Tipranavir (Monograph)
Brand name: Aptivus
Drug class: HIV Protease Inhibitors
VA class: AM800
Chemical name: 2-Pyridinesulfonamide, –(3-[[1R]-1-[[6R]-5,6-dihydro-4-hydroxy-2-oxo-6-[2-phenylethyl]-6-propyl-2H-pyran-3-yl]propyl]phenyl)-5-(trifluoromethyl)-
Molecular formula: C31H33F3N2O5S
CAS number: 174484-41-4
Warning
-
Clinical hepatitis and hepatic decompensation, including some fatalities, reported. (See Hepatic Effects under Cautions.)
-
Extra vigilance warranted in HIV-infected patients with chronic HBV or HCV coinfection since these individuals are at increased risk of hepatotoxicity. (See Hepatic Impairment under Cautions.)
-
Intracranial hemorrhage, including some fatalities, reported. (See Intracranial Hemorrhage under Cautions.)
Introduction
Antiretroviral; HIV protease inhibitor (PI).
Uses for Tipranavir
Treatment of HIV Infection
Treatment of HIV-1 infection in adults, adolescents, and pediatric patients ≥2 years of age. Must be used in conjunction with low-dose ritonavir (ritonavir-boosted tipranavir) and other antiretrovirals.
Used in patients who are antiretroviral-experienced and infected with HIV-1 resistant to multiple HIV PIs.
Not labeled by FDA for initial treatment in antiretroviral-naive patients, and use in such patients is not recommended.
Not recommended for initial treatment in antiretroviral-naive adults and adolescents because of inferior virologic efficacy and higher rate of adverse events compared with other ritonavir-boosted PIs and because higher ritonavir dosage required for boosting plasma tipranavir concentrations compared with other PIs.
Not recommended for initial treatment in antiretroviral-naive pediatric patients because higher ritonavir dosage required for boosting plasma tipranavir concentrations compared with other ritonavir-boosted PIs and rare, but serious, adverse events reported (i.e., intracranial hemorrhage).
Consider the following factors when initiating ritonavir-boosted tipranavir: Use with other active antiretrovirals is associated with greater likelihood of treatment response; genotypic or phenotypic viral resistance testing and/or treatment history should guide therapy; number of baseline primary PI mutations affects virologic response to the drug; caution advised in patients at increased risk of hepatotoxicity or bleeding or in patients receiving certain drugs concomitantly. (See Cautions and see Interactions.)
Tipranavir Dosage and Administration
Administration
Oral Administration
Administer orally in conjunction with low-dose ritonavir (ritonavir-boosted tipranavir). Do not use without low-dose ritonavir.
Take tipranavir and low-dose ritonavir at same time.
If tipranavir is taken with ritonavir capsules or oral solution, take the drugs with or without meals.
If tipranavir is taken with ritonavir tablets, take the drugs with a meal.
Capsules
Swallow tipranavir capsules whole; do not chew.
Assess children for ability to swallow capsules; consider oral solution in those unable to reliably swallow capsules.
Oral Solution
Use oral solution in those who have difficulty swallowing capsules.
Oral solution is a clear yellow viscous liquid; supplied with an oral dispensing syringe.
Dosage
Pediatric Patients
Treatment of HIV Infection
Oral
Dosage is based on body weight or body surface area. To avoid medication errors, use extra care in calculating dose, transcribing medication order, dispensing prescription, and providing dosing instructions.
Children 2–18 years of age: 14 mg/kg (375 mg/m2) twice daily with ritonavir 6 mg/kg (150 mg/m2) twice daily. If this dosage is not tolerated due to adverse effects, consider reducing dosage to 12 mg/kg (290 mg/m2) twice daily with ritonavir 5 mg/kg (115 mg/m2) twice daily provided the virus is not resistant to multiple HIV PIs.
Adults
Treatment of HIV Infection
Oral
500 mg twice daily with low-dose ritonavir (200 mg twice daily).
Prescribing Limits
Pediatric Patients
Treatment of HIV Infection
Oral
Do not exceed adult dosage.
Special Populations
Hepatic Impairment
Mild hepatic impairment (Child-Pugh class A): Dosage adjustments not necessary.
Moderate or severe hepatic impairment (Child-Pugh class B or C): Contraindicated.
