Disorders of Consciousness
Medically reviewed by Drugs.com. Last updated on Aug 4, 2025.
The person may be cared for at home after he or she is discharged. Anyone caring for the person will be taught physical and mental care routines, and what to do in an emergency. His or her level of consciousness may be checked regularly.
WHILE YOU ARE HERE:
Informed consent:
You have the right to understand the person's health condition in words that you know. You should be told the tests, treatments, or procedures that may be done. Healthcare providers should also tell you about the risks and benefits of each treatment. Because the person is unable to give consent, you may be given permission to sign a consent form for him or her. You may be asked to sign a form that gives healthcare providers permission to do certain tests, treatments, or procedures. A consent form is a legal piece of paper that tells exactly what will be done for the person. Before you give your consent, make sure all your questions have been answered so that you understand what may happen.
Medicines:
The person may be given any of the following:
- Antibiotics help fight or prevent a bacterial infection.
- Anticonvulsants are given to control or prevent seizures.
- Blood pressure medicine may be given to lower the person's blood pressure and keep it as close to normal as possible.
- Other medicines may be given to treat the problem causing the person's condition. Some may be given to relieve symptoms or prevent health problems.
Monitoring:
- A heart monitor, also called ECG or telemetry, checks the electrical activity of the heart.
- Neuro signs tell healthcare providers how the brain is working after an injury or illness. Healthcare providers check the person's eyes, memory, and ability to wake up. Hand grasp may also be tested. Neuro signs may need to be checked often.
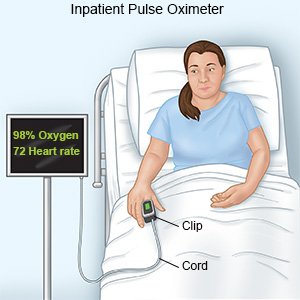
- A pulse oximeter is a machine that shows the amount of oxygen in the blood.
Tests:
- Blood and urine tests may be used to check the person's overall health or organ function. His or her blood sugar level, electrolytes, and blood gases will be checked. The tests may be used to look for signs of infection. The tests may find drugs or alcohol that are affecting the person.
- X-ray, PET, CT, or MRI pictures are used to check the person's brain, heart, and lungs. The pictures may show an infection, a collapsed lung, a tumor, broken ribs, or fluid around the heart or lungs.
- An EEG prints a paper tracing of brain wave activity from several areas of the brain.
- An evoked potential test measures how the nerves and brain react to sound or touch.
- An ECG helps healthcare providers look for damage or problems in different areas of the heart.
Treatment
will depend on the cause of the DoC. The person may need any of the following:
- An IV or nasogastric (NG) tube may be used to give the person nutrition and liquids. An NG tube is put in through the nose and goes down into the stomach. The tube may also go directly from the outside of the body into the stomach. This is called a gastrostomy tube.
- Extra oxygen may be needed to help the person breathe easier. He or she may need a ventilator. This is a machine that can breathe for the person if he or she cannot breathe well on his or her own.
RISKS:
Problems causing a disorder of consciousness can affect a person physically, mentally, or emotionally. Long-term problems may include trouble speaking or moving his arms or legs.
CARE AGREEMENT:
You have the right to help plan the person's care. Learn about his or her health condition and how it may be treated. Discuss treatment options with the person's healthcare providers to decide what care he or she will receive. You always have the right to refuse treatment.© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
