Quinine
Scientific Name(s): Cinchona calisya Wedd., Cinchona ledgeriana Moens ex Trim. (yellow cinchona), Cinchona succirubra Pav. ex Klotsch (red cinchona)
Common Name(s): China bark, Cinchona bark, Fever tree, Jesuit's bark, Peruvian bark, Quina-quina, Red bark
Clinical Overview
Use
Quinine has been used for the treatment of malaria and associated febrile states, leg cramps caused by vascular spasm, internal hemorrhoids, varicose veins, and pleural cavities after thoracoplasty.
Dosing
Quinine has been widely studied as an antimalarial, and has been used at doses of 325 mg to 1 g as the sulfate salt. Classical doses of the crude bark were approximately 1 g.
Contraindications
Contraindications have not yet been identified.
Pregnancy/Lactation
Quinine has been previously listed as being contraindicated during pregnancy because of fetal and abortifacient effects.1 A review of the safety of antimalarial drugs in pregnancy state that standard (antimalarial) doses of quinine showed no evidence of increased risk of abortion or preterm delivery. Quinine has been shown to be secreted into breast milk, but insignificant amounts are ingested by the infant. However, high doses of quinine can cause uterine stimulation in pregnant women and deafness and optic nerve hypoplasia in children.2
Interactions
Rifamycins and cigarette smoking increase the elimination of quinine.3, 4, 5, 6, 7 Cimetidine3, 6 and ketoconazole4, 6 decrease the clearance of quinine. Serum levels of amantadine, carbamazepine, digoxin, phenobarbital, and warfarin may be elevated by quinine.3, 6, 8, 9 Quinine may enhance the effects of nondepolarizing muscle relaxants and succinylcholine. Close monitoring of neuromuscular function is required.6 Dosage adjustment may be necessary. For additional information please refer to the "Evidence-Based Herb-Drug Interactions" appendix.
Adverse Reactions
Quinine can cause cinchonism, hypoglycemia, serious hematologic disorders, urticaria, contact dermatitis, and other hypersensitivity reactions.
Toxicology
Quinine is rapidly absorbed from the GI tract and toxicity is dose related. Treatment of an overdose is generally supportive.
Scientific Family
- Rubiaceae
Botany
The cinchonas are evergreen shrubs and trees that grow to heights of 15 to 31 m.10 They are native to the mountainous areas of tropical Central and South America, including regions of Bolivia, Costa Rica, and Peru. The oblong seed capsule is about 3 cm long and, when ripe, splits open at the base. Each capsule contains 40 to 50 slender seeds that are so light that approximately 75,000 seeds equal 30 g.11 In addition, these trees are found in cultivation in Africa and Southeast Asia.10, 12 At least one other genus (Remijia) of the same family has been reported to contain quinidine.13
History
The dried ground bark of the cinchona plant has been used for centuries for the treatment of malaria, fever, indigestion, mouth and throat diseases, and cancer.10, 11, 12 The name cinchona is said to be derived from the Countess of Chinchon, the wife of a viceroy of Peru, who it was long believed was cured in 1638 from a fever by the use of the bark;13 however, the story has been widely disputed. Formal use of the bark to treat malaria was established in the mid-1800s when the British began the worldwide cultivation of the plant11 in order to assure the continuing availability because the plant was in danger of extinction in some regions because of the harvesting of wild populations.13
Extracts of the bark have been used to treat hemorrhoids, to stimulate hair growth, and to manage varicose veins. Quinine has been used as an abortifacient.11 Extracts of cinchona have a bitter, astringent taste and have been used as flavoring for foods and beverages. Although the use of quinine for the treatment of malaria has been largely supplanted by semisynthetic antimalarials, its use persists in some regions of the world.
