Type 2 Diabetes in the Older Adult
Medically reviewed by Drugs.com. Last updated on Aug 4, 2025.
What do I need to know about type 2 diabetes?
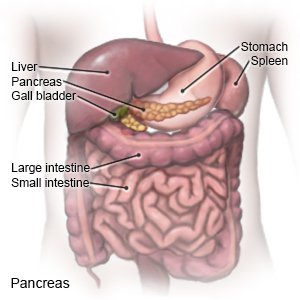
The risk for type 2 diabetes increases as you get older. When the blood sugar level increases, the pancreas should make more insulin. Insulin helps move sugar out of the blood so it can be used for energy. Type 2 diabetes means your pancreas does not make enough insulin, or your body does not use insulin well. Diabetes cannot be cured, but it can be managed.
 |
What is diabetes education?
Diabetes education will start right away, if the diagnosis is new. You may need diabetes education at a later time to refresh your memory. Your diabetes care team may include physicians, nurse practitioners, community health providers, and physician assistants. It may also include nurses, dietitians, exercise specialists, pharmacists, dentists, and podiatrists. Family members, or others who are close to you, may also be part of the team. You and your team will make goals and plans to manage diabetes and other health problems. The plans and goals will be specific to your needs. Members of your diabetes care team will teach you the following:
- About your blood sugar level: You will be given information on when and how to check your blood sugar level. Your healthcare provider will help you create a blood sugar level range. The goal is to keep your blood sugar within the range so it does not go too high or too low. Make a list of the times you checked your blood sugar level and the results of your checks. Take this to all follow-up appointments.
- A glucose meter is a device that uses a test strip to check the level. You put a small drop of blood from a finger on the test strip. The strip is put into the device. The device then figures out how much sugar is in your blood.

- A continuous glucose monitor (CGM) uses a sensor to check the level. The sensor is placed on your abdomen or arm. A transmitter on the sensor gets a glucose reading. CGM data may be linked to an insulin pump, if needed. The data will help you and your provider see how much time your blood sugar levels stayed in range. Your provider may recommend nutrition, physical activity, or medicine changes if your levels were often above or below range.

- A glucose meter is a device that uses a test strip to check the level. You put a small drop of blood from a finger on the test strip. The strip is put into the device. The device then figures out how much sugar is in your blood.
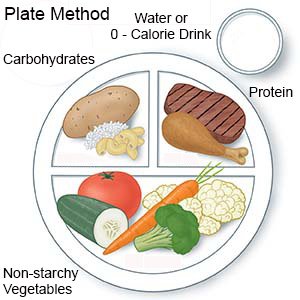
- About nutrition: A dietitian will help you make a meal plan to keep your blood sugar level steady. You will learn how food affects your blood sugar levels. You will also learn to keep track of carbohydrates (sugar and starchy foods). You will learn why it is important not to skip meals. You may develop hypoglycemia if you have taken diabetes medicine and do not eat. Hypoglycemia means your blood sugar level is too low. You may be taught the plate method for portion control. With the plate method, ½ of your plate contains non-starchy vegetables, ¼ contains protein, and ¼ contains carbohydrates. Your dietitian will give you examples of each kind of food to include. Ask your care team for more information about meal planning.
- About non-insulin diabetes medicines: These medicines help control your blood sugar level and may help you maintain a healthy weight. Most non-insulin medicines are taken by mouth. Some are injected daily or weekly. You may need more than 1 medicine, depending on your A1c results over time.
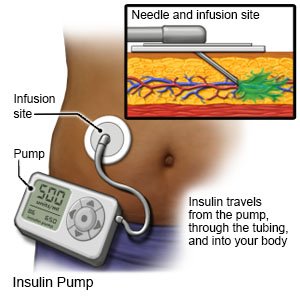
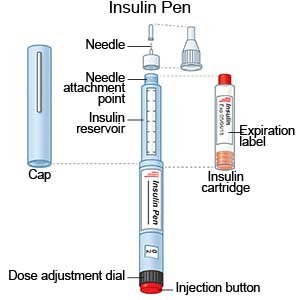
- About insulin: Insulin may be used or added if non-insulin diabetes medicine becomes less effective. You will learn how much insulin you need and when to use it. You will also be taught how to match insulin with blood sugar levels, activity, and carbohydrates. Insulin may be given through a pump or pen, or injected. You and your care team will discuss the best method for you:
- An insulin pump is a wearable medical device that gives continuous insulin. An insulin pump prevents the need for multiple insulin injections in a day.
- An insulin pen is a device prefilled with insulin. Most insulin pens are disposable. You throw the pen away after it is empty or used for a certain amount of time. Some pens have a replaceable cartridge filled with insulin. You keep the pen and only throw away the cartridge.
- Insulin injections are given with a needle and syringe. You and your family members will be taught how to draw up and give insulin if this is the best method for you. You will also be taught how to dispose of used needles and syringes.
- An insulin pump is a wearable medical device that gives continuous insulin. An insulin pump prevents the need for multiple insulin injections in a day.
- How to prevent complications (health problems): Diabetes that is not well controlled can lead to health problems. Examples include foot sores, retinopathy (vision loss), and peripheral neuropathy (loss of feeling in your hands and feet). Also, risk for dementia can increase with blood sugar levels that are too high or too low for long periods of time. Your team will help you know when to get regular checkups, such as vision checks. They will teach you how to watch for problems and when to get a problem checked.
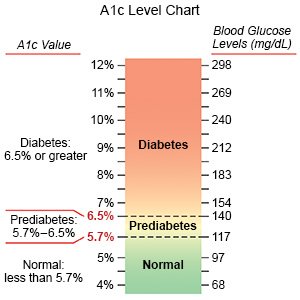
- About your A1c level: Your provider will check your A1c every 3 months, or 2 times each year if your diabetes is controlled. An A1c test shows the average amount of sugar in your blood over the past 2 to 3 months. Your provider will tell you what your A1c level should be.
What can I do to manage my blood sugar levels?
Sometimes type 2 diabetes can be managed with changes in nutrition and physical activity.
- Work with your diabetes care team to create plans to meet your needs. You and your team will make goals and plans to manage diabetes and other health problems. For example, the plan will include how to manage medicines you may take for diabetes and for other health conditions. The plans and goals will be specific to your needs and abilities. Your plan will change as your needs and abilities change. Tell your care team if you have trouble following any part of your care plan.
- Try to be physically active for 30 to 60 minutes most days of the week. Physical activity, such as exercise, helps keep your blood sugar level steady and lowers your risk for heart disease. Physical activity can also lower your risk for falls. Activity can be spread throughout the day. Try to get at least 10 minutes of activity at a time. Do not miss more than 2 days in a row. Your provider can help you create an activity plan:
- Set a goal for 30 minutes of aerobic activity at least 5 times a week. Aerobic activity helps your heart stay strong. Aerobic activity includes walking, bicycling, dancing, swimming, and raking leaves.