Renal Impairment
Renal clearance of tipranavir negligible; decreased total body clearance not expected in renal impairment. Some experts state dosage adjustment not necessary.
Geriatric Patients
Select dosage with caution because of age-related decreases in hepatic, renal, and/or cardiac function and concomitant disease and drug therapy.
Cautions for Tipranavir
Contraindications
-
Moderate or severe hepatic impairment (Child-Pugh class B or C).
-
Concomitant use with drugs highly dependent on CYP3A for metabolism and for which elevated plasma concentrations are associated with serious and/or life-threatening events (e.g., alfuzosin, certain antiarrhythmics, cisapride, ergot alkaloids, lurasidone, pimozide, sildenafil used for treatment of pulmonary arterial hypertension [PAH], oral midazolam, triazolam, lovastatin, simvastatin). (See Specific Drugs under Interactions.)
-
Concomitant use with potent CYP3A inducers (e.g., rifampin, St. John’s wort [Hypericum perforatum]) since such use may result in decreased plasma concentrations of tipranavir and possible loss of virologic response. (See Specific Drugs under Interactions.)
Warnings/Precautions
Sensitivity Reactions
Dermatologic Reactions
Mild to moderate rash, including maculopapular rash and possible photosensitivity reactions reported. Rash accompanied by joint pain or stiffness, throat tightness, or generalized pruritus also reported. Discontinue if severe rash occurs.
Rash reported in healthy, HIV-negative women who received a single dose of ethinyl estradiol followed by ritonavir-boosted tipranavir. (See Estrogens/Progestins under Interactions.)
Sulfonamide Sensitivity
Tipranavir contains a sulfonamide moiety; use with caution in patients with known sulfonamide allergy. Potential for cross-sensitivity between drugs with sulfonamide moieties and tipranavir unknown.
Hepatic Effects
Hepatitis and hepatic decompensation (including some fatalities) reported; causal relationship not established. Hepatotoxicity generally has occurred in patients with advanced HIV infection receiving multiple concomitant drugs.
Increased concentrations of serum hepatic transaminases (grade 3 and 4) reported.
Evaluate hepatic function prior to and frequently during treatment. HIV-infected patients with coexisting HBV or HCV infection or elevated serum transaminases prior to therapy may be at increased risk for hepatotoxicity, including further transaminase increases or hepatic decompensation.
Discontinue if signs or symptoms of hepatitis develop, if asymptomatic increases in serum AST or ALT of >10 times the ULN occur, or if asymptomatic increases in AST or ALT of 5–10 times the ULN and increases in total bilirubin of >2.5 times the ULN develop.
Clinicians and patients should be vigilant for appearance of signs or symptoms of hepatitis (e.g., fatigue, malaise, anorexia, nausea, jaundice, bilirubinemia, acholic stools, liver tenderness, hepatomegaly). (See Hepatic Impairment under Cautions.)
Intracranial Hemorrhage
Intracranial hemorrhage (including some fatalities) reported. Other medical conditions or concomitant therapy may have caused or contributed to these events.
Ritonavir-boosted tipranavir therapy generally not associated with abnormal coagulation parameters; abnormal coagulation parameters have not preceded intracranial hemorrhage.
Manufacturer states that routine monitoring of coagulation parameters not necessary.
Interactions
Tipranavir must be used with low-dose ritonavir (ritonavir-boosted tipranavir). Failure to administer with recommended low-dose ritonavir will result in subtherapeutic tipranavir concentrations and inadequate antiviral response. Consider the usual cautions, precautions, and contraindications associated with ritonavir.
Concomitant use with certain drugs is not recommended or requires particular caution. (See Specific Drugs under Interactions.) Consider potential for drug interactions prior to and during ritonavir-boosted tipranavir therapy. Review all drugs patient is receiving and monitor for adverse effects.
Effects on Platelets and Coagulation
Tipranavir inhibits platelet aggregation in vitro.
Caution advised in patients who may be at risk for increased bleeding from trauma, surgery, or other medical conditions; those receiving concomitant drugs known to increase the risk of bleeding (i.e., anticoagulants, antiplatelet agents); and those receiving high-dose vitamin E.
Vitamin E
Each mL of tipranavir oral solution contains 116 units of vitamin E. Vitamin E content of usual dosages of this formulation exceeds recommended daily intake.