Chemistry
Typical cinchona bark contains about 16% of quinoline alkaloids consisting mainly of quinine, quinidine, cinchonine, and cinchonidine. The primary component of this mixture is quinine. Quinidine is the dextrorotatory isomer of quinine. Approximately 35 additional minor compounds related to quinine have been identified in the plant.10, 11 As a rule, the yellow cinchona has a higher alkaloid content than other varieties. Commercial formulations of quinine contain about 10% of dihydroquinine as an impurity.3
The cinchona alkaloids are extremely bitter tasting. Concentrations in the 100 to 300 ppm range are used to flavor beverages such as tonic water. Tonic water contains about 15 mg of quinine per bottle.14 Quinine may have tumor necrosis factor (TNF)-suppressive activity as demonstrated in one small study.8
Uses and Pharmacology
Quinine is eliminated mainly by hepatic metabolism with very little excreted unchanged in the urine.4, 5, 15 Cytochrome P450 3A4 has been shown to be important in the metabolism of quinine. Seven metabolites have been identified with 3-hydroxyquinine being the major metabolite.3, 4, 5, 16 In patients with acute renal failure who are infected with Plasmodium falciparum, up to 12% of antimalarial activity is due to the 3-hydroxyquinine metabolite.16
Antimalarial
Quinine is among the most potent of the cinchona alkaloids with respect to antimalarial activity.10 Resistant strains of Plasmodium have been identified. A small, in vitro study showed potential of phenobarbital to partially reverse quinine resistance.17 Calcium antagonists and other agents (eg, prochlorperazine) are being studied for reversing P. falciparum resistance to quinine.18 Various antibiotics (ie, artemisinin, artemether, clindamycin, doxycycline, mefloquine) in combination with quinine are being tested and used to treat resistant strains of P. falciparum.19, 20, 21, 22, 23, 24 If the oral route is not available for administration of quinine in children, effective alternate routes (ie, IM, intrarectal, IV) can be used.25, 26, 27, 28 Close monitoring for adverse reactions is advised, especially in young children who are more susceptible to quinine toxicity.26 The combination of quinine and clindamycin has been safely and effectively used in Thailand for the treatment of uncomplicated malaria.29
Antipyretic
Quinine has been thought to have antipyretic action.1 Although quinine administered before acetaminophen produces a more rapid drop in temperature than administration after acetaminophen, quinine alone has no effect on fever.30
Leg and other muscle cramps
Another common use of quinine has been for the treatment of leg cramps caused by vascular spasm. For more than 50 years, quinine, quinidine, and hydroquinine have been used to prevent muscle cramps.31 However, because 157 adverse drug reactions attributed to quinine were reported from 1969 to 1992, the Food and Drug Administration (FDA) concluded that quinine was not safe for use in this condition.32 In 1994, the FDA prohibited the marketing of quinine for nocturnal leg cramps and discontinued its availability and the labeling of products for this use in prescription and nonprescription form. 32, 33 However, a quick search of the Internet found a multitude of quinine preparations available and advertised for leg cramps.34
Clinical data
Various crossover, randomized trials, and 2 meta-analyses have confirmed that quinine is effective in the prevention of nocturnal leg cramps.31, 35, 36, 37
A Report of the Therapeutics and Technology Assessment Subcommittee of the American Academy of Neurology regarding the management of muscles cramps (2010) states that the use of quinine derivatives for treatment of muscle cramps is likely effective based on controlled studies; however, it should be avoided for routine treatment of cramps. According to this report, quinine should only be considered when cramps are very disabling, no other agents relieve symptoms, and there is careful monitoring of side effects. They should only be used after informing the patient of the potentially serious side effects.61
Other uses
Quinine is bacteriostatic, highly active in vitro against protozoa, and inhibits the fermentation of yeast.11
Quinine and quinidine have cardiodepressant activity. The latter compound is used for its antiarrhythmic activity.
A mixture of quinine and urea hydrochloride is injected as a sclerosing agent in the treatment of internal hemorrhoids, varicose veins, and pleural cavities after thoracoplasty.11
Quinine has been used to reverse multidrug resistance in patients with acute leukemias who express a higher incidence of P glycoprotein expression in blast cells. A high cure rate and better survival were shown in patients treated with combined quinine and chemotherapy when compared with chemotherapy alone. Although a higher incidence of side effects occurred, this combination has potential in treating acute leukemias.6, 38
Dosing
Quinine has been widely studied as an antimalarial, and has been used at doses of 325 mg to 1 g as the sulfate salt. Classical doses of the crude bark were approximately 1 g.
Pregnancy / Lactation
Quinine has been previously listed as being contraindicated during pregnancy because of fetal and abortifacient effects.1 A review of the safety of antimalarial drugs in pregnancy state that standard (antimalarial) doses of quinine showed no evidence of increased risk of abortion or preterm delivery. Quinine has been shown to be secreted into breast milk, but insignificant amounts are ingested by the infant. However, high doses of quinine can cause uterine stimulation in pregnant women and deafness and optic nerve hypoplasia in children.2
Interactions
Amantadine
In a randomized crossover study, administration of a single oral 200 mg dose of quinine decreased the renal clearance of a single oral dose of amantadine (3 mg/kg), increasing the plasma concentrations, in men but not women.39
Carbamazepine
The effect of a single 600 mg oral dose of quinine on the pharmacokinetics of a 200 mg oral dose of carbamazepine was studied in 6 healthy volunteers.40 Compared with giving carbamazepine alone, quinine administration increased the carbamazepine area under the plasma concentration-time curve (AUC) and peak plasma concentration 51% and 36.5%, respectively.
