Stevens-Johnson Syndrome
Medically reviewed by Drugs.com. Last updated on Aug 4, 2025.
Stevens-Johnson syndrome (SJS) is a rare and serious condition of your skin and mucus membranes. SJS will cause you to lose up to 10% of your outer layer of skin. SJS is usually caused by a response to a medicine you have been taking. The most common medicines are antibiotics, NSAIDs, and antiseizure medicines. The response may happen 1 week to 2 months after you take the medicine. SJS may also be caused by infection, vaccinations, or diseases involving your organs or whole body.
WHILE YOU ARE HERE:
Informed consent
is a legal document that explains the tests, treatments, or procedures that you may need. Informed consent means you understand what will be done and can make decisions about what you want. You give your permission when you sign the consent form. You can have someone sign this form for you if you are not able to sign it. You have the right to understand your medical care in words you know. Before you sign the consent form, understand the risks and benefits of what will be done. Make sure all your questions are answered.
An IV
is a small tube placed in your vein that is used to give you medicine or liquids.
A Foley catheter
is a tube put into your bladder to drain urine into a bag. Keep the bag below your waist. This will prevent urine from flowing back into your bladder and causing an infection or other problems. Also, keep the tube free of kinks so the urine will drain properly. Do not pull on the catheter. This can cause pain and bleeding, and may cause the catheter to come out.
A ventilator
is a machine that gives you oxygen and breathes for you when you cannot breathe well on your own. An endotracheal (ET) tube is put into your mouth or nose and attached to the ventilator. You may need a trach if an ET tube cannot be placed. A trach is a tube put through an incision and into your windpipe.
Air bed:
You may be placed on an air-fluidized bed to decrease further injury to your skin. An air-fluidized bed has warm air that moves around inside the mattress. The moving air feels like fluid movement.
Intake and output:
The amount of liquid you are getting and urinating will be tracked. Ask how much liquid you should drink each day. Ask if your urine needs to be measured or collected.
Mouth care:
Clean your mouth as shown by your healthcare provider. You may need to use a special toothbrush or swab to clean your mouth. You may also need to rinse your mouth with a medicated mouthwash to help prevent infection. Lip protectant may also be used to protect your lips and help them heal.
Nasogastric (NG) tube:
An NG tube is put into your nose and passed down your throat until it reaches your stomach. Food and medicine may be given through an NG tube if you cannot swallow. The tube may instead be attached to suction if your stomach needs to be kept empty.
Medicines:
- Antacids may be needed if sores grow in your stomach and cause bleeding.
- Antibiotics may be given to help treat an infection in your blood. Antibiotics may also be put on your skin to lower your risk for infection.
- Blood thinners help stop clots from forming in your blood if you are not able to get out of bed.
- Eye drops may be used to help eye sores heal and prevent infection.
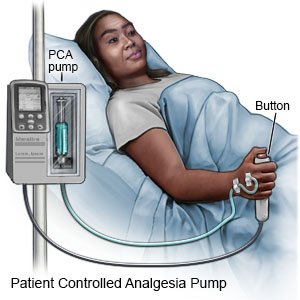
- Pain medicines may be given. You may get pain medicine from a pump called patient-controlled analgesia (PCA). The PCA will give you small amounts of pain medicine through your IV. The pump also has a cord with a push button on the end. When you feel pain and push the button, you will give yourself pain medicine. There is a limit on how much medicine you can give yourself.
- Immune globulins may be given to make your immune system stronger. You may need immune globulins to treat or prevent an infection.
- Pressors may be given to increase your blood pressure. A normal blood pressure helps protect your heart, lungs, brain, kidneys, and other organs.
Treatment options
The following list of medications are related to or used in the treatment of this condition.
Tests:
- A chest x-ray may be done to check for an infection in your heart or lungs.
- Eye exams may be done to check your vision and help prevent long-term problems from sores in your eyes.
- A wound culture is done to check for a skin infection. A swab is used to collect fluid from a sore and then sent for testing.
Treatments:
- TPN is liquid nutrition that provides your body with protein, sugar, vitamins, minerals, and sometimes fat (lipids). TPN is used when you have problems with eating or digesting food.
- Wound care is done to protect skin sores and help them heal.
- Hydrotherapy is done in a whirlpool to help clean your wounds, and to remove dead tissue from your skin.
- Physical therapy may be needed to help your arm and leg movement if you have to stay in bed.
- Surgery may be needed if your skin does not heal properly. You may need debridement to clean the wounds and to remove dirt or dead tissues. A skin graft may be done to cover and to help heal the areas where you lost skin.
RISKS:
Your skin may heal with or without scars. Healed skin may have color changes. You may lose your nails and hair for your lifetime. You may have lifelong problems swallowing, and difficulty urinating. SJS may also cause you to have lifelong skin, vision, and medical problems. You may die. Death is usually caused by infection, lung problems, or other serious problems.
CARE AGREEMENT:
You have the right to help plan your care. Learn about your health condition and how it may be treated. Discuss treatment options with your healthcare providers to decide what care you want to receive. You always have the right to refuse treatment.© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.
Learn more about Stevens-Johnson Syndrome
Treatment options
Care guides
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
