavir or ritonavir-boosted tipranavir not recommended1 Saquinavir: Ritonavir-boosted saquinavir: Dosage adjustments not needed1 Tipranavir: Ritonavir-boosted tipranavir: Do not use concomitantly1 |
|
Immunosuppressive agents (cyclosporine, sirolimus, tacrolimus) |
Potential for decreased immunosuppressive agent concentrations1 |
Use concomitantly with caution1 |
|
Lamivudine |
No in vitro evidence of antagonistic antiretroviral effects 1 |
|
|
Opiates and Opiate Partial Agonists (buprenorphine, buprenorphine/naloxone, methadone) |
Buprenorphine: Decreased buprenorphine concentrations and AUC; no effect on norbuprenorphine or etravirine concentrations1 Methadone: No clinically important change in methadone or etravirine concentrations1 |
Buprenorphine: Routine buprenorphine or buprenorphine/naloxone dosage adjustments not needed; monitor for withdrawal symptoms since buprenorphine or buprenorphine/naloxone maintenance dosage adjustment may be needed in some patients1 Methadone: Dosage adjustments not needed; monitoring for withdrawal symptoms is recommended as methadone maintenance therapy may need to be adjusted in some patients1 |
|
Paroxetine |
No change in etravirine or paroxetine concentrations1 |
Dosage adjustments not needed1 |
|
Proton pump inhibitors |
Omeprazole: Increased etravirine concentrations1 |
Omeprazole: Dosage adjustments not needed1 |
|
Sildenafil |
Decreased sildenafil concentrations1 |
Usual etravirine and sildenafil dosages can be used; sildenafil dosage may need to be increased based on clinical effect1 |
|
St. John’s wort (Hypericum perforatum) |
Possible substantially decreased etravirine concentrations and loss of antiretroviral efficacy1 |
Concomitant use not recommended1 |
|
Tadalafil |
Possible pharmacokinetic interaction with tadalafil1 |
No recommendations at this time1 |
|
Vardenafil |
Possible pharmacokinetic interaction with vardenafil1 |
No recommendations at this time1 |
|
Zidovudine |
No in vitro evidence of antagonistic antiretroviral effects1 |
Etravirine Pharmacokinetics
Absorption
Bioavailability
Absolute oral bioavailability is unknown.1
Following oral administration in adults, peak plasma concentrations attained within approximately 2.5–4 hours.1 11
Food
Systemic exposure is decreased by about 50% if etravirine is administered under fasting conditions compared with administration after a meal.1 11
Effect of food on etravirine bioavailability was studied using various meals (standard, light, enhanced-fiber, high-fat);11 magnitude of the food effect is similar with all meal types.1 11
Distribution
Extent
Distribution into compartments other than plasma (e.g., CSF, genital tract secretions) not evaluated.1
Crosses the placenta and has been detected in cord blood.202
Distributed into human milk.1
Plasma Protein Binding
99.9%, principally albumin and alpha 1-acid glycoprotein.1
Elimination
Metabolism
Metabolized principally in the liver by CYP isoenzymes 3A, 2C9, and 2C19.1
In cell culture, the major metabolites are at least 90% less active than etravirine against wild-type HIV-1.1
Elimination Route
Following oral administration of a single dose in adults, the majority (93.7%) is eliminated in feces as unchanged etravirine (81.2–86.4%).1 Up to 1.2% of the dose is eliminated in urine as metabolites.1
Unlikely to be removed by hemodialysis or peritoneal dialysis.1
Half-life
Mean terminal elimination half-life in adults is about 41 hours.1
Special Populations
Renal impairment: Pharmacokinetics not studied; alterations not expected because renal clearance is minimal.1
Hepatic impairment: Pharmacokinetics not altered in patients with mild or moderate hepatic impairment (Child-Pugh class A or B);1 12 not studied in patients with severe hepatic impairment (Child-Pugh class C).1
HIV-infected individuals coinfected with HBV and/or HCV: Reduced clearance reported.1
Geriatric individuals: Studies in those up to 77 years of age indicate no substantial differences in pharmacokinetics relative to younger adults.1
Pediatric patients 2 years to <18 years of age weighing ≥10 kg: Weight-based dosage results in systemic etravirine exposures similar to those reported in adults receiving 200 mg twice daily.1
Pregnant patients: Pharmacokinetics not studied.1
Stability
Storage
Oral
Tablets
25°C (excursions permitted between 15–30°C).1 Store in tight, closed container; protect from moisture.1 Dispense and store in original container; do not remove desiccant from bottle.1
Actions and Spectrum
-
Inhibits replication of HIV-1 by interfering with viral RNA- and DNA-directed polymerase activities of reverse transcriptase.1 4
-
Highly active against wild-type HIV-1; active against some clinical HIV-1 isolates resistant to some other NNRTIs (delavirdine, efavirenz, nevirapine).1 3 4 200
-
Different resistance profile than other NNRTIs; certain single mutations that result in class resistance to other NNRTIs may not necessarily result in etravirine resistance.2 3 4