Hyperglycemic and Diabetogenic Effects
Hyperglycemia (potentially persistent), new-onset diabetes mellitus or exacerbation of preexisting diabetes mellitus reported with use of HIV PIs; diabetic ketoacidosis has occurred.
Initiate or adjust antidiabetic therapy (e.g., insulin, oral hypoglycemic agents) as needed. (See Specific Drugs under Interactions.)
Immune Reconstitution Syndrome
During initial treatment, patients who respond to antiretroviral therapy may develop an inflammatory response to indolent or residual opportunistic infections (e.g., Mycobacterium avium complex [MAC], M. tuberculosis, cytomegalovirus [CMV], Pneumocystis jirovecii [formerly P. carinii], reactivation of herpes simplex and herpes zoster); this may necessitate further evaluation and treatment.
Autoimmune disorders (e.g., Graves' disease, polymyositis, Guillain-Barré syndrome) reported in the setting of immune reconstitution; time to onset is more variable and can occur many months after initiation of antiretroviral therapy.
Adipogenic Effects
Possible redistribution or accumulation of body fat, including central obesity, dorsocervical fat enlargement (buffalo hump), peripheral wasting, breast enlargement, and general cushingoid appearance. Mechanism and long-term consequences of fat redistribution unknown; causal relationship not established.
Lipid Effects
Increased concentrations of total serum cholesterol and triglycerides reported.
Determine serum cholesterol and triglyceride concentrations prior to and periodically during therapy; manage lipid disorders as clinically appropriate. (See HMG-CoA Reductase Inhibitors under Interactions.)
Hemophilia A and B
Spontaneous bleeding reported with HIV PIs; causal relationship not established.
Use with caution in patients with history of hemophilia A or B. Increased hemostatic therapy (e.g., antihemophilic factor) may be needed.
HIV Resistance
Potential for cross-resistance with other HIV PIs not evaluated. Effect of ritonavir-boosted tipranavir therapy on subsequent therapy with other HIV PIs unknown.
Specific Populations
Pregnancy
Category C.
Antiretroviral Pregnancy Registry at 800-258-4263 or [Web].
Some experts state data insufficient to recommend routine use of ritonavir-boosted tipranavir for initial treatment in antiretroviral-naive pregnant women.
Lactation
Not known whether distributed into milk.
Instruct HIV-infected women not to breast-feed because of risk of HIV transmission and risk of adverse effects in the infant.
Pediatric Use
Safety and efficacy not established in children <2 years of age.
Adverse effects reported in children generally similar to those reported in adults; rash reported more frequently in children than in adults.
Geriatric Use
Insufficient experience in patients ≥65 years of age to determine whether geriatric patients respond differently than younger adults.
Use with caution and monitor because of age-related decreases in hepatic, renal, and/or cardiac function and concomitant disease and drug therapy.
Hepatic Impairment
Use with caution since tipranavir concentrations may be increased.
Contraindicated in moderate or severe hepatic impairment (Child-Pugh class B or C).
Risk for further elevations in hepatic enzyme concentrations or severe liver disease in HIV-infected patients with chronic HBV or HCV coinfection or increased AST or ALT concentrations prior to therapy. (See Hepatic Effects under Cautions.)
Common Adverse Effects
Diarrhea, nausea, pyrexia, fatigue, vomiting, headache, abdominal pain.
Drug Interactions
Drug interaction studies were conducted using ritonavir-boosted tipranavir.
Tipranavir metabolized principally by CYP3A4.
Tipranavir with low-dose ritonavir inhibits CYP3A and 2D6.
Tipranavir is a P-glycoprotein (P-gp) substrate and is both a weak inhibitor and potent inducer of P-gp transport system.
Drugs Affecting or Metabolized by Hepatic Microsomal Enzymes
Pharmacokinetic interactions likely with drugs that are inhibitors, inducers, or substrates of CYP3A4 with possible alteration in metabolism of tipranavir, ritonavir, and/or other drug.
Drugs Affecting or Affected by P-glycoprotein Transport
Pharmacokinetic interactions likely with drugs that are P-gp inhibitors or inducers with possible altered metabolism of tipranavir or the other drug.