Nondepolarizing muscle relaxants
A 47-year-old patient receiving quinine (1800 mg daily) developed recurarization after reversal from anesthesia and administration of pancuronium (6 mg).7
Phenobarbital
The effect of a single 600 mg oral dose of quinine on the pharmacokinetics of a 120 mg oral dose of phenobarbital was studied in 6 healthy volunteers.40 Compared with giving phenobarbital alone, quinine administration increased the phenobarbital AUC and peak plasma concentration 45% and 35%, respectively.
Warfarin
There is no report of an interaction occurring with coadministration of quinine and warfarin. However, in healthy subjects, quinine (330 mg) administration prolonged the prothrombin time (form 5 to 11.8 seconds)41 and reduced the prothrombin content in blood in a patient receiving dicumarol (not available in the US).42 A similar interaction may be expected to occur with coadministration of quinine and warfarin.
Adverse Reactions
Quinine exhibits considerable inter- and intraindividual variations in metabolism and elimination, with differences also seen in healthy compared with malaria-infected patients. Adverse effects are dose-related.43
Cardiac events
Because quinine is related to quinidine, ventricular fibrillation, prolongation of the QTc interval, and other adverse cardiac events can occur.18 Administration of IV quinine within 72 hours of mefloquine may cause QTc prolongation.22 Closely monitor patients with a cardiac history if quinine is given.
Cinchonism
The ingestion of these alkaloids can result in the clinical syndrome known as cinchonism. People who are hypersensitive to these alkaloids also may develop the syndrome, which is characterized by severe headache, abdominal pain, convulsions, visual disturbances and blindness, auditory disturbances such as ringing in the ears, paralysis, and collapse.10
Hematologic disorders
Therapeutic doses of quinine have resulted in acute hemolytic anemia12 a limitation for its use in patients who are glucose-6-phosphate dehydrogenase deficient.3 Quinine also has been associated with other serious hematologic disorders such as agranulocytosis, disseminated intravascular coagulation44, 45 hemolytic uremic syndrome (HUS)16, 44, 46, 47, 48, 49 neutropenia (leukopenia)50 pancytopenia with coagulopathy51, 52 and thrombocytopenia (the most common hematologic adverse effect).50, 53, 54, 55 Patients may present with one or several concomitant hematologic adverse events. Two deaths have been attributed to quinine-induced thrombocytopenia.53, 55
Hypersensitivity reactions
Ground cinchona bark and quinine have been reported to cause urticaria, contact dermatitis, and other hypersensitivity reactions. These reactions also may occur with the use of topical preparations containing cinchona extracts or quinine.11
Systemic hypersensitivity reactions can present as HUS, with acute renal failure and simulating sepsis.16, 49
Hypoglycemia
Children with severe malaria often present with hypoglycemia.56 Quinine has been shown to increase insulin secretion.57, 58 Quinine-induced hypoglycemia has been documented in patients with and without malaria.59, 60 Quinine-stimulated insulin release may be amplified in pregnancy, aggravating hypoglycemia.2 Monitor plasma glucose levels.
Related/similar drugs
Toxicology
Quinine and related alkaloids are rapidly absorbed from the GI tract; a single 2 to 8 g oral dose of quinine may be fatal to an adult.3, 11, 12 Treatment of an overdose is generally supportive. Urinary acidification can be employed if necessary.1 Quinine is not eliminated by hemofiltration or hemodialysis.15
References
Disclaimer
This information relates to an herbal, vitamin, mineral or other dietary supplement. This product has not been reviewed by the FDA to determine whether it is safe or effective and is not subject to the quality standards and safety information collection standards that are applicable to most prescription drugs. This information should not be used to decide whether or not to take this product. This information does not endorse this product as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this product. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this product. This information is not specific medical advice and does not replace information you receive from your health care provider. You should talk with your health care provider for complete information about the risks and benefits of using this product.
This product may adversely interact with certain health and medical conditions, other prescription and over-the-counter drugs, foods, or other dietary supplements. This product may be unsafe when used before surgery or other medical procedures. It is important to fully inform your doctor about the herbal, vitamins, mineral or any other supplements you are taking before any kind of surgery or medical procedure. With the exception of certain products that are generally recognized as safe in normal quantities, including use of folic acid and prenatal vitamins during pregnancy, this product has not been sufficiently studied to determine whether it is safe to use during pregnancy or nursing or by persons younger than 2 years of age.
More about quinine
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (20)
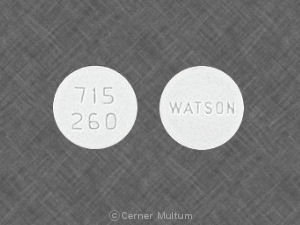
- Drug images
- Side effects
- Dosage information
- During pregnancy
- Drug class: antimalarial quinolines
- Breastfeeding
- En español
Patient resources
Professional resources
Other brands
Related treatment guides
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.