-
Cross-resistance may occur between etravirine and other commercially available NNRTIs (delavirdine, etravirine, nevirapine, rilpivirine), and is expected in patients who have virologic failure while receiving a regimen that contains etravirine.1
Advice to Patients
-
Advise patients of the critical nature of compliance with human immunodeficiency virus (HIV) therapy and importance of remaining under the care of a clinician.1 Inform patients of the importance of taking as prescribed; do not alter or discontinue antiretroviral regimen without consulting a clinician.1
-
Advise patients of the importance of using etravirine in conjunction with other antiretrovirals and to not use for monotherapy.1
-
Advise patients of the importance of taking etravirine twice daily after a meal on a regular dosing schedule.1 Food enhances absorption of the drug; magnitude of the food effect is similar with all meal types (standard, light, enhanced-fiber, high-fat).1
-
Advise patients to swallow the tablets whole with liquid (e.g., water) without chewing.1 Patients unable to swallow tablets whole may disperse the tablets in 5 mL (1 teaspoon) of water (enough to cover the tablets); after dispersion in water, orange juice, milk, or water (approximately 15 mL, 1 tablespoon) may be added to the mixture.1 Ingest the liquid containing the dispersed etravirine tablets immediately, then rinse the glass several times with water, orange juice, or milk and drink the rinse each time to ensure that the entire dose is ingested.1 Warm water (greater than 40°C) or carbonated beverages should not be used.1
-
Inform patients that if a missed dose is remembered within 6 hours of the usually scheduled time, it should be taken after a meal as soon as possible and the next dose taken at the regularly scheduled time.1 If the missed dose is remembered more than 6 hours after the scheduled time, the dose should be omitted and the next dose taken at the regularly scheduled time.1
-
Advise patients that a severe and potentially life-threatening rash has occurred (usually within the first few weeks of etravirine therapy).1 Advise patients on the importance of immediately contacting clinician if rash occurs.1 Advise patients on the importance of immediately discontinuing etravirine and seeking medical care if rash associated with systemic symptoms (e.g., fever, generally ill feeling, extreme tiredness, muscle or joint aches, blisters, oral lesions, eye inflammation, swelling of the face, eyes, lips, or mouth, breathing difficulties, yellowing of the eyes or skin, dark or tea colored urine, pale colored stools, nausea, vomiting, loss of appetite, or right upper quadrant tenderness/pain) occurs.1
-
Inform patients that redistribution/accumulation of body fat may occur, with as yet unknown long-term health effects.1
-
Advise patients to inform their healthcare provider immediately of any symptoms of infection, since in some patients with advanced HIV infection, signs and symptoms of inflammation from previous infections may occur soon after anti-HIV treatment is started.1
-
Advise patients to inform their clinician of existing or contemplated concomitant therapy, including prescription and OTC drugs and herbal supplements (e.g., St. John’s wort), as well as any concomitant illnesses.1
-
Advise women to inform their clinician if they are or plan to become pregnant or plan to breast-feed.1
-
Advise patients of other important precautionary information.1
Additional Information
The American Society of Health-System Pharmacists, Inc. represents that the information provided in the accompanying monograph was formulated with a reasonable standard of care, and in conformity with professional standards in the field. Readers are advised that decisions regarding use of drugs are complex medical decisions requiring the independent, informed decision of an appropriate health care professional, and that the information contained in the monograph is provided for informational purposes only. The manufacturer’s labeling should be consulted for more detailed information. The American Society of Health-System Pharmacists, Inc. does not endorse or recommend the use of any drug. The information contained in the monograph is not a substitute for medical care.
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
* available from one or more manufacturer, distributor, and/or repackager by generic (nonproprietary) name
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Tablets |
25 mg* |
Etravirine Tablets |
|
|
Intelence |
Janssen |
|||
|
100 mg* |
Etravirine Tablets |
|||
|
Intelence |
Janssen |
|||
|
200 mg* |
Etravirine Tablets |
|||
|
Intelence |
Janssen |
AHFS DI Essentials™. © Copyright 2025, Selected Revisions February 10, 2025. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
† Off-label: Use is not currently included in the labeling approved by the US Food and Drug Administration.