Specific Drugs
|
Drug |
Interaction |
Comments |
|---|---|---|
|
Abacavir |
Decreased abacavir AUC; clinical importance unknown In vitro evidence of additive antiretroviral effects |
Appropriate dosages for concomitant use with respect to safety and efficacy not established |
|
Alfuzosin |
Increased alfuzosin concentrations expected and risk of hypotension |
Concomitant use contraindicated |
|
Antacids |
Decreased tipranavir concentrations and AUC |
Administer ritonavir-boosted tipranavir 2 hours before or 1 hour after antacids |
|
Antiarrhythmic agents (amiodarone, disopyramide, dofetilide, dronedarone, flecainide, lidocaine, mexiletine, propafenone, quinidine) |
Amiodarone, disopyramide, dofetilide, flecainide, lidocaine, mexiletine, propafenone, quinidine: Possible increased concentrations of antiarrhythmic agents Dronedarone: Increased dronedarone concentrations expected |
Amiodarone, flecainide, propafenone, quinidine: Concomitant use contraindicated Disopyramide, dofetilide, lidocaine, mexiletine: Experts state do not use concomitantly; consider alternative antiarrhythmic agent or antiretroviral Dronedarone: Experts state concomitant use contraindicated |
|
Anticoagulants, oral |
Potential for increased risk of bleeding Apixaban, rivaroxaban: Increased concentrations of the anticoagulant expected Betrixaban, dabigatran, edoxaban: Possible increased concentrations of the anticoagulant Warfarin: Possible altered warfarin concentrations; potential for serious and/or life-threatening bleeding |
Apixaban: Experts state concomitant use not recommended, consider alternative antiretroviral or warfarin; if concomitant use necessary, reduce apixaban dosage by 50% and monitor for apixaban toxicity Betrixaban, edoxaban, rivaroxaban: Experts state concomitant use not recommended; consider alternative antiretroviral or warfarin Dabigatran: Experts state consider alternative antiretroviral or warfarin; if concomitant use necessary, administer dabigatran and ritonavir-boosted tipranavir at the same time Warfarin: Use with caution; monitor INR, especially when initiating or discontinuing ritonavir-boosted tipranavir; adjust warfarin dosage as needed |
|
Anticonvulsants (carbamazepine, eslicarbazepine, ethosuximide, lamotrigine, oxcarbazepine, phenobarbital, phenytoin, valproic acid) |
Carbamazepine: Possible increased carbamazepine concentrations; possible decreased tipranavir concentrations Eslicarbazepine, oxcarbazepine: Possible decreased tipranavir concentrations Ethosuximide: Possible increased ethosuximide concentrations Lamotrigine: Possible decreased lamotrigine concentrations Phenobarbital, phenytoin: Possible decreased tipranavir concentrations; possible decreased phenytoin concentrations Valproic acid: Possible decreased valproic acid concentrations |
Carbamazepine, phenobarbital, phenytoin: Use with caution; consider alternative anticonvulsant; if used concomitantly, monitor anticonvulsant and tipranavir concentrations and virologic response Eslicarbazepine, oxcarbazepine: Experts state consider alterative anticonvulsant or antiretroviral; if concomitant use necessary, monitor virologic response and consider anticonvulsant and tipranavir concentration monitoring Ethosuximide: Monitor clinically for ethosuximide toxicities Lamotrigine: Experts state increased lamotrigine dosage may be needed; consider lamotrigine concentration monitoring or consider alternative anticonvulsant Valproic acid: Use concomitantly with caution; monitor valproate concentrations and virologic response |
|
Antifungals, azoles |
Fluconazole: Increased tipranavir concentrations and AUC; no clinically important effect on fluconazole concentrations Isavuconazonium (prodrug of isavuconazole): Possible increased isavuconazole concentrations and altered tipranavir concentrations Itraconazole, ketoconazole: Increased antifungal concentrations Posaconazole: Possible increased posaconazole and tipranavir concentrations Voriconazole: Altered voriconazole concentration |
