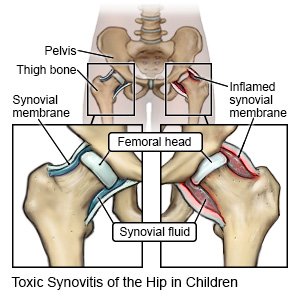
Toxic Synovitis of the Hip in Children
Medically reviewed by Drugs.com. Last updated on Aug 4, 2025.
What is toxic synovitis of the hip?
Toxic synovitis of the hip is swelling of your child's hip joint. The swelling usually develops after a viral infection or trauma and does not spread to other areas. Toxic synovitis of the hip can occur at any age but is most common in children 3 to 10 years old.
 |
What are the signs and symptoms of toxic synovitis of the hip?
- Sudden pain in the hip, upper leg, or knee
- Pain that causes your child to limp when he or she walks
- Limited leg and hip motion
- Sitting or lying with the legs apart in an unusual position
- A fever of 100ºF (37.78ºC) or lower
How is toxic synovitis of the hip diagnosed?
Your child's healthcare provider will examine your child's hip and leg to locate the pain. The provider may ask when your child's symptoms began. Your child's leg and hip movement will be checked. Any of the following tests may also be needed:
- Blood tests may show if an infection is causing your child's symptoms.
- MRI, x-ray, or ultrasound pictures may be taken to check your child's bones, joints, muscles, or blood vessels. Healthcare providers may also use the ultrasound to help find and remove fluid from the hip joint. Do not let your child enter the MRI room with anything metal. The MRI machine uses a powerful magnet. Metal can cause serious injury from the magnet. Tell the healthcare provider if your child has any metal in or on his or her body.
- A bone scan is used to take pictures of your child's bones. Your child is given a small, safe amount of radioactive dye in an IV. Healthcare providers can look at the pictures for broken bones, infection, or problems in the bones.
How is toxic synovitis of the hip treated?
Toxic synovitis may go away on its own within 3 weeks. The following can help you manage your child's condition:
- Rest and limited leg movement may help your child improve more quickly. Your child may also be told to keep weight off his or her leg until pain is reduced.
- Medicines may be needed to treat pain or a bacterial infection.
When should I seek immediate care?
- Your child's symptoms get worse.
- Your child cannot put any weight on his or her leg.
- Your child's fever is higher than 100ºF (37.8ºC), or as directed by a healthcare provider.
When should I call my child's doctor?
- Your child's symptoms do not improve within 3 weeks on their own, or within 2 days with medicine.
- You have questions or concerns about your child's condition or care.
Care Agreement
You have the right to help plan your child's care. Learn about your child's health condition and how it may be treated. Discuss treatment options with your child's healthcare providers to decide what care you want for your child. The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
