Bronchiectasis in Children
Medically reviewed by Drugs.com. Last updated on Aug 4, 2025.
Bronchiectasis is a condition that causes mucus to collect in your child's airway. Chronic respiratory infections or inflammation cause the bronchi to become thick. Bronchi are larger airways that help carry air in and out of your child's lungs. The lungs make mucus to trap and remove germs and irritants that your child breathes. Bronchiectasis prevents your child's lungs from clearing the mucus. This leads to more infections and inflammation, and scarring in the lungs.
 |
WHILE YOU ARE HERE:
Informed consent
is a legal document that explains the tests, treatments, or procedures that your child may need. Informed consent means you understand what will be done and can make decisions about what you want. You give your permission when you sign the consent form. You can have someone sign this form for you if you are not able to sign it. You have the right to understand your child's medical care in words you know. Before you sign the consent form, understand the risks and benefits of what will be done to your child. Make sure all of your questions are answered.
Medicines:
- Antibiotics help fight or prevent an infection caused by bacteria. Some antibiotics also help bring down swelling in your child's airway. He or she may get antibiotics as pills, through an IV, or breathed in through a nebulizer.
- Bronchodilators help open the air passages in your child's lungs.
- Expectorants help thin your child's mucus. Thin mucus may be easier to cough up.
- Steroids help decrease inflammation in your child's lungs and open his or her airway so he or she can breathe easier.
Tests:
- A sputum (mucus) sample is collected in a cup when your child coughs. The sample is sent to a lab to find out if he or she has an infection.
- X-ray or CT scan pictures are used to check your child's lungs and airway. Your child may be given contrast liquid to help these show up better in the pictures. Tell the healthcare provider if your child has ever had an allergic reaction to contrast liquid.
- Bronchoscopy is done to look inside your child's airway and lungs. Healthcare providers insert a bronchoscope (a tube with a light on the end) into your child's mouth and down into the lungs. Healthcare providers may also collect samples of sputum, fluid, or cells from your child's lungs for testing. This may help find the cause or see if he or she has an infection.
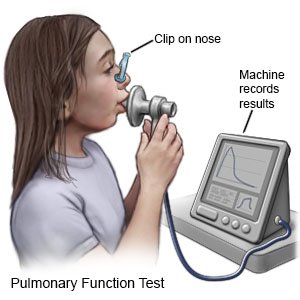
- Pulmonary function tests (PFTs) help healthcare providers learn how well your child's body uses oxygen. Your child breathes into a mouthpiece connected to a machine. The machine measures how much air he or she breathes in and out over a certain amount of time. PFTs help healthcare providers decide the best treatment for your child.
Treatment:
- Oxygen may be given through a mask or nasal cannula to help your child breathe easier. Oxygen can also decrease the strain on your child's heart and can help prevent more breathing problems.
- Surgery may be used to remove a part of your child's lung causing symptoms. Your child may also need a lung transplant if symptoms become severe. Surgery may also be needed to stop heavy bleeding if your child coughs up a lot of blood.
Treatment options
The following list of medications are related to or used in the treatment of this condition.
RISKS:
As more airway damage happens, your child may develop lung conditions such as respiratory failure. Pressure can grow in your child's pulmonary artery (blood vessel) and lead to heart failure. Respiratory or heart failure may be life-threatening.
CARE AGREEMENT:
You have the right to help plan your child's care. Learn about your child's health condition and how it may be treated. Discuss treatment options with your child's healthcare providers to decide what care you want for your child.© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.
Learn more about Bronchiectasis
Treatment options
Care guides
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
