Metronidazole
Pronunciation: me-troe-NI-da-zole
Generic name: metronidazole
Brand names: Flagyl, Flagyl ER, Flagyl I.V., RTU, Likmez,
... show all 8 brands
Dosage forms: intravenous solution, oral capsule, oral tablet, extended-release tablet, oral suspension ,
... show all 2 dosage forms
Drug classes: Amebicides, Miscellaneous antibiotics
What is metronidazole?
Metronidazole is an antibiotic that may be used to treat certain infections of the vagina, stomach, liver, skin, joints, brain and spinal cord, lungs, heart, or bloodstream.
Metronidazole has been approved to treat:
- Symptomatic trichomoniasis (a sexually transmitted infection) in adults that has been confirmed by culture or wet smear test
- Asymptomatic trichomoniasis in females when associated with cervical changes, and in asymptomatic sexual partners
- Amebiasis (an infection caused by a parasite) in adults and children
- Anaerobic bacterial infections (infections caused by bacteria that do not need oxygen to survive).
Metronidazole is thought to work by first diffusing into the cytoplasm of the anaerobic bacteria where it is then activated and reduced into a short-lived nitroso free radical which can interact with DNA, causing a loss of the helical DNA structure, strand breakage, and bacterial death.
Metronidazole is well absorbed after oral administration, with peak concentrations being reached in one to two hours. Although it starts to work quickly, it may take a couple of days before you start to feel better or notice an improvement in your symptoms. It is important that you still finish the course of metronidazole that your doctor has prescribed, even if you feel better, because the infection may still be present, and it could flare up or recur if you haven’t finished the course.
Metronidazole was first FDA-approved in 1963.
Warnings
To reduce the development of drug-resistant bacteria, do not use metronidazole to treat any condition that has not been checked by your doctor. This medicine will not treat a viral infection such as the common cold or flu.
Metronidazole has been shown to be carcinogenic in rats and mice and unnecessary use should be avoided.
Do not use metronidazole if you recently drank alcohol, or have taken disulfiram (Antabuse) within the past 2 weeks. Do not drink alcohol or consume foods or medicines that contain propylene glycol while you are taking metronidazole and for at least 3 days after you stop taking it.
Seizures and other nervous system abnormalities have been reported in patients treated with metronidazole. You should stop using this medicine immediately if you experience any neurological symptoms such as seizures, headaches, visual changes, weakness, numbness, or tingling.
Related/similar drugs
prednisone, amoxicillin, omeprazole, pantoprazole, doxycycline, ciprofloxacin, cephalexin
Before taking this medicine
You should not use this medicine if you are allergic to metronidazole, secnidazole, or tinidazole, or if you:
- drank alcohol in the past 3 days
- consumed foods or medicines that contain propylene glycol in the past 3 days or
- took disulfiram (Antabuse) within the past 14 days
- have Cockayne Syndrome (a rare genetic disorder that affects growth and development).
Before taking metronidazole, tell your healthcare provider about all of your medical conditions, including if you:
- liver disease
- kidney disease (or if you are on dialysis)
- a heart rhythm disorder
- a stomach or intestinal disease such as Crohn's disease
- a blood cell disorder such as anemia (lack of red blood cells) or low white blood cell (WBC) counts
- medical problems that affect the brain or a nerve disorder
- a yeast infection or a fungal infection anywhere in your body
- a history of blood problems
- or take any medications, especially warfarin, lithium, busulfan, cimetidine, phenytoin, or phenobarbital.
Tell your doctor if you are pregnant or intend to become pregnant. The use of metronidazole during pregnancy has been well-studied and a review of 17 studies found that treating bacterial vaginosis and trichomoniasis with metronidazole reduced the risk of preterm birth and was effective and offered no teratogen risk. Conversely, isolated studies have suggested its use may result in low birth weight or preterm delivery. Talk to your doctor about the risks and benefits of taking metronidazole during pregnancy. Some product labels for metronidazole say it is contraindicated during the first trimester.
Tell your doctor if you are breastfeeding or plan to breastfeed. Metronidazole can pass into your breast milk. Talk to your healthcare provider about the best way to feed your baby while taking metronidazole. If you are breastfeeding, you may consider pumping and throwing away your breast milk during treatment with metronidazole and for 48 hours after your last dose and feeding your infant stored human milk or formula.
Not all uses of metronidazole are approved for treating children and teenagers. Metronidazole is not approved to treat vaginal infections in girls who have not begun having menstrual periods.
How should I take metronidazole?
Take metronidazole exactly as prescribed by your doctor. Follow all directions on your prescription label and read all medication guides or instruction sheets.
- The dose depends on the infection being treated.
- The dosage should be reduced by 50% in those with severe hepatic impairment.
- In patients undergoing hemodialysis, consider a supplementary dose following the hemodialysis session, depending on the patient's clinical situation.
- Metronidazole will not treat a vaginal yeast infection. You may even develop a new vaginal yeast infection, which may need to be treated with antifungal medication. Tell your doctor if you have symptoms such as itching or discharge during or after treatment with this medicine.
