Neuromuscular Disease
Medically reviewed by Drugs.com. Last updated on Aug 4, 2025.
AMBULATORY CARE:
A neuromuscular disease
is a condition that prevents nerves from sending signals to your muscles properly. Abnormal nerve signals may cause muscles to become weak and atrophy (waste away). Examples of neuromuscular disease include amyotrophic lateral sclerosis (ALS), muscular dystrophy, and myasthenia gravis.
Common signs and symptoms of a neuromuscular disease:
- Muscle weakness that gets worse over time, contractures (tight or stiff muscles), or muscle cramps
- Tingling or loss of feeling in parts of your body, or paralysis
- A weak hand grip, dropping things often, or trouble buttoning clothes or writing
- Feeling more tired than usual, dragging one leg, or tripping when you walk
- Arm or leg jerks while resting, or muscle twitching
- Slurred or nasal speech
- Trouble chewing or swallowing, or drooling
- Trouble breathing, blurred or double vision, a drooping eyelid, or dizziness
- Trouble controlling your bladder or bowels
Call your local emergency number (911 in the US), or have someone call if:
- You have chest pain or shortness of breath.
- You become confused, or you have trouble speaking.
- You have trouble breathing.
- You fall and hit your head.
Seek care immediately if:
- You feel lightheaded, dizzy, or faint.
- You have a severe headache or vision changes.
Call your doctor or neurologist if:
- You have a fever.
- You have new or worsening symptoms.
- You choke or cough when you eat or drink.
- You have questions or concerns about your condition or care.
Treatment
may include any of the following:
- Medicines may be given to decrease nerve damage or keep your immune system from attacking nerve cells. Medicines may be used to prevent or relieve muscle stiffness, twitches, or restlessness. Medicines may be used to ease muscle cramps, increase energy, or reduce saliva or mucus. Your healthcare provider may use several types of medicine to help manage your symptoms. The medicines may change over time as your condition improves or worsens.
- Plasmapheresis is a procedure to remove antibodies from your blood that are attacking nerve cells.
- Respiratory therapy may be needed to help prevent or manage breathing problems. It may include the use of devices that help you breathe better.
- Extra oxygen may be given if you develop breathing problems. You may need a ventilator if your breathing problems become severe. A ventilator is a machine that breathes for you.
- Surgery may be done to remove your thymus gland or to release tight muscles. Surgery may also be used to prevent or relieve other symptoms, depending on the type of neuromuscular disease you have.
Manage a neuromuscular disease:
- Go to therapy as directed. A physical therapist teaches you exercises to help improve movement and strength, and to decrease pain. An occupational therapist teaches you skills to help with your daily activities. A speech therapist can teach you exercises to help you swallow more easily. A respiratory therapist can teach you exercises to prevent or manage breathing problems. Therapy helps you maintain muscle function, reduce atrophy and contractures, and prevent problems from lack of movement.
- Prevent falls in your home. A 4-pronged cane or a walker may help you feel safer when you walk. Remove rugs from the floor to help prevent falls. Chairs with side arms and hard cushions may make it easier to get up. Put grab bars on the walls beside toilets and inside showers and bathtubs. You may want to put a shower chair inside the shower. Have someone test the water before you bathe if you have trouble feeling heat.

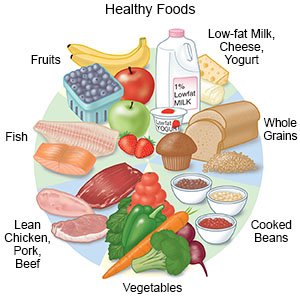
- Eat healthy foods. Healthy foods can help you build your strength. Healthy foods include fruits, vegetables, whole-grain breads, low-fat dairy products, beans, lean meats, and fish. Ask if you need to be on a special diet. A dietitian can help you plan meals with foods that are easier or safer for you to swallow.
- Do not smoke. Nicotine and other chemicals in cigarettes and cigars can lead to or worsen nerve damage. Ask your healthcare provider for information if you currently smoke and need help to quit. E-cigarettes and smokeless tobacco still contain nicotine. Talk to your provider before you use these products.
- Ask about vaccines you may need. If you are taking certain medicines, your provider will help you schedule vaccines. You may need to get some vaccines 4 to 6 weeks before or 2 to 6 months after treatment. Talk to your provider about any other concerns or questions you have about vaccines. Examples include if vaccines will affect your symptoms or interact with your treatment.
Follow up with your doctor or neurologist as directed:
You will need to have regular visits to help manage your symptoms. Write down your questions so you remember to ask them during your visits.
© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
