Febuxostat (Monograph)
Brand name: Uloric
Drug class: Antigout Agents
VA class: MS400
Chemical name: 2-[3-cyano-4-(2-methylpropoxy) phenyl]-4-methylthiazole-5-carboxylic acid
Molecular formula: C16H16N2O3S
CAS number: 144060-53-7
Warning
-
In a postmarketing outcome study in patients with coexisting gout and cardiovascular disease, cardiovascular mortality was higher in those receiving febuxostat compared with those receiving allopurinol. (See Cardiovascular Death under Cautions.)
-
Reserve febuxostat use for patients with an inadequate response to maximum recommended dosages of allopurinol or in whom allopurinol is not tolerated or is not recommended; evaluate risks and benefits of initiating or continuing febuxostat therapy.
Introduction
Xanthine oxidase inhibitor.
Uses for Febuxostat
Gout
Long-term management of hyperuricemia in patients with gout who have had an inadequate response to maximum recommended dosages of allopurinol or in whom allopurinol is not tolerated or is not recommended. (See Cardiovascular Death under Cautions.)
Goal in management of gout is reduction in serum urate concentrations to levels below the limit of urate solubility (about 6.8 mg/dL).
Not recommended for the management of asymptomatic hyperuricemia.
Febuxostat Dosage and Administration
General
-
Acute gout attacks (gout flare) may occur after initiation of febuxostat. Consider gout flare prophylaxis with an NSAIA or colchicine; start these agents when febuxostat therapy is initiated. Gout flare prophylaxis may be beneficial for up to 6 months. During these acute attacks, continue febuxostat and manage the gout flare as appropriate.
-
Testing for target serum urate concentrations can be performed after 2 weeks of febuxostat therapy.
Administration
Oral Administration
Administer orally without regard to meals or antacids.
Dosage
Adults
Gout
Oral
Initial dosage is 40 mg once daily. Increase dosage to 80 mg once daily in patients who do not achieve serum urate concentrations of <6 mg/dL after 2 weeks of therapy with febuxostat 40 mg once daily.
Special Populations
Hepatic Impairment
Dosage adjustment not necessary in patients with mild to moderate hepatic impairment (Child-Pugh class A or B). Manufacturer makes no specific dosage recommendations for patients with severe hepatic impairment (Child-Pugh class C). (See Hepatic Impairment under Cautions.)
Renal Impairment
Dosage adjustment not necessary in patients with mild to moderate renal impairment (Clcr 30–89 mL/minute). In patients with severe renal impairment (Clcr 15–29 mL/minute), maximum 40 mg once daily. (See Renal Impairment under Cautions.)
Geriatric Patients
Dosage adjustment not necessary. (See Geriatric Use under Cautions.)
Cautions for Febuxostat
Contraindications
-
Concomitant therapy with azathioprine or mercaptopurine. (See Interactions.)
Warnings/Precautions
Warnings
Cardiovascular Death
Results from a postmarketing study (CARES) in patients with coexisting gout and cardiovascular disease indicate higher cardiovascular mortality (4.3 versus 3.2%) and overall mortality (7.8 versus 6.4%) in patients receiving febuxostat compared with those receiving allopurinol. All patients had a history of major cardiovascular disease (e.g., MI, unstable angina or TIA requiring hospitalization, stroke, peripheral vascular disease, diabetes mellitus with microvascular or macrovascular disease). Cardiovascular mortality generally resulted from sudden cardiac death.
In the CARES study, incidence of major cardiovascular events (e.g., nonfatal MI, unstable angina requiring urgent coronary revascularization, nonfatal stroke) was similar in febuxostat- and allopurinol-treated patients.
Reserve febuxostat for use in patients who have had an inadequate response to maximum recommended dosages of allopurinol or in whom allopurinol is not tolerated or is not recommended; consider risks and benefits of initiating or continuing febuxostat therapy.
Monitor for signs and symptoms of adverse cardiovascular events. Consider prophylactic low-dose aspirin therapy in patients with a history of cardiovascular disease.
Sensitivity Reactions
Dermatologic and Hypersensitivity Reactions
Serious dermatologic reactions (e.g., Stevens-Johnson syndrome, erythema multiforme, toxic epidermal necrolysis, drug reaction with eosinophilia and systemic symptoms [DRESS]) and hypersensitivity reactions reported.
Many patients reporting dermatologic reactions to febuxostat also reported similar reactions to prior allopurinol therapy. Use with caution in patients with history of dermatologic reactions to allopurinol.
Discontinue febuxostat if serious dermatologic reactions suspected. (see Advice to Patients)
Other Warnings and Precautions
Acute Gout
Febuxostat initiation may increase frequency of acute gout attacks (gout flare). Consider gout flare prophylaxis with an NSAIA or colchicine; start these agents when febuxostat therapy is initiated.
