Non-Small Cell Lung Cancer
Medically reviewed by Drugs.com. Last updated on Aug 4, 2025.
Non-small cell lung cancer (NSCLC) is the most common type of lung cancer.
 |
DISCHARGE INSTRUCTIONS:
Call your local emergency number (911 in the US) if:
- You suddenly have more trouble breathing than usual.
Seek care immediately if:
- You cannot think clearly.
- Your lips or nails look blue or pale.
- You have a headache or dizziness.
- You have more swelling in your face, arms, neck, or chest.
Call your doctor or oncologist if:
- You have a fever.
- You have severe pain.
- Your symptoms such as wheezing, or cough, get worse.
- You have questions or concerns about your condition or care.
Manage your symptoms:
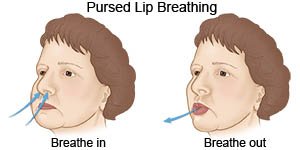
- Use pursed-lip breathing any time you feel short of breath. Take a deep breath in through your nose. Slowly breathe out through your mouth with your lips pursed for twice as long as you inhaled. You can also practice this breathing pattern while you bend, lift, climb stairs, or exercise. It slows down your breathing and helps move more air in and out of your lungs.
- Eat small meals often. Your shortness of breath may make it hard to eat a lot of food at one time. Eat a variety of healthy foods. Healthy foods include fruits, vegetables, whole-grain breads, low-fat dairy products, beans, lean meats, and fish. Ask if you need to be on a special diet.

- Drink liquids as directed. Ask how much liquid to drink each day and which liquids are best for you. Drink extra liquids to prevent dehydration. You will need to drink extra liquids if you are vomiting or have diarrhea from cancer treatments.
- Limit or do not drink alcohol. Alcohol can make breathing problems worse. Ask your healthcare provider if alcohol is okay for you. Your provider may tell you to limit the amount you drink. A drink is 12 ounces of beer, 5 ounces of wine, or 1½ ounces of liquor.
- Balance exercise with rest. Ask about the best exercise plan for you. Exercise may improve your energy levels and appetite. It can also help you heal faster after treatment or surgery. Rest when you feel tired.
Lower your risk for NSCLC:
- Do not smoke. Nicotine and other chemicals in cigarettes and cigars can cause lung damage. Ask your healthcare provider for information if you currently smoke and need help to quit. E-cigarettes or smokeless tobacco still contain nicotine. Talk to your healthcare provider before you use these products.
- Smokefree.gov
Phone: 1- 800 - 784-8669
Web Address: www.smokefree.gov
- Smokefree.gov
- Have lung cancer screening, if recommended. Screening is a test done to find lung cancer early. Screening may be recommended if you are a heavy smoker or you quit within the past 15 years. A heavy smoker means at least 1 pack each day for 20 years or 2 packs each day for 10 years. You can have screening if you are at least 50 years old, never had lung cancer, and do not have any symptoms. Screening may be done 1 time each year until you are 77 to 80. Ask your provider for more information about lung cancer screening.
- Have your home tested for radon and asbestos. You can decrease your exposure to radon and asbestos by having your home tested and treated. Ask your healthcare provider how to get your home tested. If asbestos is found in your home, do not try to remove it yourself. Have a professional remove it.
- Limit your exposure to harmful chemicals in the workplace. Asbestos and other harmful chemicals can be found in mines, mills, textile plants, and shipyards. Follow procedures and policies to protect yourself at work. Use protective equipment such as masks to decrease your risk of inhaling harmful chemicals.
Use oxygen as directed:
You may need extra oxygen if your blood oxygen level is lower than it should be. You may get oxygen through a mask placed over your nose and mouth or through small tubes placed in your nostrils. Ask your healthcare provider before you stop using the oxygen. Do not smoke and stay away from others that smoke when you are using oxygen.
Follow up with your oncologist as directed:
You may need to return for pulmonary function tests (PFTs) to see how well your lungs are working. You will need to see your oncologist often for ongoing treatments. Write down your questions so you remember to ask them during your visits.
© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.
Learn more about Non-Small Cell Lung Cancer
Treatment options
Care guides
Symptoms and treatments
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