- Set a goal for strength training 2 times a week. Strength training helps you keep the muscles you have and build new muscles. Strength training includes lifting weights, climbing stairs, and doing yoga or tai chi.

- Stay steady on your feet with balancing activities. These include walking backwards, standing on one foot, and walking heel to toe in a straight line.
- Set a goal for 30 minutes of aerobic activity at least 5 times a week. Aerobic activity helps your heart stay strong. Aerobic activity includes walking, bicycling, dancing, swimming, and raking leaves.
- Maintain a healthy weight. Ask your team what a healthy weight is for you. A healthy weight can help you control diabetes and prevent heart disease. Ask your team to help you create a weight loss plan, if needed. Your team will help you set a weight-loss goal, such as 10 to 15 pounds, or 5% of your extra weight. Together you and your team can set manageable weight loss goals.
- Talk to your provider about weight loss medicines, if needed. These medicines are not used to lower blood sugar, but your level may decrease from weight loss. Your provider may recommend you continue taking the medicine even after you finish losing extra weight. Along with maintaining a healthy weight, these medicines can help protect your heart and kidneys.
- Know the risks if you choose to drink alcohol. Alcohol can cause your blood sugar level to be low if you use insulin. Alcohol can cause high blood sugar levels and weight gain if you drink too much. A drink of alcohol is 12 ounces of beer, 5 ounces of wine, or 1½ ounces of liquor. Your care team can tell you how many drinks are okay within 24 hours and within 1 week.
Treatment options
The following list of medications are related to or used in the treatment of this condition.
What else can I do to manage diabetes?
- Wear medical alert identification. Wear medical alert jewelry or carry a card that says you have type 2 diabetes. The identification should include any diabetes medicine you take. Ask your care team provider where to get these items.

