Cellulitis in Children
Medically reviewed by Drugs.com. Last updated on Aug 4, 2025.
What is cellulitis?
Cellulitis is a skin infection caused by bacteria. Cellulitis is common and can become severe. Cellulitis usually appears on your child's lower legs. It can also appear on his or her arms, face, and other areas. Cellulitis develops when bacteria enter a crack or break in your child's skin, such as a scratch, bite, or cut.
 |
What are the signs and symptoms of cellulitis?
Signs and symptoms usually appear on one side of your child's body. Your child may have any of the following:
- A fever
- A red, warm, swollen area on your child's skin
- Pain when the area is touched
- Red spots, bumps, or blisters
- Bumpy, raised skin that feels like an orange peel
How is cellulitis diagnosed?
Your child's healthcare provider may know your child has cellulitis by looking at his or her skin. Your child may need blood tests to show what kind of bacteria are causing the infection. Other tests may be needed to see how much the infection has spread.
How is cellulitis treated?
You should start to see improvement in your child's symptoms in 3 days. If your child's cellulitis is severe, he or she may need IV antibiotics in the hospital. If cellulitis is not treated, the infection can spread through your child's body and become life-threatening. Your child may need any of the following medicines:
- Antibiotics help treat a bacterial infection.
- Acetaminophen decreases pain and fever. It is available without a doctor's order. Ask how much to give your child and how often to give it. Follow directions. Read the labels of all other medicines your child uses to see if they also contain acetaminophen, or ask your child's doctor or pharmacist. Acetaminophen can cause liver damage if not taken correctly.
- NSAIDs , such as ibuprofen, help decrease swelling, pain, and fever. This medicine is available with or without a doctor's order. NSAIDs can cause stomach bleeding or kidney problems in certain people. If your child takes blood thinner medicine, always ask if NSAIDs are safe for him or her. Always read the medicine label and follow directions. Do not give these medicines to children younger than 6 months without direction from a healthcare provider.
Treatment options
The following list of medications are related to or used in the treatment of this condition.
How can I help manage my child's symptoms?
- Help your child wash the area with soap and water every day. Gently pat dry. Use bandages if directed by your child's healthcare provider.
- Help your child apply cream or ointment as directed. These help protect the area. Most over-the-counter products, such as petroleum jelly, are good to use. Ask your child's healthcare provider about specific creams or ointments to use.
- Place a cool, damp cloth on the area. Use clean cloths and clean water. Cool, damp cloths may help decrease pain.
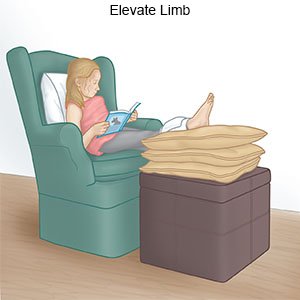
- Elevate the area above the level of your child's heart as often as you can. This will help decrease swelling and pain. Prop the area on pillows or blankets to keep it elevated comfortably.
How can I help prevent cellulitis?
- Remind your child to not scratch bug bites or areas of injury. Your child increases his or her risk for cellulitis by scratching these areas.
- Do not let your child share personal items, such as towels, clothing, and razors.
- Treat athlete's foot or any other skin condition. This can help prevent the spread of a bacterial skin infection.
- Have your child wear protective gear during sports. Some examples include knee or elbow pads, and a helmet.
- Have your child wash his or her hands often. Make sure he or she washes with soap and water after using the bathroom or sneezing. He or she also needs to wash his or her hands before eating. Use lotion to prevent dry, cracked skin.

When should I seek immediate care?
- Your child's wound gets larger and more painful.
- You feel a crackling under your child's skin when you touch it.
- Your child has purple dots or bumps on his or her skin.
- You see red streaks coming from your child's infected area.
When should I call my child's doctor?
- The red, warm, swollen area gets larger.
- Your child's fever or pain does not go away or gets worse.
- The area does not get smaller after 3 days of antibiotics.
- You have questions or concerns about your child's condition or care.
Care Agreement
You have the right to help plan your child's care. Learn about your child's health condition and how it may be treated. Discuss treatment options with your child's healthcare providers to decide what care you want for your child. The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
Learn more about Cellulitis
- Can You Drink Alcohol with Antibiotics?
- Common Side Effects from Antibiotics, and Allergies and Reactions
Treatment options
Care guides
Symptoms and treatments
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
