Open Repair of Thoracic Aortic Aneurysm
Medically reviewed by Drugs.com. Last updated on Aug 4, 2025.
What do I need to know about open repair of a thoracic aortic aneurysm (TAA)?
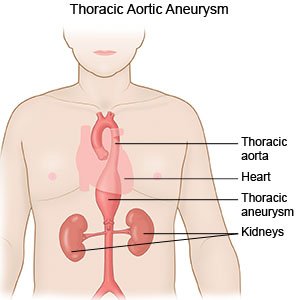
Open repair of a TAA is surgery to remove an aneurysm (bulge) in your aorta. The aorta is a large blood vessel that goes from your heart down into your abdomen. The TAA will be replaced with a graft (tube). After surgery, blood will flow through the graft instead of the aneurysm. Open repair may be planned if the aneurysm is growing but not leaking. The surgery will help prevent the aneurysm from bursting or leaking. A burst or leaking aneurysm can be life-threatening. The repair will be done immediately if the aneurysm bursts.
 |
How do I prepare for a planned open repair of a TAA?
- Your surgeon will tell you how to prepare. Your surgeon may tell you not to eat anything after midnight on the day of surgery. You may be able to drink clear liquids up to 2 hours before your surgery. You may need to spend 1 week or more in the hospital after surgery. Arrange to have someone drive you home after you are discharged. This person may need to stay with you for at least 1 week to make sure you are okay.
- Your surgeon may recommend cardiac rehabilitation (rehab). Cardiac rehab is a program run by a team of specialists who will help you create a management plan. The plan may include exercise, relaxation, stress management, and heart-healthy nutrition. Your team can help you quit using nicotine products or stimulating drugs, if needed. Nicotine may cause blood vessel damage and delay healing or increase your risk for another aneurysm. Your team will recommend that you quit using nicotine at least 4 weeks before surgery. Stimulating drugs such as cocaine increase your blood pressure (BP). A high BP increases the risk for a burst aneurysm.
- You may need blood tests or a CT scan to help your surgeon plan your surgery. You may be given contrast liquid through an IV to help your aneurysm show up better in the CT pictures. You may be given antibiotics to help prevent an infection. Tell your surgeon about any allergies you have, including to medicines, contrast liquid, or anesthesia. Tell healthcare providers if you or anyone in your family has had a problem with anesthesia.
- Tell your surgeon about all your current medicines, including any herbs or supplements. Your surgeon will tell you if you need to stop any medicine for surgery, and when to stop. Your surgeon will also tell you which medicines to take or not take on the day of surgery.
Related medications
What will happen during surgery?
- You will be given general anesthesia to keep you asleep and free from pain during surgery. Your surgeon may make an incision in the middle of your chest. The incision may instead start under your shoulder blade, wrap around your ribcage, and end on your chest. The incision may go down to your abdomen. The location of the incision depends on where the aneurysm is in your aorta. Your surgeon will clamp the aorta to stop the blood flow through the aneurysm. Your surgeon will remove the aneurysm and replace it with a graft.
- Your surgeon will remove the clamps to let blood flow. The incision may be closed with stitches, staples, medical glue, or adhesive strips. The incision may instead be left open for a few days. This will help your healthcare providers check for damage to your kidneys or bowel. You will need a second surgery to close your incision if it was left open. A bandage will be placed over your incision site to help keep the area clean and dry to prevent infection.
What should I expect after surgery?
- You will be taken to a room or the intensive care unit (ICU). Healthcare providers will watch you closely for any problems. You may have pain, swelling, or bruising in the surgery area. These should get better within a few days.
- You may need medicine to prevent or treat pain, nausea, and vomiting. Medicines may be needed to lower your BP or cholesterol level. Blood thinners may be given to prevent blood clots. You may bleed or bruise more easily while you are taking blood thinners.
- The pulses in your legs and feet will be checked often. A weak pulse may mean blood is not flowing well to your legs. You may be helped to walk around after surgery. Your providers may give you exercises to do in bed. You may also need to wear pressure stockings or inflatable boots. Exercise and pressure stockings or boots help improve blood flow and prevent clots.

- You may have a Foley catheter in your bladder to help remove urine. You may have an endotracheal (ET) tube. An ET tube is attached to a ventilator. A ventilator is a machine that breathes for you when you cannot breathe well on your own.
What are the risks of an open repair of a TAA?
You may bleed more than expected during or after surgery. You may develop an infection in the surgery area or the graft. Blood flow to your legs or spine may be decreased from blood vessel damage or a blood clot. The decrease may cause weakness or loss of movement in your legs, or damage your kidneys or bowel. You may develop another TAA even after you have this surgery. You may have a heart attack or stroke during or after surgery. These can be life-threatening.
Care Agreement
You have the right to help plan your care. Learn about your health condition and how it may be treated. Discuss treatment options with your healthcare providers to decide what care you want to receive. You always have the right to refuse treatment. The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
