Hepatitis A
Medically reviewed by Drugs.com. Last updated on Aug 4, 2025.
What is hepatitis A?
Hepatitis A is inflammation of the liver caused by hepatitis A virus (HAV) infection. HAV is most often spread through contaminated food or water, or close contact with someone who is infected. HAV infection can be prevented with 2 or 3 doses of the hepatitis A vaccine. The vaccine must be given before you are infected with HAV. You can get the vaccine as an adult if you did not get it as a child. Your healthcare provider can give you more information. He or she can tell you when to get the vaccine, and how many doses to get.
 |
What are the signs and symptoms of hepatitis A?
You may have no symptoms. Symptoms usually begin between 28 to 30 days after exposure to HAV, but it may be up to 50 days. You may have the following signs and symptoms:
- Low fever, usually under 100.4°F (38°C)
- Dark urine or pale bowel movements
- Fatigue
- Nausea, vomiting, or loss of appetite
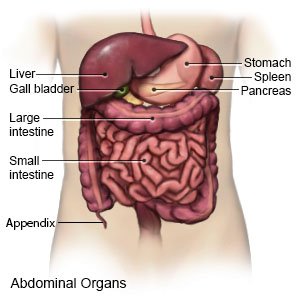
- Pain in the right upper side of your abdomen
- Jaundice (yellow skin and eyes) and itchy skin
How is hepatitis A diagnosed?
Your healthcare provider will ask about your signs and symptoms and any health problems you have. Tell him or her if you have hepatitis B, hepatitis C, or another liver disease. Tell your provider if you drink alcohol or use any illegal drugs. Blood tests are used to show if you are infected with HAV and to check your liver function.
How is hepatitis A treated?
Usually you will be treated at home. Medicine may not be needed. If you vomit a lot, you may need to go to the hospital to get fluids through an IV. Rest and healthy food will help you get better.
Treatment options
The following list of medications are related to or used in the treatment of this condition.
What can I do to manage hepatitis A?
- Eat a variety of healthy foods. Healthy foods include fruits, vegetables, whole-grain breads, low-fat dairy products, and lean meats and fish. Your healthcare provider or dietitian may recommend that you limit protein foods such as milk, fish, meat, and fatty foods. Protein and fat make your liver work harder. As you feel better, you can add other kinds of foods.

- Do not drink alcohol. Alcohol can increase liver damage. Talk to your healthcare provider if you drink alcohol and need help to stop.
- Drink more liquids. Liquids help your liver function properly. Ask your healthcare provider how much liquid to drink each day and which liquids are best for you.
- Get more rest. Rest if you are tired. Slowly return to your normal activities when you feel better.
How is HAV spread?
- Food handlers with HAV did not wash their hands after they used the bathroom.
- Drinking water that was not clean or eating raw shellfish that came from water that was not clean.
- Travel to areas in the world where hepatitis A is common or has an active outbreak.
- Daycare workers did not wash their hands after they changed a diaper.
- Sexual contact with someone who has hepatitis A, especially men who have sex with other men.
How can I prevent the spread of HAV?
You are most contagious in the 2 weeks before and the first week after you become jaundiced. Your friends, sex partners, and family members may need to get the hepatitis A vaccine. If you already have hepatitis A, it is too late to get the vaccine. The following are important things you can do to keep from spreading the infection:
- Do not share dishes or utensils. Soak dishes and utensils in boiling water. Then wash them, or use a dishwasher. You may want to use disposable dishes.
- Do not prepare food or meals for other people.
- Wash clothing and bedding in the hottest water setting.
- Clean toilets with a product that kills germs.
- Let your healthcare provider know if your work involves preparing or serving food, or close physical contact with other people. If you do this kind of work, the health department will need to evaluate if these people have been exposed to hepatitis A. You cannot return to work until your healthcare provider says it is safe.
What can I do to prevent the spread of germs?
 |
- Wash your hands often. Wash your hands several times each day. Wash after you use the bathroom, change a child's diaper, and before you prepare or eat food. Use soap and water every time. Rub your soapy hands together, lacing your fingers. Wash the front and back of your hands, and in between your fingers. Use the fingers of one hand to scrub under the fingernails of the other hand. Wash for at least 20 seconds. Rinse with warm, running water for several seconds. Then dry your hands with a clean towel or paper towel. Use hand sanitizer that contains alcohol if soap and water are not available. Do not touch your eyes, nose, or mouth without washing your hands first.

- Cover a sneeze or cough. Use a tissue that covers your mouth and nose. Throw the tissue away in a trash can right away. Use the bend of your arm if a tissue is not available. Wash your hands well with soap and water or use a hand sanitizer.
- Stay away from others while you are sick. Avoid crowds as much as possible.
- Ask about vaccines you may need. Your healthcare provider can tell you if you should also get vaccines other than those listed below, and when to get them:
- COVID-19 vaccines are given to adults as a shot. At least 1 dose of an updated vaccine is recommended for all adults. COVID-19 vaccines are updated throughout the year. Adults 65 or older need a second dose of updated vaccine at least 4 months after the first dose. Your healthcare provider can help you schedule all needed doses as updated vaccines become available.
- Ask your healthcare provider about the flu and pneumonia vaccines. All adults should get the flu (influenza) vaccine as soon as recommended each year, usually in September or October. The pneumonia vaccine is recommended for all adults aged 50 or older to prevent pneumococcal disease, such as pneumonia. Adults aged 19 to 49 years who are at high risk for pneumococcal disease should also receive the vaccine. You may need 1 dose or 2. The number depends on the vaccine used and your risk factors.
When should I seek immediate care?
- You have severe abdominal pain.
- You are too dizzy to stand up.
- You vomit blood or material that looks like coffee grounds.
- Your bowel movements are red or black, and sticky.
- You feel confused, unusually sleepy, irritable, or jittery.
When should I call my doctor?
- You are vomiting and cannot keep food or liquids down.
- You are bruising easily.
- You have questions or concerns about your condition or care.
Care Agreement
You have the right to help plan your care. Learn about your health condition and how it may be treated. Discuss treatment options with your healthcare providers to decide what care you want to receive. You always have the right to refuse treatment. The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
Learn more about Hepatitis A
Treatment options
Care guides
Symptoms and treatments
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
