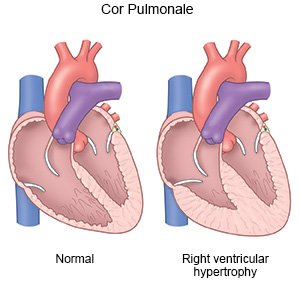
Cor Pulmonale
Medically reviewed by Drugs.com. Last updated on Aug 4, 2025.
Cor pulmonale is a condition that occurs when the right ventricle of your heart cannot pump properly. The right side of your heart pumps blood from your body into your lungs to get oxygen. Cor pulmonale is caused by pulmonary hypertension (PH). PH is high blood pressure in the arteries of your lungs. Blood cannot flow through your lungs and backs up in the right ventricle of your heart. As the right ventricle tries to pump blood properly, it becomes thickened and deformed. Cor pulmonale can become life-threatening.
 |
WHILE YOU ARE HERE:
Informed consent
is a legal document that explains the tests, treatments, or procedures that you may need. Informed consent means you understand what will be done and can make decisions about what you want. You give your permission when you sign the consent form. You can have someone sign this form for you if you are not able to sign it. You have the right to understand your medical care in words you know. Before you sign the consent form, understand the risks and benefits of what will be done. Make sure all your questions are answered.
You may need extra oxygen
if your blood oxygen level is lower than it should be. You may get oxygen through a mask placed over your nose and mouth or through small tubes placed in your nostrils. Ask your healthcare provider before you take off the mask or oxygen tubing.
A central line
is an IV catheter or tube. It is put into a large vein (blood vessel) near your collarbone, in your neck, or in your groin. Other central lines, such as a PICC, may be put into your arm. You may need a central line to receive medicines or IV fluids that need to be given through a big vein. You may need a central line if it is hard for healthcare providers to insert a regular IV. A central line can also stay in longer than a regular IV can. Some central lines may also be used to take blood samples.
Medicines:
- Diuretics are given to decrease excess fluid that collects in a part of your body, such as your legs. Diuretics can also remove excess fluid from around your heart or lungs and decrease your blood pressure. It is often called water pills. You will urinate more often when you take this medicine.
- Heart medicine may be given to strengthen or regulate your heartbeat. It also may help your heart in other ways. Talk with your healthcare provider to find out the name of your heart medicine.
- Vasodilators may improve your blood flow by making the blood vessels in your heart and lungs wider. This may decrease the pressure in your blood vessels and improve your symptoms.
- Bronchodilators are given to relax the airways in your lungs and help you breathe better.
- Blood thinners help prevent clots from forming in the blood. Blood thinners make it more likely for you to bleed or bruise. Use an electric razor and soft toothbrush to help prevent bleeding.
Monitoring:
- A heart monitor is also called an ECG or EKG. Sticky pads placed on your skin record your heart's electrical activity.
- A pulse oximeter is a device that measures the amount of oxygen in your blood. A cord with a clip or sticky strip is placed on your finger, ear, or toe. The other end of the cord is hooked to a machine.
- A pulmonary artery (PA) catheter is a balloon-tipped catheter inserted through a vein in your neck or groin. The PA catheter goes into the right side of your heart and continues to your pulmonary artery. The balloon is inflated to wedge the catheter in place. The PA catheter has a device in it that measures the pressure in your heart and lungs. The catheter is attached to a monitor that shows the pressure measurements. The measurements can also show healthcare providers how your heart responds to certain heart medicines.
Tests:
- Blood tests check your heart and lung function. Your blood is also tested for the amount of gases in it, such as oxygen, acids, and carbon dioxide.
- An EKG checks your heart rhythm for problems, such as heart damage or disease.
- A chest x-ray is a picture of your heart and lungs. Healthcare providers use the x-ray to check the size of your heart. A chest x-ray can also show fluid around your heart and lungs.
- An echocardiogram (echo) uses sound waves to show pictures of the size and shape of your heart. An echo records how your heart moves when it is beating and how blood flows through your heart. These pictures are seen on a monitor.
- MRI or CT scan pictures may be used to check your heart and lungs. CT pictures can show conditions that may have caused cor pulmonale. MRI pictures may show the size and function of the right size of your heart. You may be given contrast liquid to help the pictures show up better. Tell the healthcare provider if you have ever had an allergic reaction to contrast liquid. Do not enter the MRI room with anything metal. Metal can cause serious injury. Tell healthcare providers if you have any metal in or on your body.
- A VQ scan is a ventilation (V) and perfusion (Q) test. It shows the airways and blood vessels in your lungs. It will tell your healthcare provider how well your lungs are working. Radioactive liquid is put into your vein to show how blood flows in your lungs. You will then breathe in a gas. Pictures are taken to see how well your lungs breathe in oxygen.
- Pulmonary function tests (PFTs) show how well your body uses oxygen. You breathe into a mouthpiece connected to a machine. The machine measures how much air you breathe in and out over a certain amount of time. PFTs help your healthcare providers decide the best treatment for you.
- Cardiac catheterization is a test to see how well your heart is working. Your arteries may also be checked to see if they are blocked. A catheter is threaded into your heart through a blood vessel in your leg or arm. Contrast liquid may be given so x-ray pictures of your arteries show up better on a TV-like screen. Tell healthcare providers if you have ever had an allergic reaction to contrast liquid.
RISKS:
Cor pulmonale can become life-threatening if not treated.
CARE AGREEMENT:
You have the right to help plan your care. Learn about your health condition and how it may be treated. Discuss treatment options with your healthcare providers to decide what care you want to receive. You always have the right to refuse treatment.© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.
Learn more about Cor Pulmonale
Treatment options
- Medications for Cor Pulmonale
- Medications for Pulmonary Arterial Hypertension
- Medications for Pulmonary Embolism
- Medications for Pulmonary Heart or Vascular Disease
- Medications for Pulmonary Thromboembolism
Care guides
Medicine.com guides (external)
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
