Pseudoaneurysm
Medically reviewed by Drugs.com. Last updated on Aug 4, 2025.
AMBULATORY CARE:
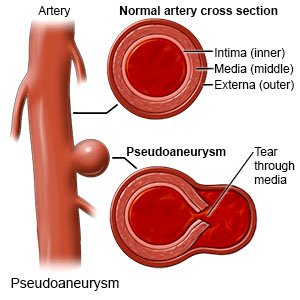
A pseudoaneurysm,
or false aneurysm, is a bulge that forms on an injured artery. An artery has 3 layers. Blood leaks through 1 or 2 layers and pools in a sac attached to the artery. A pseudoaneurysm can form in any artery. It becomes a medical emergency if it ruptures (bursts).
 |
Common signs and symptoms:
A small pseudoaneurysm may not cause any signs or symptoms. A larger pseudoaneurysm may cause any of the following:
- A lump under your skin that may be painful or tender to the touch
- Numbness, pain, or tingling in the area
- A bruise on the skin over the area
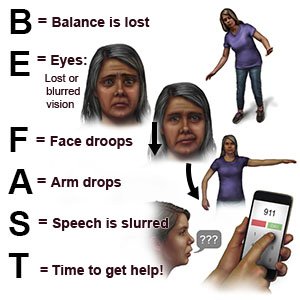
Call your local emergency number (911 in the US) or have someone call if:
- You have any of the following signs of a stroke:
- Numbness or drooping on one side of your face
- Weakness in an arm or leg
- Confusion or difficulty speaking
- Dizziness, a severe headache, or vision loss
- You have chest pain or an irregular heartbeat.
- You have severe pain at the artery site.
- You have shortness of breath, dizziness, or confusion.
- You cough up blood.
Seek care immediately if:
- You have swelling or pain near the artery site.
- You have numbness or pain in your arm or leg.
Call your doctor or neurologist if:
- You have sudden or more pain in your groin.
- Your skin over the pseudoaneurysm is cool to the touch, pale, or changes color.
- You have tingling or numbness near the pseudoaneurysm site.
- You have questions or concerns about your condition or care.
Treatment:
Your healthcare provider will use an ultrasound to check the artery for leaking blood. A small pseudoaneurysm may close on its own in about 4 weeks. You may need any of the following to treat a pseudoaneurysm that does not close:
- Medicine called thrombin may be injected into the sac to help seal the leak. You may need an arterial duplex scan 24 hours after the injection. Your provider will check to make sure the leak is sealed and that the injection did not cause damage. Medicines may also be given to lower your blood pressure or cholesterol level.
- Compression is a procedure that may be used if the pseudoaneurysm is in your leg. Your provider will place a device over the pseudoaneurysm and apply pressure. Your provider may hold the pressure for 10 to 15 minutes. You may need to have this procedure a few times.
- Endovascular repair is a procedure to fix the artery. The procedure helps lower the risk that the pseudoaneurysm will burst.
- Surgery may be used to repair the leak. Your surgeon may stitch the artery leak closed or place a patch to seal it. Your surgeon may need to bypass the artery (direct blood so it does not flow into the artery). Dead tissue may need to be removed if the area around the pseudoaneurysm becomes infected.
Manage or prevent a pseudoaneurysm:
Your healthcare provider will give you specific directions to help you manage your pseudoaneurysm. The following are general guidelines:
- Control or prevent high blood pressure (BP). High BP increases the risk that the pseudoaneurysm will burst. Your provider may recommend that you limit the amount of sodium (salt) you have every day. You may need to check your BP and keep a record of the numbers. You may also need to take medicine to control your BP.

- Follow your provider's directions for physical activity. You may need to limit activity to lower the risk that the pseudoaneurysm will burst. Your provider may help you create a physical activity plan after treatment. Physical activity helps lower the risk for another pseudoaneurysm by controlling some risk factors. Examples include controlling your BP and cholesterol levels, and maintaining a healthy weight. Ask your provider what a healthy weight is for you. Your provider can help you create a healthy weight loss plan, if needed.
- Do not use nicotine products, alcohol, or stimulating drugs. Nicotine and other chemicals in cigarettes and cigars can cause blood vessel and lung damage. Nicotine, alcohol, and stimulating drugs such as cocaine can raise your BP. Alcohol also thins your blood. Ask your healthcare provider for information if you currently use nicotine, alcohol, or street drugs and need help to quit. Do not use e-cigarettes or smokeless tobacco in place of cigarettes. These still contain nicotine.
- Eat a variety of healthy foods. Healthy foods include fruits, vegetables, whole-grain breads, beans, lean meats, fish, and low-fat dairy products. Your provider or dietitian can help you create a meal plan to help control high BP or cholesterol levels.

Follow up with your doctor or neurologist as directed:
Write down your questions so you remember to ask them during your visits.
© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.
Learn more about Pseudoaneurysm
Treatment options
Care guides
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
