Roux-En-Y Gastric Bypass
Medically reviewed by Drugs.com. Last updated on Apr 2, 2024.
What do I need to know about roux-en-Y gastric bypass surgery?
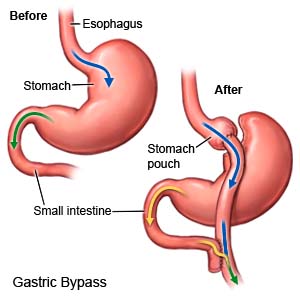
Roux-en-Y gastric bypass is a type of weight loss surgery. Staples are used to make a small stomach pouch that is separate from the rest of your stomach. The new stomach pouch is connected to the middle part of the small intestine. Food will bypass (go around) the rest of the stomach and move directly into the small intestine. The surgery makes your stomach permanently smaller so that you feel full sooner and cannot eat as much during meals. Your body will not absorb as many calories from food because part of your stomach and intestines are bypassed.
 |
What do I need to know before I have a roux-en-Y gastric bypass?
- You will work closely with a dietitian before and after surgery. Your dietitian will talk to you about nutrition and what you should eat and drink before and after surgery. You may need to follow a very low-calorie diet for several weeks before surgery. This will help you lose some weight before surgery. Weight loss will help your liver handle anesthesia better. It will also help you create healthy nutrition and activity habits.
- Your surgeon will talk to you about self-care and follow-up activities you will need after surgery. You will need to take vitamins and come in often to have your progress checked.
- If you have diabetes, your diabetes medicine needs may change after surgery. This depends on the medicine you take and if you have type 1 or type 2 diabetes. Do not change your diabetes medicine unless directed. Your providers will help you set schedules for checking your blood sugar levels and taking your medicine.
- Your medicine needs may change if you are taking medicine for hypothyroidism. Your healthcare providers will monitor your TSH levels and make medicine changes if needed. Do not change your thyroid medicine unless directed.
- Your surgeon will talk to you about family planning if you are a woman of childbearing age. It is important that you do not get pregnant for 12 to 18 months after surgery. Then your pregnancy will need to be monitored for your safety and your baby's safety. Your provider will tell you how much weight is safe for you to gain during pregnancy. He or she will help you create healthy meal plans so you get the right nutrition without gaining too much weight. If you want to prevent pregnancy, healthcare providers will help you choose the right kind of birth control. You may not be able to use birth control pills because you will not be able to absorb them fully after surgery.
How do I prepare for surgery?
- Your surgeon will talk to you about how to prepare for surgery. He or she may tell you not to eat or drink anything after midnight on the day of your surgery. Arrange to have someone drive you home and stay with you to make sure you are okay.
- Tell your surgeon about all medicines you currently take. He or she will tell you if you need to stop any medicine for surgery, and when to stop. He or she will tell you which medicines to take or not take on the day of your surgery.
- Tell your surgeon about all your allergies, including anesthesia or antibiotics. You may be given an antibiotic to help prevent a bacterial infection.
- You may need a fasting blood test to check your lipid (fat) levels, or other blood tests. Your heart may be checked to make sure it is healthy enough for surgery. You may also need tests to check your digestive system.
- If you have diabetes, healthcare providers will help you schedule meals and medicines before surgery. Your A1c level may also be checked.
- If you currently use tobacco products, you will need to quit before you have surgery. It is best to quit at least 1 year before surgery. You must quit at least 6 weeks before surgery. Talk to your surgeon or other healthcare providers if you need help quitting.
What will happen during surgery?
- You may be given general anesthesia to keep you asleep and free from pain during surgery. You may instead be given spinal anesthesia to numb the surgery area. With spinal anesthesia, you may still feel pressure or pushing during surgery, but you should not feel pain.
- Your surgeon will make small incisions in your abdomen. He or she will use staples to make a small stomach pouch that is closed off from the rest of your stomach. The new stomach pouch is then connected to the middle part of the small intestine. The incisions will be closed with stitches or medical tape.
What will happen after surgery?
- Medicines may be given to prevent or treat pain, nausea, or a bacterial infection.
- A nasogastric (NG) tube may be put into your nose and down into your stomach during surgery. The NG tube helps prevent vomiting and may help get your intestines working. The NG tube is usually removed 1 day after surgery.
- A test called a contrast swallow may be done the first day after surgery. This test checks for leaks in your stomach. You will be able to have clear liquids when your stomach starts working after surgery and tests show no leaks. You may be given ice chips at first. Then you will get clear liquids such as water, broth, or juice.
- You will be helped to walk around after surgery to help prevent blood clots.
- As you begin to eat differently, you may begin to lose weight. It may take several months to reach a healthy weight.
What are the risks of roux-en-Y gastric bypass surgery?
You may bleed more than expected or get an infection. Your spleen or other organs may be injured during surgery. You may have abdominal pain, heartburn, or a stomach ulcer. You may develop a life-threatening blood clot. The staples inside your stomach could break down. The new connections to your stomach and intestines could form scars, narrow areas, or leaks. Stomach juices may leak into your abdomen and you may need emergency surgery. You may develop gallstones or an incisional hernia (a weak area near your incision). You may need a larger incision than expected during laparoscopic surgery. After surgery, you may not lose any weight. You may lose weight and then gain it back.
Care Agreement
You have the right to help plan your care. Learn about your health condition and how it may be treated. Discuss treatment options with your healthcare providers to decide what care you want to receive. You always have the right to refuse treatment. The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.© Copyright Merative 2024 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
Learn more about Roux-En-Y Gastric Bypass
Treatment options
Care guides
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
