Metoclopramide Side Effects
Medically reviewed by Drugs.com. Last updated on Sep 13, 2024.
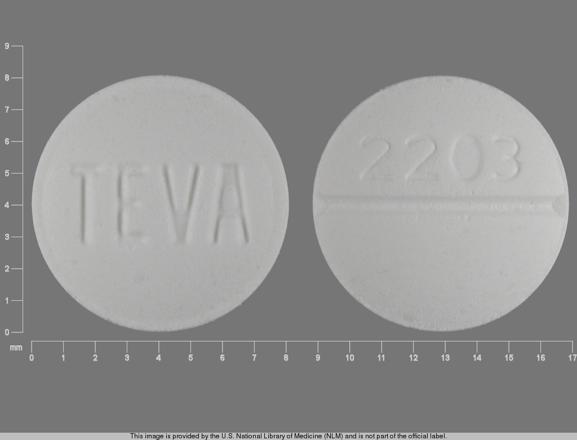
Applies to metoclopramide: oral solution, oral tablet, oral tablet disintegrating.
Other dosage forms:
Important warnings
This medicine can cause some serious health issues
Oral route (tablet)
Metoclopramide can cause tardive dyskinesia, a serious movement disorder that is often irreversible.
The risk of developing tardive dyskinesia increases with duration of treatment and total cumulative dose.
Discontinue metoclopramide in patients who develop signs or symptoms of tardive dyskinesia.
There is no known treatment for tardive dyskinesia.
In some patients, symptoms may lessen or resolve after metoclopramide is stopped.
Avoid treatment with Reglan for longer than 12 weeks because of the increased risk of developing TD with longer-term use.
Oral route (tablet, disintegrating; solution)
Metoclopramide treatment can cause tardive dyskinesia, a serious movement disorder that is often irreversible.
Risk is increased with duration of treatment and total cumulative dose.
Discontinue metoclopramide therapy in patients who develop signs or symptoms of tardive dyskinesia.
There is no known treatment for tardive dyskinesia, although symptoms may lessen or resolve after metoclopramide discontinuation.
Prolonged treatment with metoclopramide (greater than 12 weeks) should be avoided in all but rare cases where therapeutic benefit outweighs the risks.
Precautions
It is very important that your doctor check your progress at regular visits to make sure that this medicine is working properly. Blood tests may be needed to check for unwanted effects.
This medicine will add to the effects of alcohol and other CNS depressants (medicines that make you drowsy or less alert). Some examples of CNS depressants are antihistamines or medicine for hay fever or colds, sedatives, tranquilizers, or sleeping medicine, prescription pain medicine or narcotics, medicine for seizures or barbiturates, muscle relaxants, or anesthetics, including some dental anesthetics. Check with your doctor before taking any of these medicines while you are using metoclopramide.
This medicine may make you dizzy, drowsy, or have trouble with thinking or controlling body movements. Do not drive or do anything else that could be dangerous until you know how this medicine affects you.
This medicine may cause tardive dyskinesia (a movement disorder). Check with your doctor right away if you have any of the following symptoms while taking this medicine: lip smacking or puckering, puffing of the cheeks, rapid or worm-like movements of the tongue, uncontrolled chewing movements, or uncontrolled movements of the arms and legs. The risk of tardive dyskinesia is higher if you take this medicine for longer than 12 weeks. Treatment for longer than 12 weeks should be avoided in all but rare cases.
Tell your doctor right away if you have the following symptoms while you are using this medicine: inability to move the eyes, increased blinking or spasms of the eyelid, trouble with breathing, speaking, or swallowing, uncontrolled tongue movements, uncontrolled twisting movements of the neck, trunk, arms, or legs, unusual facial expressions, or weakness of the arms and legs.
Check with your doctor right away if you have any of the following symptoms while using this medicine: convulsions (seizures), difficulty with breathing, fast heartbeat, high fever, high or low blood pressure, increased sweating, loss of bladder control, severe muscle stiffness, unusually pale skin, or tiredness. These could be symptoms of a serious condition called neuroleptic malignant syndrome (NMS).
Metoclopramide may cause some people to be agitated, irritable, or display other abnormal behaviors. It may also cause some people to have suicidal thoughts and tendencies or to become more depressed. Also tell your doctor if you have sudden or strong feelings, such as feeling nervous, angry, restless, violent, or scared. If you or your caregiver notice any of these side effects, tell your doctor right away.
Your blood pressure might get too high while you are using this medicine. This may cause headaches, dizziness, or blurred vision. You might need to measure your blood pressure at home. If you think your blood pressure is too high, call your doctor right away.
This medicine may increase prolactin blood levels if used for a long time. Check with your doctor if you have breast swelling or soreness, unusual breast milk production, absent, missed, or irregular menstrual periods, stopping of menstrual bleeding, loss in sexual ability, desire, drive, or performance, decreased interest in sexual intercourse, or an inability to have or keep an erection.
You may also have dizziness, headaches, or nervousness when you Stop taking metoclopramide. These side effects should go away. Check with your doctor if any of the side effects continue or if you have any questions about them.
