Tricuspid Valve Repair
Medically reviewed by Drugs.com. Last updated on Aug 4, 2025.
What do I need to know about tricuspid valve repair (TVR)?
TVR is surgery to repair a damaged or diseased tricuspid valve. Your valve may need to be replaced if your condition is severe.
 |
How do I prepare for TVR?
- Your surgeon will tell you how to prepare. Your surgeon may tell you not to eat or drink anything after midnight on the day of your surgery. Arrange to have someone drive you home when you are discharged.
- Tell your surgeon about all medicines you currently take. Your surgeon will tell you if you need to stop any medicine for the surgery, and when to stop. Your surgeon will tell you which medicines to take or not take on the day of surgery.
- Tell your surgeon about any allergies you have, including medicines or anesthesia. You may be given an antibiotic to help prevent a bacterial infection.
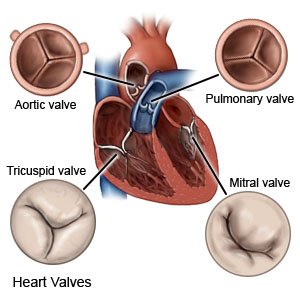
- You may need an echocardiogram (echo), EKG, or CT before your surgery. These tests will help your surgeon plan for your surgery. Your surgeon may also use an echo during surgery to check the valve and valve leaflets. Leaflets are flaps of tissue that should prevent blood from flowing backward through the valve.
Related medications
What will happen during TVR?
- You will be given general anesthesia to keep you asleep and free from pain during surgery. Your surgeon will make an incision in your chest. Your surgeon will cut or spread your ribcage apart to reach your heart. Your heart will be connected to a bypass machine. This machine pumps blood to your body and keeps blood out of your heart during surgery.
- You may need percutaneous (through the skin) surgery if you cannot have open-heart surgery. Your surgeon will insert a catheter (tube) into a vein in your groin or neck. The catheter will be guided to your heart. Your surgeon will repair your valve through the catheter.
- Your surgeon may sew a device in place to tighten or strengthen the annulus (ring of tissue) around the valve. Your surgeon may fix the leaflets with stitches. Your surgeon may guide a permanent device through the catheter. The device clips (holds) leaflets together to help them close properly. If your valve needs to be replaced, your surgeon may use a mechanical or tissue valve. A mechanical valve is made of strong materials. A tissue valve is made of tissue from an animal, such as a cow or pig.
- Your surgeon will remove the catheter and disconnect the bypass machine. Your incisions may be closed with stitches, staples, or other devices and covered with a bandage.
What should I expect after TVR?
- You will be taken to a recovery room until you are fully awake. Healthcare providers will monitor you closely for any problems. You will need to stay in the hospital for at least a few days, depending on your condition.
- You may need to lie flat for a few hours after surgery if your surgeon used a catheter in your groin. Talk to healthcare providers before you get up the first time. They may need to help you stand up safely. When you are able to get up on your own, sit or lie down right away if you feel weak or dizzy. Then press the call light button to let healthcare providers know you need help. You may need to hold a pillow against your incision when you move in and out of bed. This will help decrease pain.
What are the risks of TVR?
You may bleed more than expected or develop an infection. Parts of your heart may be damaged during surgery. Your repaired valve may stop working. You may need more surgery to fix or replace the valve. If a clip device was used, it may move out of place. The clip may not work properly, or it may stop working properly later. Your symptoms may return, even after surgery. You may develop heart failure. You may develop a blood clot or an irregular heartbeat. These can be life-threatening.
Care Agreement
You have the right to help plan your care. Learn about your health condition and how it may be treated. Discuss treatment options with your healthcare providers to decide what care you want to receive. You always have the right to refuse treatment. The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
