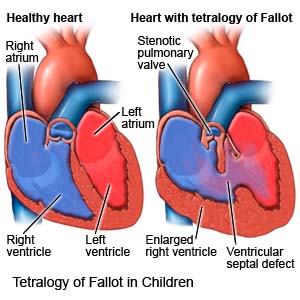
Tetralogy of Fallot in Children
Medically reviewed by Drugs.com. Last updated on Jun 30, 2025.
What is tetralogy of Fallot?
Tetralogy of Fallot (TOF) is a heart condition your child was born with. TOF causes the following 4 heart structure defects that lead to a weak heart and decreased blood flow:
- A narrowed blood vessel that connects the heart to the lungs
- A hole in the wall that separates the heart
- Aorta (major artery) growth from both sides of the heart instead of from one side as normal
- Blood flow that backs up and causes the right side of the heart to enlarge and thicken
 |
What increases my child's risk for TOF?
The cause of TOF is unknown. Any of the following may increase your child's risk:
- Maternal age older than 40
- A parent with TOF
- A viral illness in the mother during pregnancy
- Alcohol abuse during pregnancy
- Poor nutrition during pregnancy
What are the signs and symptoms of TOF?
- Blue coloration of the skin, lips, and nailbeds
- Poor appetite, slow growth, or problems putting on weight
- Clubbing (abnormal rounded shape) of fingertips and nails
- Tires easily or feels tired more than usual
- Sudden shortness of breath and fast breathing during feedings
- Fainting
- Fussy and irritable
- Heart murmur
How is TOF diagnosed?
- Blood tests show how much oxygen is flowing through your child's blood.
- An EKG test records your child's heart rhythm and how fast his or her heart beats. It is used to check for heart enlargement and other problems with blood flow.
- A chest x-ray: may show the shape of your child's heart and any enlargement from his or her condition.
- An echocardiogram is a type of ultrasound. Sound waves are used to show the structure and function of your child's heart.
- A Doppler test checks the blood flow in your child's heart. A small metal disc with gel is placed on your child's chest. Abnormal sounds may be heard when TOF is present.
- A cardiac catheterization may show the blood vessels in your child's heart and how well the heart is working. A catheter is threaded into your child's heart through a blood vessel in his or her arm, leg, or neck. Contrast dye is injected into an artery and x-rays of your child's blood flow are taken. Tell a healthcare provider if your child has ever had an allergic reaction to contrast dye.
How is TOF treated?
- Medicines can help your child's heart beat strongly and regularly or help get rid of extra fluid.
- Surgery may be needed between ages 3 to 6 months to correct the 4 heart defects. This will improve blood flow from your child's heart and lungs to his or her body.
How can I manage my child's symptoms?
- Place your child on his or her side and pull his or her knees up to his or her chest if he or she turns blue. This will help increase blood flow to his or her lungs.
- Keep your child's gums and teeth clean and healthy. Brush your child's gums or teeth regularly. Ask if your child needs antibiotics when he or she gets his or her teeth cleaned.
- Do not smoke around your child. If you smoke, it is never too late to quit. Smoke can harm your child's heart and lungs and make it hard for him or her to breathe. Ask for information if you need help quitting.
- Have your child vaccinated to help protect him or her against infections caused by viruses or bacteria. Ask for more information about vaccinations for your child.
Call your local emergency number (911 in the US) if:
- Your child has sudden trouble breathing.
- Your child has a seizure.
When should I seek immediate care?
- Your child faints.
- Your child's lips or fingernails are blue or white.
When should I call my child's doctor?
- Your child has a fever.
- Your child's signs and symptoms get worse.
- Your child is unusually fussy or irritable.
- Your child has weakness.
- You have questions or concerns about your child's condition or care.
Care Agreement
You have the right to help plan your child's care. Learn about your child's health condition and how it may be treated. Discuss treatment options with your child's healthcare providers to decide what care you want for your child. The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
Learn more about Tetralogy of Fallot
- Atorvastatin (Lipitor): Top 12 Drug Facts You Need to Know
- Do blood pressure drugs interact with alcohol?
- Side Effects of Weight Loss Drugs
Treatment options
Care guides
Medicine.com guides (external)
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