Do not take other medicines unless they have been discussed with your doctor. This includes prescription or nonprescription (over-the-counter [OTC]) medicines and herbal or vitamin supplements.
Common side effects of metoclopramide
Some side effects of metoclopramide may occur that usually do not need medical attention. These side effects may go away during treatment as your body adjusts to the medicine. Also, your health care professional may be able to tell you about ways to prevent or reduce some of these side effects.
Check with your health care professional if any of the following side effects continue or are bothersome or if you have any questions about them:
More common side effects
- diarrhea
- drowsiness
- loss of strength or energy
- muscle pain or weakness
- restlessness
- unusual weak feeling
Incidence not known
- breast tenderness and swelling
- changes in menstruation
- constipation
- decreased interest in sexual intercourse
- inability to have or keep an erection
- increased flow of breast milk
- increased need to urinate
- loss in sexual ability, desire, drive, or performance
- mental depression
- passing urine more often
- skin rash
- trouble sleeping
- unusual dryness of the mouth
- unusual irritability
Serious side effects of metoclopramide
Along with its needed effects, metoclopramide may cause some unwanted effects. Although not all of these side effects may occur, if they do occur they may need medical attention.
Check with your doctor immediately if any of the following side effects occur while taking metoclopramide:
Incidence not known
- chills
- clay colored stools
- dark urine
- difficulty with breathing
- difficulty with speaking or swallowing
- dizziness or fainting
- fast or irregular heartbeat
- fever
- general feeling of tiredness or weakness
- headache (severe or continuing)
- inability to move the eyes
- increase in blood pressure
- increased sweating
- itching, skin rash
- lip smacking or puckering
- loss of appetite
- loss of balance control
- loss of bladder control
- mask-like face
- muscle spasms of the face, neck, and back
- nausea
- puffing of the cheeks
- rapid or worm-like movements of the tongue
- seizures
- shuffling walk
- sore throat
- stiffness of the arms or legs
- stomach pain or tenderness
- swelling of the feet or lower legs
- tic-like or twitching movements
- trembling and shaking of the hands and fingers
- twisting movements of the body
- uncontrolled chewing movements
- uncontrolled movements of the arms and legs
- unusually pale skin
- vomiting
- weakness of the arms and legs
- yellow eyes or skin
Get emergency help immediately if any of the following symptoms of overdose occur while taking metoclopramide:
Symptoms of overdose
- confusion
- drowsiness (severe)
See also:
For healthcare professionals
Applies to metoclopramide: compounding powder, injectable solution, nasal spray, oral concentrate, oral syrup, oral tablet, oral tablet disintegrating.
General adverse events
The incidence of side effects correlates with dose and duration of metoclopramide therapy.[Ref]
Nervous system
- Very common (10% or more): Drowsiness (up to 70%), acute dystonic reaction (up to 25%)
- Common (1% to 10%): Akathisia, dizziness, extrapyramidal disorders, headache, parkinsonism, somnolence
- Uncommon (0.1% to 1%): Depressed level of consciousness, dyskinesia, dystonia
- Rare (0.01% to 0.1%): Bradykinesia, convulsion, dystonic reaction, tremor
- Very rare (less than 0.01%): Neuroleptic malignant syndrome
- Frequency not reported: Acute dyskinesia, acute dystonia/acute dystonic reaction, altered consciousness, autonomic instability, bulbar type of speech, choreoathetotic movements, cogwheel rigidity, convulsive seizures, extrapyramidal symptoms, facial grimacing, facial muscle spasm, fatal dystonic reaction, foot tapping, inability to sit still, involuntary movements of the extremities/face/jaw/mouth/tongue/trunk, mask-like facies, motor restlessness, opisthotonos, pacing, parkinsonian syndrome, rhythmic tongue protrusion, serotonin syndrome, syncope, tardive dyskinesia, tetanus-like reaction, unnatural position of head and shoulders[Ref]
Drowsiness, decreased level of consciousness, confusion, and hallucinations have higher incidences with higher doses.
Convulsive seizures have been reported, especially in patients with epilepsy; however, there is no obvious association with use of this drug.
Dystonic reactions typically presented as upper airway obstruction with stridor and dyspnea.
Parkinsonian symptoms may be related to usual/excessive doses and/or decreased renal function and includes tremor, rigidity, bradykinesia, and akinesia.[Ref]
Gastrointestinal
- Common (1% to 10%): Diarrhea, nausea, vomiting
- Uncommon (0.1% to 1%): Bowel disturbances
- Rare (0.01% to 0.1%): Supraglottic dystonia
- Frequency not reported: Glossal edema[Ref]
Other
- Common (1% to 10%): Asthenia, fatigue, lassitude
- Frequency not reported: Effects on the ability to drive/operate machinery, hyperpyrexia, hyperthemia, jitteriness[Ref]
Psychiatric
- Common (1% to 10%): Depression, restlessness
- Uncommon (0.1% to 1%): Hallucination, insomnia
- Rare (0.01% to 0.1%): Acute depression, confusional state
- Frequency not reported: Agitation, anxiety, confusion, delirium, mania, mental depression with suicidal ideation, nervousness, obsessive rumination, severe dysphoria, suicidal ideation, suicide[Ref]
Cardiovascular
- Common (1% to 10%): Hypotension
- Uncommon (0.1% to 1%): Bradycardia
- Very rare (less than 0.01%): Cardiac conduction abnormalities, heart block
- Frequency not reported: Acute congestive heart failure, acute hypertension, atrial fibrillation, atrioventricular (AV) block, cardiac arrest, edema, electrocardiogram QT prolonged, fatal cardiorespiratory arrest, hypertension, palpitation, possible AV block, shock, sinus arrest, supraventricular tachycardia, tachycardia, Torsade de Pointes, transient facial/upper body flushing, transient increase in blood pressure, ventricular fibrillation, ventricular tachycardia[Ref]
Hypotension, bradycardia, shock, and other abnormalities or cardiac conduction occurred most frequently with IV formulations.