- If you are treating a vaginal anaerobic bacterial infection, your sexual partner may also need to take metronidazole so you don't become reinfected.
- Do not share this medicine with another person, even if they have the same symptoms you have.
- Metronidazole is usually given for up to 10 days in a row. You may need to repeat this dosage several weeks later.
- Keep using this medicine even if your symptoms quickly improve. Skipping doses could make your infection resistant to medication. This medicine will not treat a viral infection (flu or a common cold).
Oral metronidazole
- Oral metronidazole tablets, capsules, and the suspension are taken by mouth. May be taken with or without food.
- Shake the oral suspension well before each use. Always use an accurate measuring device to measure the correct amount. Do not use a household teaspoon or tablespoon to measure your medicine. You can ask your pharmacist for the measuring device you should use and how to measure the correct dose.
- Swallow the extended-release tablet whole and do not crush, chew, or break it.
Metronidazole injection
- The injection is given as an infusion into a vein. A healthcare provider will give you the injection if you are unable to take the medicine by mouth.
Dosing information
Trichomoniasis (adults)
Treatment should be individualized. Usual dosages are:
- One-day treatment: 2 grams as a single oral dose or a split dose given on the same day
- 7-day course: 250mg three times daily for 7 consecutive days.
Amebiasis
- Adults: acute amebic dysentery. 750mg three times daily for 5 to 10 days.
- Adults: amebic liver abscess. 500mg or 750mg three times daily for 5 to 10 days.
- Children: 35mg/kg/24 hours to 50mg/kg/24 hours divided into three doses daily for 10 days.
Do not exceed adult dosages.
Anaerobic Bacterial Infections (adults)
For more serious anaerobic infections, intravenous metronidazole is usually administered initially.
- Adults: 7.5 mg/kg every 6 hours (this works out at approximately 500mg for a 70kg adult) orally for 7 to 10 days. Maximum dose 4g/24 hours.
A longer course of treatment may be required for bone, joint, lower respiratory tract, and endocardium infections.
What should I avoid while using metronidazole?
Do not drink alcohol or consume foods, medicines, or other products that contain alcohol or propylene glycol while taking metronidazole and for 3 days after your last dose. You may have unpleasant effects such as headaches, nausea, vomiting, stomach cramps, and warmth or tingling under your skin.
What are the side effects of metronidazole?
Get emergency medical help if you have signs of an allergic reaction to metronidazole (hives, itching, warmth, or tingling; fever, joint pain; dry mouth, dry vagina; stuffy nose, difficulty breathing, swelling in your face or throat) or a severe skin reaction (fever, sore throat, burning eyes, skin pain, red or purple skin rash with blistering and peeling).
Metronidazole may cause serious side effects including:
- Nervous system problems, including brain disorder (encephalopathy), inflammation of the brain and spinal cord membranes (aseptic meningitis), numbness or tingling in the hands or feet (peripheral neuropathy), and seizures (convulsions). Tell your healthcare provider right away if you have any nervous system problems while taking metronidazole
- Worsening yeast infection (candidiasis) symptoms in people with a known yeast infection or a yeast infection they were not aware of
- Low white blood cell count (leukopenia) in people with a history of blood problems. This can affect how well the body fights infection.
The most common side effects of metronidazole include
- Diarrhea
- Nausea
- Headache
- Pain in the upper abdomen and abdominal cramping
- Vomiting
- Weight loss
- Constipation.
Other side effects of metronidazole may include allergic reactions: such as itching, hives (urticaria), flushing of the skin, red skin rash that can be widespread, blisters and separation of skin layers, nasal congestion, dryness of the mouth and vagina, and fever.
Abnormal heart rhythms (QT prolongation) may also occur. Metronidazole can cause life-threatening liver problems in people with Cockayne syndrome. If you have this condition, stop taking this medicine and contact your doctor if you have signs of liver failure--nausea, stomach pain (upper right side), dark urine, clay-colored stools, or jaundice (yellowing of the skin or eyes).
These are not all the possible side effects of metronidazole. Call your doctor for medical advice about side effects. You may report side effects to the FDA at 1-800-FDA-1088.
What happens if I miss a dose?
Take the medicine as soon as you can but skip the missed dose if it is almost time for your next dose. Do not take two doses at one time.
What happens if I overdose?
Seek emergency medical attention or call the Poison Help line at 1-800-222-1222.
Overdose symptoms may include nausea, vomiting, numbness, tingling, or problems with balance or muscle movement.
What other drugs will affect metronidazole?
Sometimes it is not safe to use certain medicines at the same time. Some drugs can affect your blood levels of other drugs you use, which may increase side effects or make the medicines less effective.
Tell your doctor about all your current medicines. Many drugs can affect metronidazole, especially:
- antidepressants, such as escitalopram
- albuterol, an asthma medication
- busulfan or other cancer medications
- some heart or blood pressure medications
- lithium or other antipsychotics
- medicines to treat malaria, HIV, or other infections
- blood thinners such as warfarin.
