Colectomy
Medically reviewed by Drugs.com. Last updated on Aug 4, 2025.
What do I need to know about a colectomy?
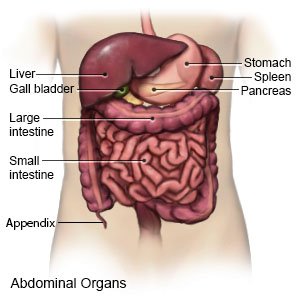
A colectomy is surgery to remove part or all of your colon.
 |
How do I prepare for surgery?
- Your surgeon will tell you how to prepare. He or she will tell you what to eat and drink in the days before surgery. He or she may tell you not to eat or drink anything after midnight on the day of surgery. Arrange to have someone drive you home after surgery.
- Tell your surgeon about all medicines you currently take. He or she will tell you if you need to stop any medicine for surgery, and when to stop. He or she will tell you which medicines to take or not take on the day of surgery.
- You may need blood tests before your surgery. You may also need an ultrasound or CT scan.
- You may need a laxative solution or an enema to clean out your colon before surgery.
Related medications
What will happen during surgery?
- You may have several small incisions or one long incision in your abdomen. Part or all of your colon will be removed. Your surgeon may attach the remaining parts of your colon with stitches. If your entire colon and rectum are removed, your small intestine will be attached to your anus.
- Your surgeon may attach your colon or small intestine to an opening in your abdomen called a stoma. This allows bowel movement to leave your body through the opening.
- Your incision will be closed with stitches or staples and covered with a bandage.
After your surgery:
You will be taken to a room to rest until you are fully awake. You will be monitored closely for any problems. You will then be able to go home or be taken to your hospital room.
- You will be helped to walk around after surgery. Movement will help prevent blood clots. You may also be given exercises to do in bed. Do not get out of bed on your own until your healthcare provider says it is okay. Talk to healthcare providers before you get up the first time. They may need to help you stand up safely.
- You will be able to eat and drink gradually. You may be given liquid nutrition through an IV at first. Then you may start to drink clear liquids. When your intestines heal from surgery, you will slowly starting eating solid food.
- Medicines may be given to prevent or treat pain. You may need bowel movement softeners to make it easier for you to have a bowel movement. You may need this medicine to prevent constipation. Blood thinners may be given to help prevent blood clots. These may make you bleed or bruise more easily.
What are the risks of surgery?
You may bleed more than expected or develop an infection. Nearby organs, such as the small intestine or bladder, may be damaged. An abscess (pocket of pus) may form near your incision. Your colon may leak and cause an infection in and around your intestines. You may develop a serious infection in your blood. An adhesion (buildup of tissue) may block your colon. You may need another colectomy. You may develop a life-threatening blood clot.
Care Agreement
You have the right to help plan your care. Learn about your health condition and how it may be treated. Discuss treatment options with your healthcare providers to decide what care you want to receive. You always have the right to refuse treatment. The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