Fluconazole: Fluconazole dosage adjustment not needed, but fluconazole dosage >200 mg daily not recommended; if high fluconazole dosage indicated, consider an alternative HIV PI or antiretroviral agent from another class Isavuconazonium: Monitor for tipranavir- and isavuconazole-associated adverse effects and virologic efficacy; consider monitoring isavuconazole concentrations Itraconazole: Use concomitantly with caution; itraconazole dosage >200 mg daily not recommended unless dosage guided by itraconazole concentration monitoring Ketoconazole: Use concomitantly with caution; ketoconazole dosage >200 mg daily not recommended Posaconazole: Monitor for tipranavir-associated adverse effects; consider monitoring for posaconazole-associated adverse effects and consider posaconazole concentration monitoring Voriconazole: Do not use concomitantly unless potential benefits outweigh risks; if used, consider monitoring voriconazole concentrations and adjusting voriconazole dosage accordingly |
|
Antimycobacterials (bedaquiline, rifabutin, rifampin, rifapentine) |
Bedaquiline: Increased bedaquiline concentrations; clinical importance unknown Rifabutin: Increased rifabutin concentrations; no change in tipranavir concentrations Rifampin: Possible decreased tipranavir concentrations; possible decreased antiretroviral activity and increased risk of tipranavir resistance Rifapentine: Possible decreased tipranavir concentrations |
Bedaquiline: Use concomitantly with caution and monitor for QTc interval prolongation and liver dysfunction Rifabutin: Reduce rifabutin dosage to 150 mg every other day or 3 times weekly (further reduction may be needed); increase monitoring for adverse effects; monitor for antimycobacterial response and consider therapeutic drug monitoring Rifampin: Concomitant use contraindicated Rifapentine: Do not use concomitantly |
|
Antiplatelet agents |
Potential for increased risk of bleeding Ticagrelor, vorapaxar: Increased antiplatelet concentrations expected |
Use concomitantly with caution Ticagrelor, vorapaxar: Concomitant use not recommended; experts state consider alternative antiretroviral |
|
Antipsychotics (lurasidone, perphenazine, pimozide, quetiapine, risperidone, thioridazine) |
Lurasidone: Increased lurasidone concentrations expected; potential for serious and/or life-threatening adverse effects Perphenazine, risperidone, thioridazine: Possible increased concentrations of the antipsychotic Pimozide: Potential for serious and/or life-threatening adverse effects (e.g., cardiac arrhythmias) Quetiapine: Increased quetiapine concentrations expected |
Lurasidone: Concomitant use contraindicated Perphenazine, risperidone, thioridazine: Experts state initiate antipsychotic using lowest dosage, adjust maintenance dosage as needed, and monitor for antipsychotic-associated adverse effects Pimozide: Concomitant use contraindicated Quetiapine: Consider alternative antiretroviral to avoid increased quetiapine exposures; if concomitant use necessary, initiate quetiapine at lowest dosage and titrate as needed; if initiating ritonavir-boosted tipranavir in patient receiving quetiapine, reduce quetiapine to one-sixth of original dosage; monitor for quetiapine efficacy and adverse effects |
|
Atazanavir |
Ritonavir-boosted tipranavir: Decreased atazanavir concentrations and AUC and increased tipranavir concentrations and AUC In vitro evidence of additive to antagonistic antiretroviral effects |
Atazanavir (with or without low-dose ritonavir): Concomitant use not recommended |
|
Avanafil |
Possible increased avanafil concentrations and increased risk of avanafil-associated adverse effects (e.g., hypotension, syncope, visual disturbances, prolonged erection) |
Experts state concomitant use not recommended |
|
Benzodiazepines |
Midazolam, triazolam: Possible increased concentrations of midazolam or triazolam; potential for serious and/or life-threatening effects (e.g., prolonged or increased sedation or respiratory depression) Alprazolam, clonazepam, diazepam: Possible increased benzodiazepine concentrations |
Midazolam, triazolam: Concomitant use with oral midazolam or triazolam contraindicated; some experts state a single parenteral dose of midazolam can be used with caution in a monitored situation for procedural sedation Alprazolam, clonazepam, diazepam: Consider alternative benzodiazepines with less potential for interaction (e.g., lorazepam, oxazepam, temazepam) |
|
β-Adrenergic blocking agents (atenolol, carvedilol, labetalol, metoprolol, nadolol, timolol, sotalol) |
Carvedilol, metoprolol, timolol: Possible increased concentrations of the β-blocker |
