Colonoscopy
Medically reviewed by Drugs.com. Last updated on May 4, 2025.
What do I need to know about a colonoscopy?
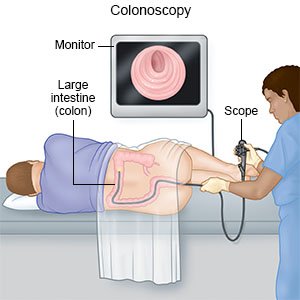
A colonoscopy is a procedure to examine the inside of your colon (intestine) with a scope. A scope is a flexible tube with a small light and camera on the end. Polyps or tissue growths may be removed during your colonoscopy.
 |
What do I need to do the week before my colonoscopy?
Give your healthcare provider a list of all the medicines, supplements, and herbs you take. You will need to stop taking medicines that contain aspirin or iron for 7 days before your colonoscopy. If you take a blood thinner, such as warfarin, ask when you should stop taking it. Make plans for someone to drive you home after your procedure.
How do I prepare for my colonoscopy?
Your healthcare provider will have you prepare your bowels before your procedure. It is important for your bowels to be empty before your procedure to allow him or her to see your colon clearly. You will need to do the following:
- Have only clear liquids for the entire day before your colonoscopy. Clear liquids include plain gelatin, unsweetened fruit juices, clear soup, and broth. Do not drink any liquid that is blue, red, or purple.
- Follow your bowel prep as directed. There are many different preparations that can be given before a colonoscopy. With any bowel prep, stay close to the bathroom. This prep will cause your bowels to move often.
- Use an enema if directed. Your healthcare provider may tell you to use an enema to help clean out your bowels.
- Do not eat or drink anything after midnight. This will help prevent problems that can happen if you vomit while under anesthesia.
Drugs used to treat this and similar conditions
Trulance
Trulance (plecanatide) is used to treat chronic idiopathic constipation (CIC) and irritable bowel ...
Anusol-HC Suppositories
Anusol-HC Suppositories is used for anal itching, hemorrhoids, proctitis, pruritus
Ozempic
Learn about Ozempic (semaglutide) for type 2 diabetes treatment, weight management, cardiovascular ...
MiraLAX
MiraLAX (polyethylene glycol) is used as a laxative to treat occasional constipation or irregular ...
Lialda
Lialda (mesalamine) is used to treat ulcerative colitis, proctitis and proctosigmoiditis. Includes ...
Humira
Humira is a tumor necrosis factor blocker that is used to treat many inflammatory conditions such ...
Budesonide
Budesonide systemic is used for asthma, asthma, maintenance, autoimmune hepatitis, crohn's disease ...
Prednisone
Prednisone is used to treat allergic disorders, ulcerative colitis, psoriasis and arthritis. Learn ...
Vasopressin
Vasopressin systemic is used for abdominal distension prior to abdominal x-ray, abdominal ...
Gabapentin
Gabapentin is an anti-epileptic drug, also called an anticonvulsant. It is used to treat some types ...
What will happen during my colonoscopy?
- You will be given medicine to help you relax. You will lie on your left side and raise one or both knees toward your chest. Your healthcare provider will examine your anus and use a gloved finger to check your rectum. You may need another enema if your bowel is not empty. The scope will be lubricated and gently placed into your anus. It will then be passed through your rectum and into your colon. Water or air will be put into your colon to help clean or expand it. This is done so your healthcare provider can see your colon clearly.
- Tissue samples may be taken from the walls of your bowel and sent to a lab for tests. If you have a polyp, your healthcare provider will pass a wire loop through the scope and use it to hold the polyp. The polyp is then removed from the wall of your colon. You should not feel this. The polyps are sent to a lab for tests. Pictures of your colon may be taken during the procedure.
What will happen after my colonoscopy?
You may feel bloated or have some gas and abdominal discomfort. You may need to lie on your left side with a heating pad on your abdomen. Eat small meals until your bloating has improved.
What are the risks of a colonoscopy?
You may have pain or bleeding. You may also have a slow heartbeat, decreased blood pressure, or increased sweating. Your colon may tear due to the increased pressure from the scope and other instruments. This may cause bowel contents to leak out of your colon and into your abdomen. If this happens, you may need to stay in the hospital and have surgery on your colon.
Care Agreement
You have the right to help plan your care. Learn about your health condition and how it may be treated. Discuss treatment options with your healthcare providers to decide what care you want to receive. You always have the right to refuse treatment. The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
Learn more about Colonoscopy
Treatment options
Symptoms and treatments
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
