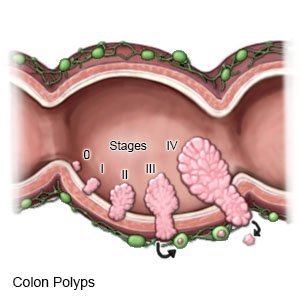
Colorectal Polyps
Medically reviewed by Drugs.com. Last updated on Aug 4, 2025.
What are colorectal polyps?
Colorectal polyps are small growths of tissue in the lining of the colon and rectum. Most polyps are usually benign (not cancer). Certain types of polyps, called adenomatous polyps, may turn into cancer.
 |
What increases my risk for colorectal polyps?
The exact cause of colorectal polyps is unknown. The following may increase your risk:
- Older age
- Foods high in fat and low in fiber
- Family history of polyps
- Intestinal diseases, such as Crohn disease or ulcerative colitis
- Smoking cigarettes or drinking alcohol
- Lack of physical activity, such as exercise
- Obesity
What are the signs and symptoms of colorectal polyps?
- Blood in your bowel movement or bleeding from the rectum
- Change in bowel movement habits, such as diarrhea or constipation
- Abdominal pain
What do I need to know about colorectal polyp screening and diagnosis?
Screening means you are checked for polyps that may be cancer, even if you do not have signs or symptoms. Screening is recommended starting at age 45 and continuing to age 75 if you are at average risk. Screening may start before you are 45 or continue after you are 75 if your risk is high. Your provider will tell you how often to get screened. Timing depends on the type of screening and if polyps or other problems were found. Timing also depends on your age and if you are at increased risk for cancer. Screening may be recommended every 1, 2, 5, or 10 years. Any of the following may be used to find polyps:
- A bowel movement sample may be checked for blood. Blood can be a sign of cancer or large polyps. Several tests are available, such as the fecal immunochemical test (FIT). Your healthcare provider can give you more information on the tests and how they are done. You may need to do this every year or every 3 years, depending on the test you use.
- Colonoscopy or sigmoidoscopy are procedures to help your provider see the inside of your colon. He or she will use a flexible tube with a small light and camera on the end. During a sigmoidoscopy, your provider will only look at rectum and lower colon. During a colonoscopy, he or she will look at the full length of your colon. A small amount of tissue may be removed from your colon for tests.
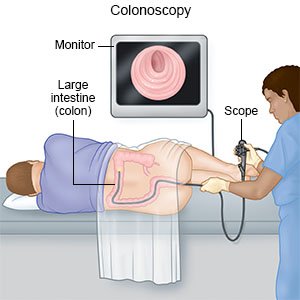
- A virtual colonoscopy is a CT scan that takes pictures of the inside of your colon and rectum. It may be used if you are not able to have a regular colonoscopy or a sigmoidoscopy.
How are colorectal polyps treated?
Small, benign polyps may not need treatment. Your healthcare provider will check the polyp over time to make sure it is not changing. Polyps that are cancer may be removed with one of the following:
- A polypectomy is a minimally invasive procedure to remove a polyp during a colonoscopy or sigmoidoscopy. Your healthcare provider may need to remove the polyp.
- Surgery may be needed to remove large or deep polyps that cannot be removed in a polypectomy. Tissues or lymph nodes near a polyp may also be removed. This helps stop cancer from spreading.
What can I do to lower my risk for colorectal polyps?
- Eat a variety of healthy foods. Healthy foods include fruit, vegetables, whole-grain breads, low-fat dairy products, beans, lean meat, and fish. Ask if you need to be on a special diet.

- Maintain a healthy weight. Ask your healthcare provider what a healthy weight is for you. Ask him or her to help with a weight loss plan if you are overweight.
- Exercise as directed. Begin to exercise slowly and do more as you get stronger. Talk with your healthcare provider before you start an exercise program.
- Limit alcohol. Your risk for polyps increases the more you drink.
- Do not smoke. Nicotine and other chemicals in cigarettes and cigars increase your risk for polyps. Ask your healthcare provider for information if you currently smoke and need help to quit. E-cigarettes or smokeless tobacco still contain nicotine. Talk to your healthcare provider before you use these products.
Where can I find more information?
- National Digestive Diseases Information Clearinghouse (NDDIC)
2 Information Way
Bethesda , MD 20892-3570
Phone: 1- 800 - 891-5389
Web Address: www.digestive.niddk.nih.gov
Call your local emergency number (911 in the US) if:
- You have sudden shortness of breath.
- You have a fast heart rate, fast breathing, or are too dizzy to stand up.
When should I seek immediate care?
- You have severe abdominal pain.
- You see blood in your bowel movement.
When should I call my doctor?
- You have a fever.
- You have chills, a cough, or feel weak and achy.
- You have abdominal pain that does not go away or gets worse after you take medicine.
- Your abdomen is swollen.
- You are losing weight without trying.
- You have questions or concerns about your condition or care.
Care Agreement
You have the right to help plan your care. Learn about your health condition and how it may be treated. Discuss treatment options with your healthcare providers to decide what care you want to receive. You always have the right to refuse treatment. The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