Cardiac arrest occurred shortly after IV administration, and may have been subsequent to bradycardia.
Sinus arrest and transient facial/upper body flushing occurred, particularly with IV administration. Flushing typically occurred without alterations in vital signs following high dose IVs.
Edema/fluid retention may be secondary to a transient increase in aldosterone levels.
Acute hypertension has occurred in patients with pheochromocytoma.
Hypertension has occurred in patients with/without pheochromocytoma.[Ref]
Genitourinary
- Uncommon (0.1% to 1%): Amenorrhea
- Rare (0.01% to 0.1%): Galactorrhea
- Frequency not reported: Breast enlargement, impotence, priapism, sexual dysfunction, urinary frequency, urinary incontinence[Ref]
Impotence may be secondary to hyperprolactinemia.[Ref]
Endocrine
- Uncommon (0.1% to 1%): Hyperprolactinemia
- Frequency not reported: Endocrine disorders, gynecomastia, transient aldosterone elevation[Ref]
Amenorrhea, galactorrhea, and gynecomastia occurred secondary to hyperprolactinemia during prolonged treatment.[Ref]
Hypersensitivity
- Uncommon (0.1% to 1%): Hypersensitivity
- Frequency not reported: Anaphylactic reaction, anaphylactic shock, angioedema[Ref]
Anaphylactic reaction/shock typically occurred with the IV formulation.[Ref]
Respiratory
- Rare (0.01% to 0.1%): Dyspnea, laryngospasm, stridor, upper airway obstruction
- Frequency not reported: Acute asthmatic symptoms, bronchospasm, laryngeal edema, respiratory failure, wheezing[Ref]
Bronchospasm, wheezing, and dyspnea typically occurred in patients with a history of asthma.
Respiratory failure occurred secondary to dystonic reactions.[Ref]
Hepatic
- Rare (0.01% to 0.1%): Altered liver function tests, hepatotoxicity, jaundice[Ref]
Hepatotoxicity occurred with concurrent use of other potentially hepatotoxic drugs and was characterized by findings such as jaundice and altered liver function tests.[Ref]
Musculoskeletal
- Rare (0.01% to 0.1%): Rigidity
- Frequency not reported: Fluid retention, generalized muscle tone increase, increased creatinine phosphokinase (CPK), muscle rigidity, muscle spasms, torticollis, trismus[Ref]
Hematologic
- Frequency not reported: Agranulocytosis, blood disorders, leukopenia, methemoglobinemia, neutropenia, sulfhemoglobinemia[Ref]
Leukopenia, neutropenia, and agranulocytosis typically did not have a clear-cut relationship with this drug.
Methemoglobinemia and sulfhemoglobinemia occurred with high doses of this drug. Methemoglobinemia may be related to NADH cytochrome b5 reductase deficiency or overdose, particularly in neonates. Sulfhemoglobinemia usually occurred in adults with concomitant use of high doses of sulfur-releasing products.[Ref]
Dermatologic
- Frequency not reported: Angioneurotic edema, maculopapular rash, rash, urticaria[Ref]
Rash and urticaria typically occurred in patients with a history of asthma.[Ref]
Ocular
- Frequency not reported: Extraocular muscle spasm, oculogyric crisis, visual disturbances[Ref]
Metabolic
- Frequency not reported: Fluid retention, porphyria[Ref]
References
1. (2001) "Product Information. Reglan (metoclopramide)." Wyeth-Ayerst Laboratories
2. Cerner Multum, Inc. "UK Summary of Product Characteristics."
3. Cerner Multum, Inc. "Australian Product Information."
More about metoclopramide
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (524)
- Drug images
- Dosage information
- Patient tips
- During pregnancy
- Drug class: GI stimulants
- Breastfeeding
Patient resources
- Metoclopramide drug information
- Metoclopramide nasal
- Metoclopramide (Injection, Intravenous) (Advanced Reading)
Other brands
Professional resources
- Metoclopramide monograph
- Metoclopramide Injection (FDA)
- Metoclopramide Oral Solution (FDA)
- Metoclopramide Orally DisintegratingTablets (FDA)
- Metoclopramide Tablets (FDA)
Other brands
Related treatment guides
Further information
Metoclopramide side effects can vary depending on the individual. Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
Note: Medication side effects may be underreported. If you are experiencing side effects that are not listed, submit a report to the FDA by following this guide.