Drinking alcohol while taking metronidazole is not recommended because the combination can cause a reaction (often referred to as a disulfiram-like reaction) in some people. Symptoms may include flushing, headaches, nausea, vomiting, and stomach cramps. The product information and health professionals recommend not drinking alcohol or taking products that contain propylene glycol during metronidazole treatment and for 3 days after finishing the course.
This list is not complete and many other drugs may interact with metronidazole. This includes prescription and over-the-counter medicines, vitamins, and herbal products. Not all possible drug interactions are listed here.
This medicine can affect the results of certain medical tests. Tell any doctor who treats you that you are using this medicine.
Storage
Store at room temperature between 68°F to 77°F (20°C to 25°C) away from moisture and heat. Do not freeze.
Throw away (discard) any unused suspension 10 days after opening the container. Keep out of reach of children.
Popular FAQ
Drinking alcohol while taking metronidazole is not recommended because the combination of metronidazole and alcohol can cause a reaction (often referred to as a disulfiram-like reaction) in some people. Symptoms may include flushing, headaches, nausea, vomiting, and stomach cramps. There has been one reported death associated with this reaction. The product information and health professionals recommend not to drink alcohol during metronidazole treatment and for 3 days after finishing the course. Continue reading
Metronidazole starts to work 1 to 2 hours after you take it, because it is quickly absorbed, and it reaches its maximum concentration after 20 minutes to 3 hours. But it may take a couple of days before you start to feel better or notice an improvement in your symptoms. It is important that you still finish the course of metronidazole that your doctor has prescribed, even if you feel better, because the infection may still be present, and it could flare up or recur if you haven’t finished the course. Continue reading
About 10% of women report a vaginal yeast infection (vaginal candidiasis) as a side effect of metronidazole treatment. Although metronidazole spares vaginal lactobacilli, which are naturally resistant to nitroimidazoles such as metronidazole, it does not restore a Lactobacillus-dominated microbiome and disruption in the normal vaginal microbiota can persist. Continue reading
Metronidazole (brand: Flagyl) can leave a bitter, metallic taste in your mouth. This is a well-known side effect. For many, the bad taste lasts throughout treatment, too, not just when you're swallowing the medicine. There are ways to help mask this taste with certain foods. Continue reading
Metronidazole does not treat chlamydia and is not a recommended treatment for chlamydia, but it may be given if symptoms of chlamydia persist after finishing a course of first-line treatments for chlamydia such as doxycycline, azithromycin, or levofloxacin. When metronidazole is given as follow up treatment for persistent symptoms of chlamydia, usually in addition to other antibiotics such erythromycin, it is there to provide treatment for other possible bacterial causes that may cause similar symptoms to chlamydia.
Infections linked with sexual activity that are usually treated with metronidazole include bacterial vaginosis, trichomoniasis, and moderate-to-severe pelvic inflammatory disease. Continue reading
Flagyl is well-known for causing diarrhea, as well as other stomach side effects like nausea, heartburn and stomach pain. Diarrhea is common and occurs in about 1% to 10% of patients. Flagyl may also cause an unpleasant metallic taste during therapy which can lead to nausea and a decreased appetite. Continue reading
If you are taking oral metronidazole or using metronidazole gel for an infection that is linked with sexual activity, such as trichomoniasis, pelvic inflammatory disease, or bacterial vaginosis you should not have sex for 7 days after single-dose therapy (or until you have completed the 7-day treatment regimen) and your symptoms have resolved. This will help reduce the risk of reinfection. If your sexual partners are also being treated, then abstain from sexual intercourse until they have finished treatment. Continue reading
More FAQ
- What are the most common skin conditions? (with photos)
- How long does it take metronidazole to leave your system?
References
More about metronidazole
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (2,421)
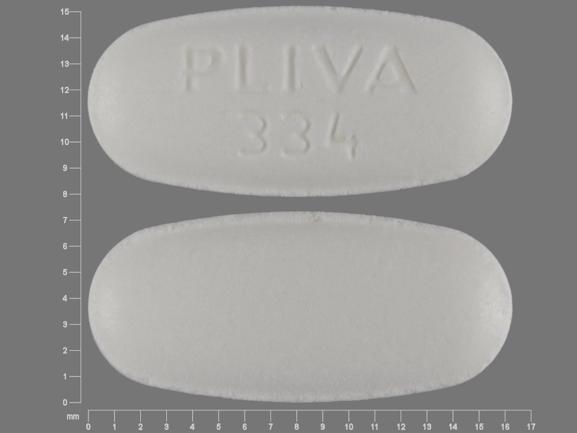
- Drug images
- Side effects
- Dosage information
- Patient tips
- During pregnancy
- Support group
- Drug class: amebicides
- Breastfeeding
Patient resources
- Metronidazole (Intravenous) advanced reading
- Metronidazole Tablets and Capsules
- Metronidazole Injection
Other brands
Flagyl, Likmez, Flagyl IV, Flagyl ER
Professional resources
- Metronidazole monograph
- Metronidazole (FDA)
- Metronidazole Capsules (FDA)
- Metronidazole Extended Release (FDA)
- Metronidazole Injection (FDA)
Other brands
Flagyl, Likmez, Flagyl ER, Flagyl 375
Related treatment guides
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.