Carvedilol, metoprolol, timolol: Clinical monitoring recommended and reduced dosage of the β-blocker may be needed; experts state consider use of alternatives not metabolized by CYP enzymes (e.g., atenolol, labetalol, nadolol, sotalol) |
|
Bosentan |
Possible increased bosentan concentrations |
In patients already receiving ritonavir-boosted tipranavir for ≥10 days, initiate bosentan using dosage of 62.5 mg once daily or every other day based on individual tolerability In patients already receiving bosentan, discontinue bosentan for ≥36 hours prior to initiating ritonavir-boosted tipranavir; after ≥10 days of ritonavir-boosted tipranavir, resume bosentan using dosage of 62.5 mg once daily or every other day based on individual tolerability |
|
Buprenorphine, buprenorphine and naloxone |
Buprenorphine or fixed combination of buprenorphine and naloxone (buprenorphine/naloxone): Decreased tipranavir concentrations; no effect on clinical efficacy of buprenorphine/naloxone |
Buprenorphine or buprenorphine/naloxone: Dosage adjustments cannot be recommended; consider monitoring tipranavir concentrations If transmucosal buprenorphine is switched to buprenorphine implant, monitor to ensure buprenorphine effects are adequate and not excessive |
|
Bupropion |
Decreased bupropion AUC |
Titrate bupropion dosage based on clinical response |
|
Buspirone |
Increased buspirone concentrations expected |
Use low buspirone dosage with caution and titrate based on clinical response |
|
Calcifediol |
Possible increased calcifediol concentrations |
Experts state calcifediol dosage adjustment may be required; closely monitor serum concentrations of 25-hydroxyvitamin D, intact parathyroid hormone, and calcium |
|
Calcium-channel blocking agents (e.g., diltiazem, felodipine, nicardipine, nisoldipine, verapamil) |
Altered concentrations of calcium-channel blocking agents |
Use concomitantly with caution; clinical monitoring recommended |
|
Colchicine |
Increased colchicine concentrations |
Patients with renal or hepatic impairment: Concomitant use with ritonavir-boosted tipranavir contraindicated Patients with normal renal or hepatic function: Dosage adjustments recommended when used with ritonavir-boosted tipranavir Colchicine for treatment of gout flares: In those receiving ritonavir-boosted tipranavir, use initial colchicine dose of 0.6 mg followed by 0.3 mg 1 hour later and repeat dose no earlier than 3 days later Colchicine for prophylaxis of gout flares: In those receiving ritonavir-boosted tipranavir, decrease colchicine dosage to 0.3 mg once daily in those originally receiving 0.6 mg twice daily or decrease dosage to 0.3 mg once every other day in those originally receiving 0.6 mg once daily Colchicine for treatment of familial Mediterranean fever (FMF): In those receiving ritonavir-boosted tipranavir, use maximum colchicine dosage of 0.6 mg daily (may be given as 0.3 mg twice daily) |
|
Cisapride |
Potential for serious and/or life-threatening effects such as cardiac arrhythmias |
Concomitant use contraindicated |
|
Clarithromycin |
Slightly increased clarithromycin concentrations; decreased hydroxyclarithromycin concentrations; increased tipranavir concentrations |
Modification of usual dosage of clarithromycin or tipranavir not necessary in patients with normal renal function; reduce clarithromycin dosage by 50% if Clcr 30–60 mL/minute and reduce by 75% if Clcr <30 mL/minute |
|
Corticosteroids (beclomethasone, betamethasone, budesonide, dexamethasone, fluticasone, methylprednisolone, prednisolone, prednisone, triamcinolone) |
Beclomethasone (orally inhaled, intranasal): Clinically important pharmacokinetic interactions not expected Budesonide, ciclesonide, fluticasone, mometasone (orally inhaled, intranasal): Increased corticosteroid concentrations possible; may result in adrenal insufficiency or Cushing's syndrome Betamethasone, methylprednisolone, triamcinolone (intra-articular or other local injections): Increased corticosteroid concentrations possible; may result in adrenal insufficiency or Cushing's syndrome Betamethasone or budesonide (systemic): Decreased tipranavir concentrations possible; increased corticosteroid concentrations, which may result in adrenal insufficiency or Cushing's syndrome Dexamethasone (systemic): Possible decreased tipranavir concentrations and increased dexamethasone concentrations Prednisolone or prednisone (systemic): Increased corticosteroid concentrations possible; may result in adrenal insufficiency or Cushing's syndrome |
