Bronchiectasis in Children
Medically reviewed by Drugs.com. Last updated on Aug 4, 2025.
What is bronchiectasis?
Bronchiectasis is a condition that causes mucus to collect in your child's airway. Chronic respiratory infections or inflammation cause the bronchi to become thick. Bronchi are larger airways that help carry air in and out of your child's lungs. The lungs make mucus to trap and remove germs and irritants that your child breathes. Bronchiectasis prevents your child's lungs from clearing the mucus. This leads to more infections and inflammation, and scarring in the lungs.
 |
What increases my child's risk for bronchiectasis?
Your child may have bronchiectasis with or without cystic fibrosis. Any of the following may increase his or her risk:
- A health condition your child was born with that makes mucus difficult to clear, such as primary ciliary dyskinesia
- A respiratory infection such as measles or pertussis (whooping cough)
- Lung infections such as pneumonia, or breathing in harmful fumes
- A condition that causes inflammation, such as allergies, rheumatoid arthritis (RA), or inflammatory bowel disease (IBS)
- An obstruction, such as food that gets stuck in your child's airway
- Gastroesophageal reflux (GER)
What are the signs and symptoms of bronchiectasis?
Periods of active signs and symptoms are called exacerbations.
- A chronic cough with mucus that may contain blood
- Wheezing or crackling, shortness of breath, or trouble breathing
- Foul-smelling mucus from your child's lungs
- Weakness and fatigue
- Clubbing of your child's fingers or toes
- Chest pain
How is bronchiectasis diagnosed?
Your child's healthcare provider will listen to his or her lungs and heart. He or she will ask about your child's other health conditions and any medicines he or she takes. Tell the provider about vaccines your child received, and if he or she missed any doses. Your child may also need any of the following tests:
- A sputum (mucus) sample is collected in a cup when your child coughs. The sample is sent to a lab to find out if he or she has an infection.
- X-ray or CT scan pictures are used to check your child's lungs and airway. Your child may be given contrast liquid to help these show up better in the pictures. Tell the healthcare provider if your child has ever had an allergic reaction to contrast liquid.
- Bronchoscopy is done to look inside your child's airway and lungs. Healthcare providers insert a bronchoscope (a tube with a light on the end) into your child's mouth and down into the lungs. Healthcare providers may also collect samples of sputum, fluid, or cells from your child's lungs for testing. This may help find the cause or see if he or she has an infection.
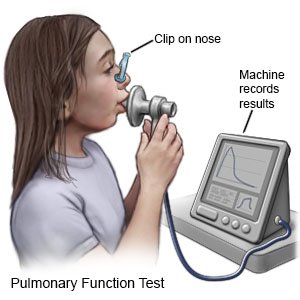
- Pulmonary function tests (PFTs) help healthcare providers learn how well your child's body uses oxygen. Your child breathes into a mouthpiece connected to a machine. The machine measures how much air he or she breathes in and out over a certain amount of time. PFTs help healthcare providers decide the best treatment for your child.
How is bronchiectasis treated?
- Medicines may help relieve your child's symptoms. Bronchodilators help open the air passages in your child's lungs. Antibiotics may be used to treat an infection caused by bacteria. Steroids and some kinds of antibiotics help decrease inflammation in your child's airway. Medicines may help thin the mucus in your child's lungs. Thin mucus may be easier to cough up.
- Oxygen may be given to help your child breathe easier. Oxygen can also decrease the strain on his or her heart and help prevent more breathing problems.
- Surgery may be used to remove a part of your child's lung causing symptoms. Your child may also need a lung transplant if symptoms become severe. Surgery may also be needed to stop heavy bleeding in your child's airway if he or she coughs up a lot of blood.
Treatment options
The following list of medications are related to or used in the treatment of this condition.
How can I help manage my child's bronchiectasis?
