Leg Fracture in Children
Medically reviewed by Drugs.com. Last updated on Aug 4, 2025.
What do I need to know about a leg fracture?
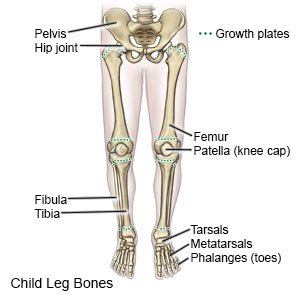
A leg fracture is a break in a bone in your child's leg.
 |
What are the signs and symptoms of a leg fracture?
- Pain that worsens when your child moves his or her leg
- A lump, swelling, or bruise at the site of the fracture
- Trouble walking, lifting, or putting weight on the leg
- Leg position or shape that is not normal
How is a leg fracture diagnosed?
Your child's healthcare provider will examine your child's leg. The provider may touch areas of your child's leg to see if he or she has decreased feeling. The provider will check for any open breaks in the skin. He or she may check your child's ability to move his or her leg. Your child may need an x-ray, CT scan, or MRI. Contrast liquid may be used to help the fracture show up better in the pictures. Tell the healthcare provider if your child has ever had an allergic reaction to contrast liquid. Do not let your child enter the MRI room with anything metal. Metal can cause serious injury. Tell the healthcare provider if your child has any metal in or on his or her body.
How is a leg fracture treated?
Treatment will depend on the kind of fracture your child has. Your child may need any of the following:
- A cast or brace may be placed on your child's leg to prevent movement and hold the broken bones in place. These may help decrease pain and prevent more bone damage.
- Prescription pain medicine may be given. Ask your child's healthcare provider how to give this medicine safely. Some prescription pain medicines contain acetaminophen. Do not give your child other medicines that contain acetaminophen without talking to a healthcare provider. Too much acetaminophen may cause liver damage. Prescription pain medicine may cause constipation. Ask your child's healthcare provider how to prevent or treat constipation.
- NSAIDs , such as ibuprofen, help decrease swelling, pain, and fever. This medicine is available with or without a doctor's order. NSAIDs can cause stomach bleeding or kidney problems in certain people. If your child takes blood thinner medicine, always ask if NSAIDs are safe for him or her. Always read the medicine label and follow directions. Do not give these medicines to children younger than 6 months without direction from a healthcare provider.
- Acetaminophen decreases pain and fever. It is available without a doctor's order. Ask how much to give your child and how often to give it. Follow directions. Read the labels of all other medicines your child uses to see if they also contain acetaminophen, or ask your child's doctor or pharmacist. Acetaminophen can cause liver damage if not taken correctly.
- Closed reduction is used to put your child's bones back into the correct position without surgery.
- Open reduction surgery may be needed to put your child's bones back into the correct position. Wires, pins, plates, or screws may be used to keep the broken pieces lined up correctly.
What can I do to help care for my child's leg fracture?
- Have your child rest as much as possible and get plenty of sleep.
- Apply ice on your child's leg for 15 to 20 minutes every hour or as directed. Use an ice pack, or put crushed ice in a plastic bag. Cover it with a towel before you apply it. Ice helps prevent tissue damage and decreases swelling and pain.
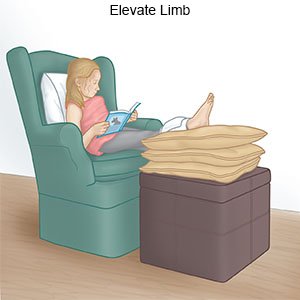
- Elevate your child's leg above the level of his or her heart as often as possible. This will help decrease swelling and pain. Prop your child's leg on pillows or blankets to keep it elevated comfortably.
- Have your child use crutches as directed. Crutches will help your child keep some weight off the leg while it heals.
- Take your child to physical therapy as directed. A physical therapist teaches your child exercises to help improve movement and strength, and to decrease pain.
When should I seek immediate care?
- Your child has increased pain in his or her leg that does not go away, even after he or she takes medicine.
- Your child's cast gets wet or damaged.
- Your child's leg or toes are numb.
- Your child's skin or toenails become swollen, cold, white, or blue.
When should I call my child's doctor?
- Your child has a fever.
- Your child's cast or brace is too tight.
- You notice new blood stains or a bad smell coming from under the cast.
- Your child has new or worsening trouble moving his or her leg.
- You have questions or concerns about your child's condition or care.
Care Agreement
You have the right to help plan your child's care. Learn about your child's health condition and how it may be treated. Discuss treatment options with your child's healthcare providers to decide what care you want for your child. The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
Learn more about Leg Fracture
Care guides
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
