Rheumatic Heart Disease
Medically reviewed by Drugs.com. Last updated on Aug 4, 2025.
AMBULATORY CARE:
Rheumatic heart disease (RHD)
is permanent heart valve damage that develops because of rheumatic fever. Rheumatic fever is an autoimmune response to a group A strep (GAS) bacterial infection that is not fully treated. The bacteria can cause infections such as strep throat, scarlet fever, or impetigo. Your immune system overreacts to the bacteria. This causes inflammation to build up in many areas of your body, including your heart. You may develop RHD right away after 1 strep infection. RHD may develop 20 or 30 years later, or after several infections.
Signs and symptoms
may develop while you have rheumatic fever, or may not start until many years later. The following are common signs and symptoms of RHD:
- Chest pain
- Palpitations (strong heartbeats), heart rhythm problems, or a heart murmur
- Shortness of breath or coughing up blood
- Swelling in your hands or feet
- Fatigue (tired mentally and physically)
Call your local emergency number (911 in the US) or have someone call if:
- You have any of the following signs of a heart attack:
- Squeezing, pressure, or pain in your chest
- You may also have any of the following:
- Discomfort or pain in your back, neck, jaw, stomach, or arm
- Shortness of breath
- Nausea or vomiting
- Lightheadedness or a sudden cold sweat
- You have any of the following signs of a stroke:
- Numbness or drooping on one side of your face
- Weakness in an arm or leg
- Confusion or difficulty speaking
- Dizziness, a severe headache, or vision loss
Seek care immediately if:
- You are lightheaded, dizzy, or faint when you stand up.
Call your doctor or cardiologist if:
- You have increased swelling in your legs or ankles.
- Your heart beats faster than usual.
- You feel your heart flutter often.
- You have questions or concerns about your condition or care.
Treatment
may include any of the following:
- Medicines may be used to help your heart beat more regularly. Medicine may be given to get rid of extra fluid in your body. This medicine may make you urinate more often. You may also need blood thinning medicine to prevent blood clots. This medicine increases your risk for bleeding and bruising.
- Antibiotics may be given as monthly injections for years to prevent another GAS infection.
- Surgery may be needed to repair or replace a damaged heart valve.
Manage or prevent RHD:
- Always have strep throat, scarlet fever, or impetigo fully treated. Rheumatic fever can develop again, even after treatment. Get tested for a GAS infection as soon as symptoms develop. You will need antibiotics to treat the infection. It is important to take every dose, even if you feel better sooner.
- Talk to your healthcare provider about pregnancy. Pregnancy makes your heart work harder. You and your baby may need to be monitored by specialists during your pregnancy.
- Ask about vaccines you may need. Vaccines help lower your risk for infections that can lead to disease. Get a flu vaccine as soon as recommended each year, usually in September or October. Get a COVID-19 vaccine as often as recommended. Your provider can tell you if you also need other vaccines, and when to get them.
- Be physically active, as directed. Physical activity, such as exercise, can help improve heart health. Ask your provider which activities are safe for you to do. The amount and type of exercise that is safe may depend on how severe your condition is.
- Do not smoke. Nicotine and other chemicals in cigarettes and cigars can cause lung and heart damage. Ask your provider for information if you currently smoke and need help to quit. E-cigarettes and smokeless tobacco still contain nicotine. Talk to your provider before you use these products.
- Limit or do not drink alcohol. Alcohol can raise your blood pressure and put stress on your heart. Your provider can tell you how many drinks are okay to have within 24 hours or within 1 week. A drink of alcohol is 12 ounces of beer, 5 ounces of wine, or 1½ ounces of liquor.
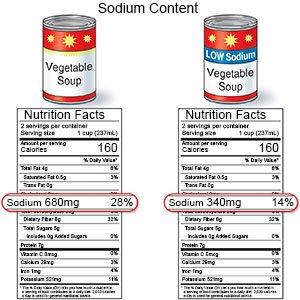
- Limit sodium (salt) as directed. Too much sodium can affect your fluid balance. Check labels to find low-sodium or no-salt-added foods. You can also make small changes to get less salt. For example, if you add salt while you cook, do not add more salt at the table. Ask your healthcare provider or dietitian for more ways to cut down on salt.
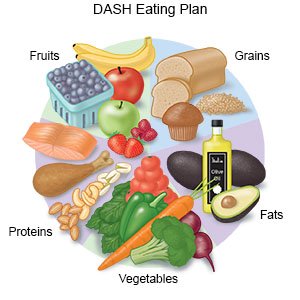
- Eat heart-healthy foods. Heart-healthy foods include salmon, tuna, walnuts, whole-grain breads, low-fat dairy products, beans, and oils such as olive or canola oil. A dietitian or your provider can give you more information on meal plans such as the DASH (Dietary Approaches to Stop Hypertension) eating plan. The DASH plan is low in sodium, processed sugar, unhealthy fats, and total fat. It is high in potassium, calcium, and fiber. These can be found in vegetables, fruit, and whole-grain foods.
Follow up with your doctor or cardiologist as directed:
You may need to return regularly for tests to check your heart. Write down your questions so you remember to ask them during your visits.
© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
