Ventriculoperitoneal Shunt Placement for Hydrocephalus in Adults
Medically reviewed by Drugs.com. Last updated on Jun 2, 2025.
What do I need to know about ventriculoperitoneal shunt placement?
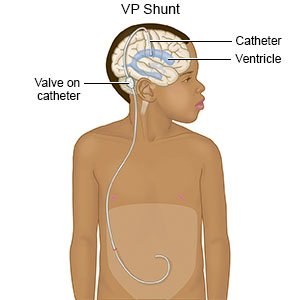
Ventriculoperitoneal (VP) shunt placement is surgery to help remove extra cerebrospinal fluid (CSF) in your brain.
 |
How do I prepare for surgery?
Your surgeon will talk to you about how to prepare for surgery. He or she may tell you not to eat or drink anything after midnight on the day of your surgery. He or she will tell you what medicines to take or not take on the day of your surgery. You may be given an antibiotic through your IV to help prevent a bacterial infection. Arrange to have someone drive you home and stay with you to make sure you are okay.
Related medications
Acetazolamide
Acetazolamide systemic is used for edema, epilepsy, glaucoma, hydrocephalus, hypokalemic periodic ...
What will happen during surgery?
- You will be given general anesthesia to keep you asleep and free from pain during surgery. Two small incisions will be made. One incision will be in your head and the other in your abdomen. One end of the shunt will be placed into your brain. This end of the shunt will be connected to a valve that controls the amount of CSF that goes through the shunt. You may need another incision behind your ear to create a pocket for the valve. Near the valve is a reservoir or pump. The pump can be pressed by the surgeon to check how the shunt is working.
- Connected to the valve on the shunt is a catheter (tube). This catheter is tunneled under your skin, from your head to your abdomen. The extra CSF will empty into your abdomen. It will be quickly absorbed into your blood. Your incisions may be closed with staples or stitches. Bandages may be placed over the incisions.
What will happen after surgery?
Providers will monitor you closely to make sure the shunt is working properly. Your intracranial pressure (ICP) will be checked. The ICP is the pressure inside your skull. Your provider may need to change the settings on your valve if your ICP is too high or too low. You may need imaging tests to check the placement of the shunt and make sure it is not blocked. A sample of your CSF may be tested to check for infection and inflammation.
What are the risks of surgery?
You may get a headache that is worse when you sit or stand. Your tube may become blocked or move out of place, and you may need another surgery. You could have bleeding into your brain and you may need surgery to treat it. You may get an infection at the incision site or a more serious infection in your brain. There may be damage to your brain or the organs in your abdomen.
Care Agreement
You have the right to help plan your care. Learn about your health condition and how it may be treated. Discuss treatment options with your healthcare providers to decide what care you want to receive. You always have the right to refuse treatment. The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
Learn more about Ventriculoperitoneal Shunt Placement for Hydrocephalus
Care guides
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
