A-Fib (Atrial Fibrillation)
Medically reviewed by Drugs.com. Last updated on Aug 4, 2025.
What is atrial fibrillation (A-fib)?
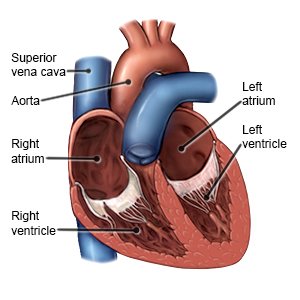
A-fib is an irregular heartbeat that reduces your heart's ability to pump blood through your body. A-fib may come and go, or it may be a long-term condition. A-fib can cause life-threatening blood clots, stroke, or heart failure. It is important to treat and manage A-fib to help prevent these problems.
 |
What increases my risk for A-fib?
- High blood pressure, heart failure, or heart valve disease
- Smoking
- COPD, sleep apnea, a blood clot in your lung, or other lung diseases
- Diabetes, obesity, or thyroid disease
- Heavy alcohol use or large amounts of caffeine
- Age 65 years or older
- A family history of A-fib or other heart problems
- Certain medicines, such as some antidepressants, bronchodilators, and cancer medicines
What are the signs and symptoms of A-fib?
- A heartbeat that races, pounds, or flutters
- Weakness, severe tiredness, or confusion
- Feeling lightheaded, sweaty, dizzy, or faint
- Shortness of breath or anxiety
- Chest pain or pressure
How is A-fib diagnosed?
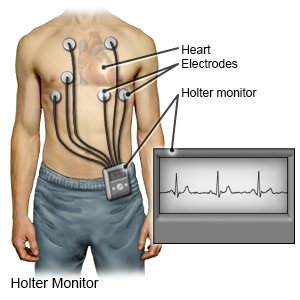
Your healthcare provider will examine you. Tell the provider about your symptoms, health conditions, and medicines. Tell the provider if you drink alcohol, smoke cigarettes, or use any illegal drugs. You will need an EKG to check your heart rhythm and how fast your heart beats. You may also need to wear a Holter monitor at home while you do your usual activities. The Holter monitor is a portable EKG machine.
 |
How is A-fib treated?
Conditions that cause A-fib, such as thyroid disease, will be treated. You may also need any of the following:
- Heart medicines help control your heart rate or rhythm. You may need more than 1 medicine to treat your symptoms.
- Antiplatelet or blood thinner medicines help prevent blood clots and stroke.
- Cardioversion is a procedure to return your heart rate and rhythm to normal. It can be done using medicines or electric shock.
- A-fib ablation is a procedure that uses energy to burn a small area of heart tissue. This creates scar tissue and prevents electrical signals that cause A-fib. You may need this procedure more than 1 time. Ask for more information on A-fib ablation.
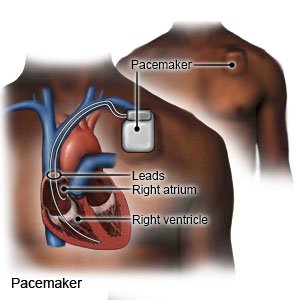
- A pacemaker may be inserted into your heart. A pacemaker is a device that controls your heartbeat. A pacemaker may be inserted during an ablation procedure or surgery. Ask your healthcare provider for more information on pacemakers.
- Surgery may be needed if other procedures do not work. During surgery your healthcare provider will make cuts in the upper part of your heart. The provider will stitch the cuts together to create scar tissue. The scar tissue will prevent electrical signals that cause A-fib.
Treatment options
The following list of medications are related to or used in the treatment of this condition.
How can I manage or prevent A-fib?
- Get screening for A-fib, if recommended. Screening means you are checked for A-fib, even if you do not have signs or symptoms. Screening can find problems early so treatment can begin. Early treatment can save your life. Your healthcare provider will talk to you about the benefits and risks of screening. Screening may be recommended starting at age 50. Your provider may recommend regular screenings if you stay at high risk for A-fib.
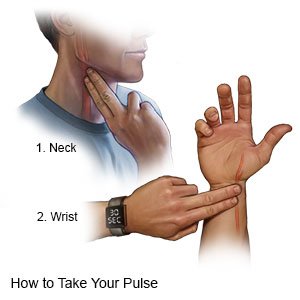
- Know your target heart rate. Learn how to check your pulse and monitor your heart rate.
- Know the risks if you choose to drink alcohol. Alcohol can increase your risk for A-fib or make A-fib harder to manage. Ask your provider if it is okay for you to drink any alcohol. Your provider can help you set limits for the number of drinks you have in 24 hours and in a week. A drink of alcohol is 12 ounces of beer, 5 ounces of wine, or 1½ ounces of liquor.
- Do not smoke. Nicotine can cause heart damage and make it more difficult to manage your A-fib. Do not use e-cigarettes or smokeless tobacco in place of cigarettes or to help you quit. They still contain nicotine. Ask your provider for information if you currently smoke and need help quitting.
- Eat heart-healthy foods. Heart healthy foods will help keep your cholesterol low. These include fruits, vegetables, whole-grain breads, low-fat dairy products, beans, lean meats, and fish. Replace butter and margarine with heart-healthy oils such as olive oil and canola oil.

- Maintain a healthy weight. Ask your provider what a healthy weight is for you. Your provider can help you create a safe weight loss plan, if needed. Even a small goal of a 10% weight loss can improve your heart health.
- Get regular physical activity. Physical activity helps improve your heart health. Get at least 150 minutes of moderate aerobic physical activity each week. Your provider can help you create an activity plan.

- Manage other health conditions. This includes high blood pressure or cholesterol, sleep apnea, diabetes, and other heart conditions. Take medicine as directed and follow your treatment plan. Your provider may need to change a medicine you are taking if it is causing your A-fib. Do not stop taking any medicine unless directed by your provider.
Call your local emergency number (911 in the US) or have someone call if:
- You have any of the following signs of a heart attack:
- Squeezing, pressure, or pain in your chest
- You may also have any of the following:
- Discomfort or pain in your back, neck, jaw, stomach, or arm
- Shortness of breath
- Nausea or vomiting
- Lightheadedness or a sudden cold sweat
- You have any of the following signs of a stroke:
- Numbness or drooping on one side of your face
- Weakness in an arm or leg
- Confusion or difficulty speaking
- Dizziness, a severe headache, or vision loss
When should I seek immediate care?
- Your arm or leg feels warm, tender, and painful. It may look swollen and red.
- Your heart rate is more than 110 beats per minute.
- You are short of breath, even at rest.
When should I call my doctor?
- You have new or worsening swelling in your legs, feet, ankles, or abdomen.
- You have questions or concerns about your condition or care.
Care Agreement
You have the right to help plan your care. Learn about your health condition and how it may be treated. Discuss treatment options with your healthcare providers to decide what care you want to receive. You always have the right to refuse treatment. The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
Learn more about A-Fib
Treatment options
Symptoms and treatments
Medicine.com guides (external)
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