References
1. Janssen. Intelence (etravirine) tablets prescribing information. Titusville, NJ; 2023 Mar.
2. Madruga JV, Cahn P, Grinsztejn B et al. Efficacy and safety of TMC125 (etravirine) in treatment-experienced HIV-1 infected patients in DUET-1: 24-week results from a randomised, double-blind, placebo-controlled trial. Lancet. 2007; 370:29-38. https://pubmed.ncbi.nlm.nih.gov/17617270
3. Lazzarin A, Campbell T, Clotet B et al. Efficacy and safety of TMC125 (etravirine) in treatment-experienced HIV-1 infected patients in DUET-2: 24-week results from a randomised, double-blind, placebo-controlled trial. Lancet. 2007; 370:39-48. https://pubmed.ncbi.nlm.nih.gov/17617271
4. Vingerhoets J, Azijn H, Fransen E et al. TMC125 displays a high genetic barrier to the development of resistance: evidence from in vitro selection experiments. J Virol. 2005; 79:12773-82. https://pubmed.ncbi.nlm.nih.gov/16188980
8. Schöller-Gyüre M, van den Brink W, Kakuda TN et al. Pharmacokinetic and pharmacodynamic study of the concomitant administration of methadone and TMC125 in HIV-negative volunteers. J Clin Pharmacol. 2008; 48:322-9.
11. Schöller-Gyüre M, Boffito M, Pozniak AL et al. Effects of different meal compositions and fasted state on the oral bioavailability of etravirine. Pharmacotherapy. 2008; 28:1215-22. https://pubmed.ncbi.nlm.nih.gov/18823217
12. Schöller-Gyüre M, Kakuda TN, De Smedt G et al. Effects of hepatic impairment on the steady-state pharmacokinetics of etravirine 200 mg BID: an open-label, multiple-dose, controlled Phase I study in adults. Clin Ther. 2010; 32:328-37. https://pubmed.ncbi.nlm.nih.gov/20206790
199. Kuhar DT, Henderson DK, Struble KA et al. Updated US Public Health Service guidelines for the management of occupational exposures to human immunodeficiency virus and recommendations for postexposure prophylaxis. Infect Control Hosp Epidemiol. 2013; 34:875-92. https://pubmed.ncbi.nlm.nih.gov/23917901
200. Panel on Antiretroviral Guidelines for Adults and Adolescents, US Department of Health and Human Services (HHS). Guidelines for the use of antiretroviral agents in HIV-1-infected adults and adolescents (March 23, 2023). Updates may be available at HIV.gov website. https://clinicalinfo.hiv.gov/en/guidelines
201. Panel on Antiretroviral Therapy and Medical Management of HIV-infected Children, US Department of Health and Human Services (HHS). Guidelines for the use of antiretroviral agents in pediatric HIV infection (April 11, 2023). Updates may be available at HIV.gov website. https://clinicalinfo.hiv.gov/en/guidelines
202. Panel on Treatment of HIV-Infected Pregnant Women and Prevention of Perinatal Transmission, US Department of Health and Human Services (HHS). Recommendations for use of antiretroviral drugs in pregnant HIV-1-infected women for maternal health and interventions to reduce perinatal HIV transmission in the United States (January 31, 2023). Updates may be available at HIV.gov website. https://clinicalinfo.hiv.gov/en/guidelines
300. Katlama C, Haubrich R, Lalezari J, et al. Efficacy and safety of etravirine in treatment-experienced, HIV-1 patients: pooled 48 week analysis of two randomized, controlled trials. AIDS. 2009;23:2289-2300.
301. Katlama C, Clotet B, Mills A, et al. Efficacy and safety of etravirine at week 96 in treatment-experienced HIV type-1-infected patients in the DUET-1 and DUET-2 trials. Antivir Ther. 2010;15:1045-1052.
302. Tudor-Williams G, Cahn P, Chokephaibulkit K, et al. Etravirine in treatment-experienced, HIV-1 infected children and adolescents: 48-week safety, efficacy and resistance analysis of the phase II PIANO study. HIV Med. 2014;15:513-524.
303. MacBrayne C, Rutstein R, Wiznia A, et al. Etravirine in treatment-experienced HIV-infected children 1 year to less than 6 years of age. AIDS. 2021;35:1413-1421.
304. Institute for Safe Medication Practices. ISMP list of error-prone abbreviations, symbols, and dose designations. 2024.
Related/similar drugs
Frequently asked questions
More about etravirine
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (2)
- Drug images
- Side effects
- Dosage information
- During pregnancy
- Drug class: NNRTIs
- Breastfeeding
- En español