Beclomethasone (orally inhaled, intranasal): Dosage adjustments not necessary Budesonide, ciclesonide, fluticasone, mometasone (orally inhaled, intranasal): Do not use concomitantly unless potential benefits of inhaled or intranasal corticosteroid outweigh risks of systemic corticosteroid adverse effects; consider alternative (e.g., beclomethasone) Betamethasone, methylprednisolone, triamcinolone (intra-articular or other local injections): Do not use concomitantly Betamethasone or budesonide (systemic): Do not use concomitantly unless potential benefits outweigh risks of systemic corticosteroid adverse effects Dexamethasone (systemic): Consider alternative corticosteroid for long-term use; if concomitant use necessary, monitor virologic response Prednisolone or prednisone (systemic): Consider concomitant use only if potential benefits outweigh risks of systemic corticosteroid adverse effects; if concomitant use necessary, monitor for adrenal insufficiency, Cushing's syndrome, and other corticosteroid-associated adverse effects |
|
Daclatasvir |
Data not available |
|
|
Darunavir |
No in vitro evidence of antagonistic antiretroviral effects |
|
|
Dasabuvir, ombitasvir, paritaprevir, and ritonavir |
Fixed combination of dasabuvir, ombitasvir, paritaprevir, and ritonavir (dasabuvir/ombitasvir/paritaprevir/ritonavir) or fixed combination of ombitasvir, paritaprevir, and ritonavir copackaged with dasabuvir (ombitasvir/paritaprevir/ritonavir with dasabuvir): Data not available |
Dasabuvir/ombitasvir/paritaprevir/ritonavir (fixed combination) or ombitasvir/paritaprevir/ritonavir with dasabuvir (copackaged): Experts state do not use concomitantly |
|
Delavirdine |
In vitro evidence of additive antiretroviral effects |
|
|
Didanosine |
Decreased didanosine concentrations and decreased tipranavir concentrations In vitro evidence of additive antiretroviral effects |
For optimal absorption, administer didanosine at least 2 hours before or after tipranavir |
|
Digoxin |
Possible increased digoxin concentrations |
Use concomitantly with caution; titrate digoxin dosage and monitor digoxin concentrations |
|
Disulfiram |
Potential pharmacokinetic interaction with alcohol contained in tipranavir capsules; possible disulfiram-like reaction |
|
|
Dolutegravir |
Decreased dolutegravir concentrations and AUC |
In integrase strand transfer inhibitor-naive (INSTI-naive) patients, use dolutegravir 50 mg twice daily; in INSTI-experienced patients with documented or suspected INSTI resistance, consider alternative to ritonavir-boosted tipranavir whenever possible |
|
Dronabinol |
Possible increased dronabinol concentrations |
Experts state monitor for dronabinol-associated adverse effects |
|
Dutasteride |
Possible increased dutasteride concentrations |
Experts state adjust dutasteride dosage as needed based on clinical effects and endogenous hormone concentrations |
|
Elbasvir and grazoprevir |
Fixed combination of elbasvir and grazoprevir (elbasvir/grazoprevir): Increased grazoprevir concentrations expected; possible increased risk of ALT elevations |
Elbasvir/grazoprevir: Concomitant use contraindicated |
|
Eluxadoline |
Increased eluxadoline concentrations expected |
Experts state use eluxadoline 75 mg twice daily and monitor for eluxadoline-associated adverse effects |
|
Eplerenone |
Increased eplerenone concentrations expected |
Experts state concomitant use contraindicated |
|
Efavirenz |
Decreased tipranavir concentrations and no change in efavirenz concentrations using tipranavir 500 mg twice daily and ritonavir 100 mg twice daily with efavirenz 600 mg once daily In vitro evidence of additive antiretroviral effects |
Some experts state dosage adjustments not necessary |
|
Elvitegravir and cobicistat |
Fixed combination of elvitegravir, cobicistat, emtricitabine, and tenofovir alafenamide (EVG/c/FTC/TAF) or fixed combination of elvitegravir, cobicistat, emtricitabine, and tenofovir disoproxil fumarate (EVG/c/FTC/TDF): Possible altered or suboptimal concentrations of elvitegravir, cobicistat, and/or tipranavir |
EVG/c/FTC/TAF or EVG/c/FTC/TDF: Do not use concomitantly |
|
Emtricitabine |
In vitro evidence of additive antiretroviral effects |
|
|
Enfuvirtide |
Increased tipranavir trough concentrations In vitro evidence of synergistic antiretroviral effects |