Hepatic Effects
Fatal and nonfatal hepatic failure reported; causal relationship to drug cannot be excluded. Elevations of serum aminotransferase concentrations also reported.
Perform liver function tests (serum ALT, AST, alkaline phosphatase, and total bilirubin concentrations) prior to initiation of therapy and repeat promptly in patients with manifestations suggestive of liver damage (see Advice to Patients). Interrupt therapy if ALT >3 times the ULN and investigate the cause. Treat the cause, if possible, to resolution or stabilization. If an alternate etiology is not found, do not restart febuxostat.
Risk for severe drug-related liver injury if no alternate etiology is found and ALT is >3 times the ULN with total bilirubin concentrations >2 times the ULN; do not restart febuxostat in these patients. Manufacturer states that febuxostat may be used with caution in patients with lesser elevations of ALT or bilirubin if an alternate probable cause of liver function test abnormalities determined.
Specific Populations
Pregnancy
Data are inadequate regarding use of febuxostat in pregnant women.
Animal studies revealed no evidence of fetal harm at exposures greater than those achieved with maximum recommended human dosage.
Lactation
Distributed into milk in rats. Not known whether febuxostat distributes into human milk, affects human milk production, or affects breast-fed infant.
Consider benefits of breast-feeding and importance of the drug to the woman; also consider any potential adverse effects on the breast-fed infant from the drug or underlying maternal condition.
Pediatric Use
Safety and efficacy not established in pediatric patients.
Geriatric Use
No substantial differences in safety and efficacy relative to younger adults, but increased sensitivity of some older patients cannot be ruled out.
Hepatic Impairment
Not studied in patients with severe hepatic impairment (Child-Pugh class C); caution if used in these individuals. Dosage adjustment not needed in patients with mild to moderate hepatic impairment (Child-Pugh class A or B).
Renal Impairment
Increased systemic exposure in patients with severe renal impairment; dosage adjustment recommended. Dosage adjustment not needed in patients with mild to moderate renal impairment. (See Renal Impairment under Dosage and Administration and see Special Populations under Pharmacokinetics: Absorption and Pharmacokinetics: Elimination.)
Not studied in individuals with end-stage renal disease who are undergoing dialysis.
Secondary Hyperuricemia
Not evaluated in patients with secondary hyperuricemia. Not recommended in patients whose rate of urate formation is greatly increased.
Common Adverse Effects
Liver function abnormalities, nausea, arthralgia, rash.
Drug Interactions
Does not inhibit CYP isoenzymes 1A2, 2C9, 2C19, or 3A4; weakly inhibits CYP2D6. Does not induce CYP 1A2, 2B6, 2C9, 2C19, or 3A4.
Metabolized by UGT enzymes, including UGT 1A1, 1A3, 1A9, and 2B7; CYP isoenzymes, including CYP 1A2, 2C8, and 2C9; and non-CYP enzymes. Relative contribution of each enzyme isoform to the drug’s metabolism is not clear.
Drugs Affecting Hepatic Microsomal or Other Enzymes
Drug interactions generally are not expected between febuxostat and inhibitors or inducers of particular enzyme isoforms.
Drugs Metabolized by Hepatic Microsomal Enzymes
Pharmacokinetic interactions are unlikely between febuxostat and substrates of these isoenzymes.
Drugs Metabolized by Xanthine Oxidase
Inhibition of xanthine oxidase by febuxostat may increase plasma concentrations of drugs metabolized by the enzyme, resulting in toxicity. (See Contraindications under Cautions.)
Specific Drugs
|
Drug |
Interaction |
Comments |
|---|---|---|
|
Antacids |
Pharmacokinetic interaction unlikely |
|
|
Antineoplastic agents |
Not evaluated Mercaptopurine: Possible inhibition of mercaptopurine metabolism; possible increase in toxic effects |
No information on safety of concomitant use Mercaptopurine: Concomitant use contraindicated |
|
Azathioprine |
Possible inhibition of azathioprine metabolism; possible increase in toxic effects |
Concomitant use contraindicated |
|
Colchicine |
Clinically important pharmacokinetic interaction unlikely |
Dosage adjustment not needed |
|
Desipramine |
Pharmacokinetic interaction not considered clinically important |
Dosage adjustment not expected to be necessary |
|
Hydrochlorothiazide |
Clinically important pharmacokinetic interaction unlikely |
Dosage adjustment not needed |
|
Indomethacin |
Clinically important pharmacokinetic interaction unlikely |
Dosage adjustment not needed |
|
Naproxen |
Clinically important pharmacokinetic interaction unlikely |
Dosage adjustment not needed |
|
Theophylline |
Urinary excretion of 1-methylxanthine (major metabolite of theophylline) increased by approximately 400-fold; no effect on theophylline peak concentration or AUC |
Use concomitantly with caution; dosage adjustment of theophylline not necessary Long-term safety of 1-methylxanthine exposure not known |
|
Warfarin |
Pharmacokinetic interaction unlikely |
Dosage adjustment not needed |
Febuxostat Pharmacokinetics
Absorption
Bioavailability
Peak plasma concentrations of febuxostat are reached in 1–1.5 hours.
