Retinal Detachment
Medically reviewed by Drugs.com. Last updated on Aug 4, 2025.
What is retinal detachment?
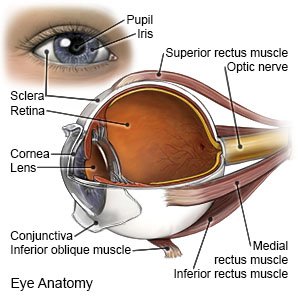
Retinal detachment is when your retina separates from the back of your eye. The retina is the thin layer of tissue that lines the back of your eye. It captures light and sends messages to the brain. Retinal detachment usually happens in 1 eye but may happen in both.
 |
What causes retinal detachment?
Retinal detachment is caused by fluid that builds up between your retina and your eye. This causes your retina to separate from the back of your eye. Your risk for retinal detachment may increase if you have any of the following:
- A personal or family history of retinal detachment
- Trouble seeing far way (nearsightedness)
- Eye surgery, such as cataract removal
- An eye injury such as a tear or hole in the retina
- An eye infection
- An eye disease, such as glaucoma
- Diabetic retinopathy or eye cancer
What are the symptoms of retinal detachment?
Symptoms usually happen suddenly. You may have any of the following:
- Seeing floaters, such as spots, cobwebs, strings, or specks
- Seeing flashes of light
- A dark or blind spot in the center of your vision
Related medications
Treatment options
The following list of medications are related to or used in the treatment of this condition.
How is retinal detachment diagnosed and treated?
Your healthcare provider will examine your eye. The provider may test your vision by asking you to read letters off a chart. You may need an ultrasound if your healthcare provider cannot see inside your eye well. Retinal detachment is often treated immediately with surgery to reattach your retina. Many types of surgery for retinal detachment are available. Talk to your healthcare provider about which eye surgery is right for you.
What can I do to protect my vision?
- Get an eye exam as often as directed. Eye exams are done to check for or monitor diabetic retinopathy or other problems. Early diagnosis and treatment of eye problems may prevent permanent vision damage.
- Manage health conditions that can cause vision problems. Common examples include diabetes, high blood pressure, and high cholesterol. Follow up with healthcare providers who manage these conditions.
- Wear sunglasses with ultraviolet (UV) light protection. UV light from the sun can damage your eyes. It can increase your risk for vision loss.
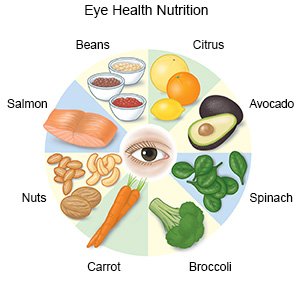
- Eat foods that contain eye-healthy nutrients. Healthy nutrients include vitamin A, vitamin C, vitamin E, omega-3 fatty acids, lutein, and zeaxanthin. They can be found in foods such as spinach, peanuts, salmon, collard greens, avocados, squash, eggs, and blueberries. Ask your healthcare provider for a full list of foods that contain eye-healthy nutrients. You may also need to take a vitamin or supplement to help you get enough of these nutrients.
- Exercise as directed. Ask your healthcare provider about the best exercise plan for you.

- Do not smoke. Nicotine can damage blood vessels in your eyes. Do not use e-cigarettes or smokeless tobacco in place of cigarettes or to help you quit. They still contain nicotine. Ask your healthcare provider for information if you currently smoke and need help to quit.
When should I call my doctor?
- You have a sudden change in your vision or loss of vision.
- You have eye pain.
- You see more floaters or flashes of light than usual.
- You have questions or concerns about your condition or care.
Care Agreement
You have the right to help plan your care. Learn about your health condition and how it may be treated. Discuss treatment options with your healthcare providers to decide what care you want to receive. You always have the right to refuse treatment. The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
Learn more about Retinal Detachment
Treatment options
Care guides
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
