Chlorambucil
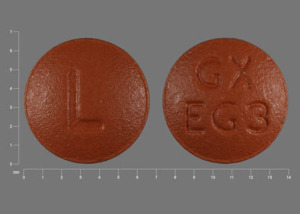
Generic name: Chlorambucil
Brand name: Leukeran
Dosage form: tablet
Drug class: Alkylating agents
What is chlorambucil?
Chlorambucil is an anti-cancer chemotherapy drug used for treatment of Hodgkin's disease and specific types of leukemias and lymphomas. It is from a group of medicines called alkylating agents which acts on cancer cells to slow down or stop their growth. It is a tablet that you swallow with a glass of water.
What is chlorambucil used for?
Chlorambucil is used in the treatment of
- Hodgkin’s disease
- chronic lymphatic (lymphocytic) leukemia,
- malignant lymphomas including lymphosarcoma,
- giant follicular lymphoma.
It does not cure these conditions but may help with symptoms that you may have.
This medicine may also be used for conditions not listed here. Talk to your doctor or healthcare provider if you have any questions about chlorambucil being used for any other conditions.
Warnings
Chlorambucil may:
- Decrease blood cells in bone marrow, so it is important you have tests done regularly to check if your blood cells are being affected by this medicine.
- Increase your risk of bleeding or infection, you should call your doctor if you have unusual bruising or bleeding, or new signs of infection (fever, chills, weakness).
- Increase the chance of developing other cancers.
- Affect your fertility, which is your ability to become pregnant or be able to father a child. Women should not become pregnant while taking chlorambucil and for a time afterwards as it may harm your fetus or cause birth defects. See below on this page for more information about chlorambucil and pregnancy.
- You should not breastfeed while using this medicine. See the breastfeeding section below for more information on chlorambucil and breastfeeding.
What should I tell my doctor before taking chlorambucil?
You should not take chlorambucil if:
- You are allergic to chlorambucil or any of the inactive ingredients in the product. See below for product ingredients.
- You have used chlorambucil in the past and it was not effective.
You should tell your doctor if you have had an allergic reaction to another cancer drug such as bendamustine, busulfan, carmustine, dacarbazine, ifosfamide, lomustine, mechlorethamine, melphalan, streptozocin, or temozolomide. If you have had an allergic reaction to one of these drugs, it may increase your risk of having an allergic reaction to chlorambucil.
Tell your doctor if you have ever had:
- kidney disease,
- liver disease,
- a seizure,
- a head injury or brain tumor,
- if you have received radiation or chemotherapy within the past 4 weeks.
How should I take chlorambucil?
Chlorambucil is a tablet that is usually taken daily for 3 to 6 weeks according to your doctor's treatment plan. Sometimes alternate treatment schedules are used which can be intermittent, biweekly or once a month pulse treatments.
While on this medicine you must be under the care of a doctor. You should follow the directions of your doctor and take the medicine exactly as prescribed.
Remember to store your tablets in the refrigerator.
Dosing Information
Your dose of chlorambucil will be worked out according to your condition that you are being treated for, your body weight, whether it is initiation of treatment or a short course.
The dosage may change or be delayed depending on how well you respond to treatment and any change in blood test results.
What happens if I miss a dose? Take the medicine as soon as you can, but if it is almost the same time for your next dose, then skip the missed dose. You should not take two doses at one time.
What happens if I overdose? If you think you have taken too much of this medicine you should get emergency medical attention or call the Poison Help line at 1-800-222-1222.
Overdose symptoms may include agitation, fast heartbeats, skin rash, bruising, bleeding gums, nosebleeds, trouble breathing, or signs of infection (fever, chills, weakness).
What should I avoid while taking chlorambucil?
Infection risk: Avoid being near people who are sick or have infections, as you may have an increased risk of infection. Tell your doctor at once if you develop signs of infection (high temperature, chills, weakness).
Bleeding or bruising risk: Avoid activities or sports that may increase your risk of bleeding or injury. When shaving or cleaning your teeth be extra careful so that you do not cause any bleeding.
Vaccines: You should not receive a "live" vaccine while using chlorambucil. Live vaccines include measles, mumps, rubella (MMR), rotavirus, typhoid, yellow fever, varicella (chickenpox), zoster (shingles), and nasal flu (influenza) vaccine.
What are the side effects of chlormabucil?
What are the serious (bad) side effects of chlorambucil?
Allergic Reactions:
You should immediately get emergency medical help if you have signs of:
- allergic reaction (difficulty breathing, swelling in your face or throat, hives)
- or a severe skin reaction (fever, sore throat, burning eyes, skin pain, red or purple skin rash with blistering and peeling).
Other serious (bad) side effects:
You should call your doctor at once if you have:
- a seizure
- any unusual lump or mass,
- severe diarrhea or vomiting,
- a cough that is new or worsening,
- signs of bone marrow suppression eg. dizziness, feeling tired or short of breath, pale lips or fingernail beds, fast heart rate,
- signs of liver problems eg. low appetite, pain in the upper right side of stomach, dark urine, clay-colored stools, yellowing of the skin or eyes, or
- signs of low blood cell counts eg. high body temperature, chills, tiredness, mouth sores, skin sores, easy bruising, unusual bleeding, pale skin, cold hands and feet, feeling light-headed or short of breath.
What are the common side effects of chlorambucil?
- nausea, vomiting or diarrhea,
- white patches or sores in or around your mouth,
- bone marrow suppression,
- low blood cell counts,
- missed menstrual periods in women.
This is not a complete list of side effects and others may occur. Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.
Related/similar drugs
Interactions
Other drugs may affect chlorambucil, including prescription and over-the-counter medicines, vitamins, and herbal products. Tell your doctor about all your current medicines and any medicine you start or stop using.
To check for interactions with chlorambucil, click the link below.
Pregnancy and breastfeeding
Fertility: Chlorambucil can affect your fertility (your ability to become pregnant or father a child) while taking treatment and afterwards. You should discuss this with your healthcare provider if you are planning on starting a family in the future. Men might be able to store sperm before starting treatment and women might be able to store eggs.
You still may be able to become pregnant, so it is important to use effective birth control while you are using this medicine and for a time afterwards.
Pregnancy: Do not use chlorambucil if you are pregnant or planning a pregnancy. It could harm the unborn baby or cause birth defects. Use effective birth control to prevent pregnancy while taking this medicine. If you are planning a pregnancy you should discuss with your doctor how long after treatment you need to wait before trying to conceive.
Breastfeeding: It is not known if chlorambucil passes into breast milk.
Many drugs do pass into breast milk and because there is potential for serious adverse reactions to your child if you breastfeed, it is important that you talk to your doctor and make a decision whether you:
- do not breastfeed and take chlorambucil,
- or discontinue chlorambucil and breastfeed.
Storage
How do I store chlorambucil?
- Store in a refrigerator at 2° to 8°C (36° to 46°F).
Ingredients
Active ingredient: chlorambucil
Inactive ingredients:
Leukeran. Tablet core: microcrystalline cellulose, anhydrous lactose, colloidal anhydrous silica, stearic acid. Tablet film coating: hypromellose, titanium dioxide, synthetic yellow, iron oxide, synthetic red iron oxide, macrogol.
Manufactured For: Aspen Global Incorporated, GBS Plaza, Cnr La Salette & Royal Roads Grand Bay, Mauritius.
References
More about chlorambucil
- Check interactions
- Compare alternatives
- Reviews (3)
- Side effects
- Dosage information
- During pregnancy
- Drug class: alkylating agents
- Breastfeeding
- En español
Patient resources
Other brands
Professional resources
Other brands
Related treatment guides
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.