- Take your child to pulmonary rehabilitation (rehab) as directed. Pulmonary rehab is a program that can help your child learn how to manage bronchiectasis and prevent exacerbations. The plan will include aerobic exercise, such as walking, swimming, or riding a bicycle. Regular exercise helps your child's lungs work well and helps keep the airway clear. Rehab can help your child increase his or her ability to exercise for as long as recommended. Your child's plan will change over time as he or she starts to become responsible for his or her own care.
- Help your child keep his or her airway clear and open. Have your child do airway clearance techniques as needed. Healthcare providers will show your child how to do these in pulmonary rehab. A saline nasal rinse can help clear irritants from your child's sinuses. Your child can help thin mucus by drinking more liquids or using a cool mist humidifier.
- Help your child avoid cigarette smoke. Nicotine and other chemicals in cigarettes and cigars can cause lung damage and make his or her symptoms worse. Do not smoke around your child or allow others to smoke around him or her. Do not let your adolescent smoke. Ask your healthcare provider for information if he or she currently smokes and needs help to quit. E-cigarettes or smokeless tobacco still contain nicotine. Talk to your healthcare provider before your adolescent uses these products.
What can I do to prevent the spread of germs?
 |
- Have your child wash his or her hands often. He or she should wash after using the bathroom and before preparing or eating food. Have your child use soap and water. Show him or her how to rub soapy hands together, lacing the fingers. Wash the front and back of the hands, and in between the fingers. The fingers of one hand can scrub under the fingernails of the other hand. Teach your child to wash for at least 20 seconds. Use a timer, or sing a song that is at least 20 seconds. An example is the happy birthday song 2 times. Have your child rinse with warm, running water for several seconds. Then dry with a clean towel or paper towel. Your older child can use hand sanitizer that contains alcohol if soap and water are not available.

- Remind your child to cover a sneeze or cough. Show your child how to use a tissue to cover his or her mouth and nose. Have your child throw the tissue away in a trash can right away. Then your child should wash his or her hands well or use a hand sanitizer. Show your child how to use the bend of his or her arm if a tissue is not available.
- Keep your child away from anyone who is sick. Have your child avoid crowds as much as possible. Ask anyone who is sick not to come to your home.
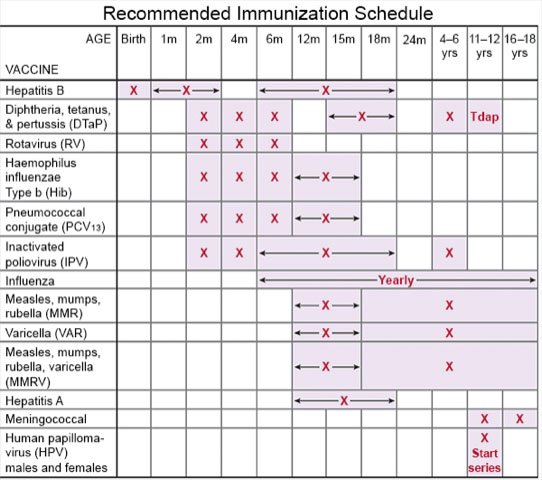
- Talk to your child's healthcare provider about vaccines. Vaccines can help prevent some lung infections. Examples include pneumonia, pertussis (whooping cough), diphtheria, and influenza (flu). Have your child get a flu vaccine every year as soon as recommended, usually starting in September or October. Children get vaccines on a regular schedule throughout childhood. Make sure your child receives all vaccines and booster shots. Schedule catch-up doses if your child misses any regular doses.
Call your local emergency number (911 in the US) if:
- Your child has sudden or more severe trouble breathing.
- Your child has severe chest pain.
When should I call my child's doctor?
- Your child coughs up blood.
- Your child is confused or feels faint.
- Your child has a fever.
- Your child coughs more than usual or wheezes.
- Your child's medicines do not relieve his or her symptoms.
- You have questions or concerns about your child's condition or care.
Care Agreement
You have the right to help plan your child's care. Learn about your child's health condition and how it may be treated. Discuss treatment options with your child's healthcare providers to decide what care you want for your child. The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
Learn more about Bronchiectasis
Treatment options
Care guides
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