Food
Administration with food decreases the rate and extent of absorption of febuxostat; not considered clinically important.
Special Populations
Mild to moderate hepatic impairment: Peak concentrations and AUC are increased by 20–30%; not considered clinically important.
Mild or moderate renal impairment: AUC is increased by 7–18 or 45–49%, respectively; not considered clinically important.
Severe renal impairment: AUC is increased by 96–98%.
Distribution
Plasma Protein Binding
99.2%.
Elimination
Metabolism
Metabolized by conjugation by UGT 1A1, 1A3, 1A9, and 2B7; oxidation by CYP 1A2, 2C8, and 2C9; and metabolism by other enzymes.
Elimination Route
Excreted in urine (49%) and feces (45%), principally as metabolites.
Half-life
5–8 hours.
Special Populations
Pharmacokinetic values in geriatric adults similar to those in younger adults.
Mild, moderate, or severe renal impairment: Clearance is decreased 14, 34, or 48%, respectively.
Stability
Storage
Oral
Tablets
25°C (may be exposed to 15–30°C).
Actions
-
Febuxostat inhibits xanthine oxidase, the enzyme that catalyzes the conversion of hypoxanthine to xanthine and xanthine to uric acid. By blocking uric acid production, febuxostat decreases serum concentrations of uric acid.
-
Febuxostat has minimal effects on other enzymes involved in purine and pyrimidine synthesis and metabolism.
Advice to Patients
-
Importance of reading patient information (medication guide) provided by the manufacturer.
-
Importance of informing patients that higher cardiovascular mortality reported with febuxostat compared with allopurinol therapy in patients with gout and established cardiovascular disease. Instruct all patients, including those without cardiovascular disease, to be alert for the development of signs and symptoms of cardiovascular events (e.g., chest pain, shortness of breath, rapid or irregular heartbeat, symptoms suggestive of stroke).
-
Importance of informing patients that gout flares may initially increase when starting treatment with febuxostat and that medications to help reduce flares may be taken regularly for the first few months after initiation. Advise patients that they should not discontinue febuxostat therapy if such flares occur.
-
Risk of adverse hepatic effects. Importance of promptly reporting any symptoms suggestive of liver injury (e.g., fatigue, anorexia, right upper abdominal discomfort, dark urine, jaundice).
-
Risk of severe dermatologic or hypersensitivity reactions. Importance of notifying clinician at the earliest onset of any manifestations of severe dermatologic or hypersensitivity reactions (e.g., rash; red and painful skin; peeling or blistering of the skin; swelling or blistering of the lips, eyes, or mouth; difficulty swallowing or breathing).
-
Importance of informing clinicians of existing or contemplated concomitant therapy, including prescription and OTC drugs and herbal products and any concomitant illnesses (e.g., cardiovascular or cerebrovascular disease).
-
Importance of women informing clinicians if they are or plan to become pregnant or plan to breast-feed.
-
Importance of advising patients of other important precautionary information. (See Cautions.)
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
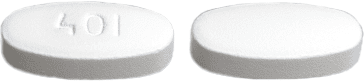
Oral |
Tablets |
40 mg |
Uloric |
Takeda |
|
80 mg |
Uloric |
Takeda |
AHFS DI Essentials™. © Copyright 2025, Selected Revisions November 18, 2019. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
Reload page with references included
Related/similar drugs
Zyloprim
Zyloprim is used for calcium oxalate calculi with hyperuricosuria, gout, hyperuricemia secondary to ...
Uloric
Uloric (febuxostat) reduces the production of uric acid in your body and is used to treat gout ...
Botox
Botox is used for cosmetic purposes and to treat overactive bladder symptoms, urinary incontinence ...
Krystexxa
Krystexxa (pegloticase) is an enzyme that metabolizes uric acid and is used to treat chronic gout ...
Benemid
Benemid is used for adjunct to antibiotic therapy, gout, gouty arthritis
Probenecid
Probenecid is used for adjunct to antibiotic therapy, gout, gouty arthritis
Allopurinol
Allopurinol is used to treat gout or kidney stones, and to decrease levels of uric acid in certain ...
More about febuxostat
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (63)
- Drug images
- Side effects
- Dosage information
- During pregnancy
- Drug class: antihyperuricemic agents
- Breastfeeding
- En español