Iliotibial Band Syndrome
Medically reviewed by Drugs.com. Last updated on Aug 4, 2025.
AMBULATORY CARE:
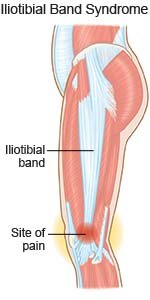
Iliotibial band syndrome (ITBS)
is an overuse injury most often seen in long distance runners and cyclists. The iliotibial (IT) band is a long band of connective tissue. It runs along the outside of your thigh and connects your hip and knee joints. The IT band helps keep your knee stable while you stand, move, or exercise. The IT band becomes irritated and inflamed from repeated movement. This causes knee pain.
 |
Common signs and symptoms:
- Pain on the outside of your knee
- Swelling in or around your knee
- A clicking or popping sound or feeling
- Pain that may move up your thigh to your hip
Call your doctor if:
- You have a fever or chills.
- You have redness, warmth, or severe swelling in or around your knee.
- Your pain does not improve or gets worse after treatments.
- You have questions or concerns about your condition or care.
Treatment
may include any of the following:
- NSAIDs , such as ibuprofen, help decrease swelling, pain, and fever. This medicine is available with or without a doctor's order. NSAIDs can cause stomach bleeding or kidney problems in certain people. If you take blood thinner medicine, always ask your healthcare provider if NSAIDs are safe for you. Always read the medicine label and follow directions.
- Steroid injections may be given to decrease swelling.
- Surgery is usually only recommended if other treatment does not work within 6 months. Many types of ITBS surgery are available. Your healthcare provider can tell you more about surgery, if needed.
Self-care:
- Rest your leg as directed. Return to your daily activities and exercise gradually. Do not do exercises that cause pain.
- Apply ice on your knee as directed. Ice decreases swelling and pain. Use an ice pack, or put crushed ice in a plastic bag. Cover the bag with a towel before you put it on your skin. Apply ice for 15 to 20 minutes every hour or as directed.
- Elevate your calf and foot above the level of your heart as often as you can. This will help decrease swelling and pain. Prop your calf and foot on pillows or blankets to keep it elevated comfortably.

- Massage painful areas as directed. Use a foam roller to gently massage your painful areas. Place the foam roller on a flat surface. Lie on your side with the foam roller against your painful leg. Move so that it rolls up and down from your hip to above your knee. Do not lie with it against the outside of your kneecap.
- Stretch as directed. Stand and wrap your painful leg behind and to the side of your other leg. Reach your arm to the outside of the ankle of your painful leg. Hold for 15 seconds Return to the starting position. Do this 10 times. Repeat this exercise 3 to 5 times per day. Ask your healthcare provider or physical therapist for other ways to stretch.
- Go to physical therapy as directed. Your physical therapist will teach you how to do exercises that will strengthen your hip muscles and improve your flexibility.
Prevent ITBS:
- Get new sports shoes regularly. Over time, the soles of your shoes can wear out in spots. Your shoes should always fit well and support your feet. Your knees should feel steady when you walk or run.
- Slowly increase the time and distance that you run or bike. Start with short runs or cycle rides.
- Run on flat surfaces only. Avoid uneven surfaces, hills, or stairs. These may cause pain and make your condition worse.
- Warm up before you stretch and exercise. This will help prevent an injury. Walk or ride a stationary bike for 5 to 10 minutes.
- Change the seat height or foot position of your bicycle. Ask your physical therapist for help. These changes can decrease the stress on your IT band.
- Use correct body position when you exercise. Ask your healthcare provider or physical therapist how to move your legs and feet when running or cycling. This may decrease the stress on your IT band.
Follow up with your doctor as directed:
Write down your questions so you remember to ask them during your visits.
© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
