Lumbar Spinal Stenosis
Medically reviewed by Drugs.com. Last updated on Aug 4, 2025.
What is lumbar spinal stenosis?
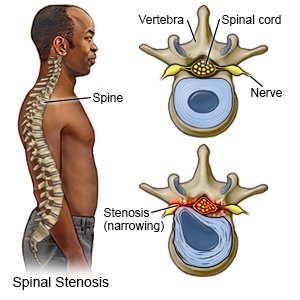
Lumbar spinal stenosis is narrowing of the spinal canal in your lower back. Your spinal canal is the opening in your spine that contains your spinal cord. When your spinal canal narrows, it may put pressure on your spinal cord and nerves.
 |
What causes lumbar spinal stenosis?
Narrowing of your spinal canal may be caused by changes that happen as you age. These changes include bone spurs (growths), herniated discs, and thickened ligaments. Bone growths can be caused by osteoarthritis. A herniated disc bulges out between the vertebrae (bones) and into your spinal canal. Discs are spongy cushions between the vertebrae in your spine. Herniated discs may be caused by activities that increase stress on the spine. An example is heavy lifting. Ligaments that connect the vertebrae may thicken and harden as you get older. Other conditions, such as spinal injuries and Paget's disease, can also cause spinal stenosis.
What are the signs and symptoms of lumbar spinal stenosis?
Signs and symptoms may start or get worse when you stand or walk. They are often relieved when you sit or lean forward.
- Low back pain
- Pain, numbness, tingling, or weakness in one or both legs
- Pain in your buttocks that extends to your thighs or legs
How is lumbar spinal stenosis diagnosed?
Your healthcare provider will ask about your symptoms and when they started. He or she will ask if you have any medical conditions. Your provider may ask you to lift, bend, walk, sit, or reach. An x-ray, MRI or a CT may show problems in your spine that are causing spinal stenosis. You may be given contrast liquid to help the spine show up better in the pictures. Tell the healthcare provider if you have ever had an allergic reaction to contrast liquid. Do not enter the MRI room with anything metal. Metal can cause serious injury. Tell the healthcare provider if you have any metal in or on your body.
How is lumbar spinal stenosis treated?
- NSAIDs , such as ibuprofen, help decrease swelling, pain, and fever. NSAIDs can cause stomach bleeding or kidney problems in certain people. If you take blood thinner medicine, always ask your healthcare provider if NSAIDs are safe for you. Always read the medicine label and follow directions.
- Acetaminophen decreases pain and fever. It is available without a doctor's order. Ask how much to take and how often to take it. Follow directions. Read the labels of all other medicines you are using to see if they also contain acetaminophen, or ask your doctor or pharmacist. Acetaminophen can cause liver damage if not taken correctly.
- Prescription pain medicine may be given. Ask how to take this medicine safely.
- Muscle relaxers help decrease pain and muscle spasms.
- A steroid injection may be given to reduce inflammation. Steroid medicine is injected into the epidural space. The epidural space is between your spinal cord and vertebrae.
- A nerve block is an injection of numbing medicine. You may need a nerve block if your pain is not going away, or is getting worse.
- Surgery may be needed to widen your spinal canal or decrease pressure on your spinal cord. Surgery may also be done to fix damaged or injured vertebrae in your back.
How can I manage my symptoms?
- Go to physical and occupational therapy as directed. A physical therapist teaches you exercises to help improve movement and strength, and to decrease pain. An occupational therapist teaches you skills to help with your daily activities.
- Rest when you feel it is needed. Slowly start to do more each day. Return to your daily activities as directed.
- Apply heat on your back for 20 to 30 minutes every 2 hours for as many days as directed. Heat helps decrease pain and muscle spasms.
- Apply ice on your back for 15 to 20 minutes every hour or as directed. Use an ice pack, or put crushed ice in a plastic bag. Cover it with a towel before you apply it to your skin. Ice helps prevent tissue damage and decreases swelling and pain.
When should I seek immediate care?
- You have pain in your leg that does not go away or gets worse.
- You have trouble moving your legs.
- You cannot control when you urinate or have a bowel movement.
When should I contact my healthcare provider?
- You have new or worsening symptoms.
- Your symptoms keep you from doing your daily activities.
- You have questions or concerns about your condition or care.
Care Agreement
You have the right to help plan your care. Learn about your health condition and how it may be treated. Discuss treatment options with your healthcare providers to decide what care you want to receive. You always have the right to refuse treatment. The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