- Do not smoke. Nicotine and other chemicals in cigarettes can cause lung disease and other health problems. It can also cause blood vessel damage that makes diabetes more difficult to manage. Ask your healthcare provider for information if you currently smoke and need help to quit. Do not use e-cigarettes or smokeless tobacco in place of cigarettes or to help you quit. They still contain nicotine.
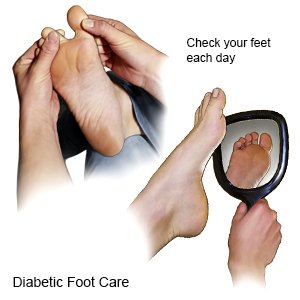
- Check your feet every day for sores. Look at your whole foot, including the bottom, and between and under your toes. Check for wounds, corns, and calluses. Use a mirror to see the bottom of your feet. The skin on your feet may be shiny, tight, dry, or darker than normal. Your feet may also be cold and pale. Feel your feet by running your hands along the tops, bottoms, sides, and between your toes. Redness, swelling, and warmth are signs of blood flow problems that can lead to a foot ulcer. Do not try to remove corns or calluses yourself. Work with a podiatrist or other care team provider who can help you with these problems. A podiatrist is a foot specialist.
- Manage other health issues as directed. Health issues may include high blood pressure, high cholesterol levels, and heart problems. Health issues may also include depression or anxiety. Together you and your care team can create a plan to manage any other health issues.
- Ask about vaccines you may need. You have a higher risk for serious illness if you get the flu, pneumonia, COVID-19, or hepatitis. Ask if you should get vaccines to prevent these or other diseases, and when to get the vaccines.
- Get help from family and friends. You may need help checking your blood sugar level, giving insulin injections, or preparing your meals. You may also need help to check your feet for sores. Talk to your care team if you need someone at home to help you.
- Go to all follow-up appointments. You may need tests to check for a low vitamin B level if you take oral diabetes medicine for a long time. Your provider may also check your cognitive (brain) function 1 time each year. Talk to your provider about all your medicines, including any that are not for diabetes. Your provider will check if a combination of your medicines could cause hypoglycemia.
- Eat high-fiber foods as directed. Fiber helps improve blood sugar levels. Fiber also lowers your risk for heart disease and other problems diabetes can cause. Examples of high-fiber foods include vegetables, whole-grain bread, and beans such as pinto beans. Your dietitian can tell you how much fiber to have each day.

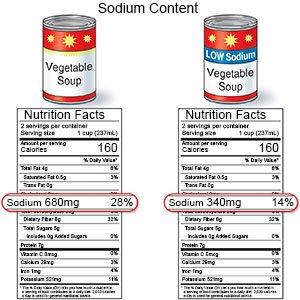
- Limit sodium (salt) as directed. Your dietitian may tell you to limit sodium to 2,300 milligrams (mg) each day. Your dietitian can help you create a meal plan that is low in sodium. If you use canned foods, choose low-sodium brands as often as possible. Do not add salt at the table if you add salt when you cook.
- Drink water throughout the day. Your dietitian may tell you to limit or avoid liquids that have artificial sweeteners. Water is the best liquid to drink.
Call your local emergency number (911 in the US) or have someone call if:
- You have any of the following signs of a stroke:
- Numbness or drooping on one side of your face
- Weakness in an arm or leg
- Confusion or difficulty speaking
- Dizziness, a severe headache, or vision loss
- You have any of the following signs of a heart attack:
- Squeezing, pressure, or pain in your chest
- You may also have any of the following:
- Discomfort or pain in your back, neck, jaw, stomach, or arm
- Shortness of breath
- Nausea or vomiting
- Lightheadedness or a sudden cold sweat
When should I seek immediate care?
- Your blood sugar level is higher than your goal and does not come down with treatment.
- You have blurred or double vision.
- You have signs of a high ketone level, such as fruity, sweet smelling breath, or shallow breathing.
- You have symptoms of a low blood sugar level, such as trouble thinking, sweating, or a pounding heartbeat.
- Your blood sugar level is lower than your goal and does not improve with treatment.
When should I call my doctor or diabetes care team provider?
- You are vomiting or have diarrhea.
- You have an upset stomach and cannot eat the foods on your meal plan.
- You feel weak or more tired than usual.
- You feel dizzy, have headaches, or are easily irritated.
- Your skin is red, warm, dry, or swollen.
- You have a wound that does not heal.
- You have numbness in your arms or legs.
- You have trouble coping with diabetes, or you feel anxious or depressed.
- You have memory problems.
- You have changes in your vision.
- You have questions or concerns about your condition or care.
Care Agreement
You have the right to help plan your care. Learn about your health condition and how it may be treated. Discuss treatment options with your healthcare providers to decide what care you want to receive. You always have the right to refuse treatment. The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
Learn more about Type 2 Diabetes
- Diabetes Medications and Alcohol Interactions
- FDA-Approved Weight Loss Drugs: Can They Help You?
- OneTouch Blood Glucose Meters
- Side Effects of Weight Loss Drugs
- Top 10 Diabetes Treatments You May Have Missed
- Which Drugs Cause Weight Gain?
Treatment options
Medicine.com guides (external)
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
