Seizures after Traumatic Brain Injury
Medically reviewed by Drugs.com. Last updated on Aug 4, 2025.
You are at higher risk for a seizure after a TBI. A seizure is an episode of abnormal brain activity. A seizure may happen within hours after your TBI or weeks to years later. Late posttraumatic seizures increase your risk for developing epilepsy. Epilepsy is a brain disorder that causes repeated seizures. You can take steps to stay safe and prevent another seizure.
DISCHARGE INSTRUCTIONS:
Call 911 or have someone else call for any of the following:
- Your seizure lasts longer than 5 minutes.
- You have a second seizure within 24 hours of the first.
- You have trouble breathing after a seizure.
- You cannot be woken after your seizure.
- You have more than 1 seizure before you are fully awake or aware.
Seek care immediately if:
- You are injured during a seizure.
Contact your healthcare provider if:
- You have a fever.
- You start to have seizures more often.
- You have questions or concerns about your condition or care.
Medicines:
You may be given the following:
- Antiseizure medicine may control or prevent another seizure. Do not stop taking this medicine unless directed by a healthcare provider. You may need blood tests to check the level of medicine in your blood. Your healthcare provider may need to change or adjust your medicine.
- Take your medicine as directed. Contact your healthcare provider if you think your medicine is not helping or if you have side effects. Tell your provider if you are allergic to any medicine. Keep a list of the medicines, vitamins, and herbs you take. Include the amounts, and when and why you take them. Bring the list or the pill bottles to follow-up visits. Carry your medicine list with you in case of an emergency.
What you can do to manage or prevent a seizure:
- Set a regular sleep schedule. A lack of sleep can trigger a seizure. Try to go to sleep and wake up at the same times every day. Keep your bedroom quiet and dark. Talk to your healthcare provider if you are having trouble sleeping.
- Limit or do not drink alcohol as directed. Alcohol can trigger a seizure, especially if you drink a large amount at one time. A drink of alcohol is 12 ounces of beer, 1½ ounces of liquor, or 5 ounces of wine. Talk to your healthcare provider about a safe amount of alcohol for you. Your provider may recommend that you do not drink any alcohol. Tell him or her if you need help to quit drinking.
- Ask what safety precautions you should take. Talk with your healthcare provider about driving. You may not be able to drive until you are seizure-free for a period of time. You will need to check the law where you live. Also talk to your healthcare provider about swimming and bathing. You may drown or develop life-threatening heart or lung damage if you have a seizure in water.
- Tell your friends, family members, and coworkers that you had a seizure. Give them written instructions to follow if you have another seizure.
What others can do to keep you safe during a seizure:
Give the following instructions to family, friends, and coworkers:
- Do not panic.
- Gently guide me to the floor or a soft surface.
- Do not hold me down or put anything in my mouth.
- Place me on my side to help prevent me from swallowing saliva or vomit.
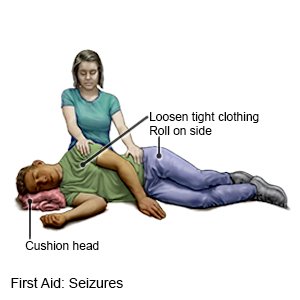
- Protect me from injury. Remove sharp or hard objects from the area surrounding me, or cushion my head.
- Loosen the clothing around my head and neck.
- Time how long my seizure lasts. Call 911 if my seizure lasts longer than 5 minutes or if I have a second seizure.
- Stay with me until my seizure ends. Let me rest until I am fully awake.
- Perform CPR if I stop breathing or you cannot feel my pulse.
- Do not give me anything to eat or drink until I am fully awake.
Follow up with your healthcare provider or neurologist as directed:
Write down your questions so you remember to ask them during your visits.
© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.
Learn more about Seizures after Traumatic Brain Injury
Care guides
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