Dosage adjustments not recommended |
|
Ergot alkaloids (dihydroergotamine, ergotamine, methylergonovine) |
Potential for serious or life-threatening adverse effects (e.g., peripheral vasospasm, ischemia of extremities) |
Concomitant use contraindicated If treatment of uterine atony and excessive postpartum bleeding is indicated in a woman receiving tipranavir, use methylergonovine maleate (Methergine) only if alternative treatments cannot be used and if potential benefits outweigh risks; use methylergonovine at lowest dosage and shortest duration possible |
|
Estrogens and progestins |
Conjugated estrogens (equine or synthetic), estradiol: Possible decreased estrogen concentrations Drospirenone, medroxyprogesterone, progesterone: Possible increased progestin concentrations Ethinyl estradiol and norelgestromin (transdermal): Data not available Etonogestrel (subdermal implant): Data not available Oral contraceptives containing ethinyl estradiol and norethindrone: Decreased ethinyl estradiol concentrations; no effect on norethindrone concentrations |
Conjugated estrogens (equine or synthetic): Adjust estrogen dosage based on clinical effects Estradiol: Monitor for estrogen deficiency; adjust estrogen dosage based on clinical effects and endogenous hormone concentrations Drospirenone, medroxyprogesterone, progesterone: Adjust progestin dosage as needed based on clinical effects Ethinyl estradiol and norelgestromin (transdermal): Consider alternative or additional contraceptive or alternative antiretroviral Etonogestrel (subdermal implant): Consider alternative or additional contraceptive or alternative antiretroviral Oral contraceptives containing ethinyl estradiol and norethindrone: Consider alternative nonhormonal or additional contraception methods |
|
Etravirine |
Decreased etravirine concentrations and possible decreased antiretroviral efficacy; increased tipranavir concentrations No in vitro evidence of antagonistic antiretroviral effects |
Do not used concomitantly |
|
Fentanyl |
Possible increased fentanyl concentrations |
Carefully monitor for fentanyl therapeutic and adverse effects, including potentially fatal respiratory depression |
|
Finasteride |
Pharmacokinetic interaction not expected |
Experts state dosage adjustment not necessary |
|
Flibanserin |
Increased flibanserin concentrations expected |
Experts state concomitant use contraindicated |
|
Fosamprenavir |
Possible decreased amprenavir concentrations |
Concomitant use not recommended |
|
Glecaprevir and pibrentasvir |
Fixed combination of glecaprevir and pibrentasvir (glecaprevir/pibrentasvir): Increased glecaprevir and pibrentasvir concentrations expected |
Glecaprevir/pibrentasvir: Experts state do not use concomitantly |
|
Goserelin |
Pharmacokinetic interaction not expected |
Experts state dosage adjustments not necessary |
|
HMG-CoA reductase inhibitors (statins) |
Atorvastatin, lovastatin, rosuvastatin, simvastatin: Increased concentrations and AUCs of the antilipemic agent and increased risk of statin-associated adverse effects, including myopathy and rhabdomyolysis |
Atorvastatin: Avoid concomitant use Lovastatin: Concomitant use contraindicated Pitavastatin: Dosage adjustments not necessary Rosuvastatin: Dosage adjustments not necessary Simvastatin: Concomitant use contraindicated |
|
Immunosuppressive agents (cyclosporine, everolimus, sirolimus, tacrolimus) |
Potential for altered or increased immunosuppressive agent concentrations |
Adjust dosage of immunosuppressive agent to account for potential increased concentrations and monitor for immunosuppressive agent-associated adverse effects; monitor plasma concentrations of immunosuppressive agent |
|
Ivabradine |
Increased ivabradine concentrations expected |
Experts state concomitant use contraindicated |
|
Lamivudine |
Pharmacokinetic interactions unlikely In vitro evidence of additive antiretroviral effects |
|
|
Ledipasvir and sofosbuvir |
Fixed combination of ledipasvir and sofosbuvir (ledipasvir/sofosbuvir): Decreased ledipasvir and sofosbuvir concentrations expected; possible reduced HCV antiviral effects |
Ledipasvir/sofosbuvir: Concomitant use not recommended |
|
Leuprolide |
Pharmacokinetic interactions not expected |
Experts state dosage adjustments not necessary |
|
Loperamide |
Decreased loperamide concentrations; no clinically important change in tipranavir concentrations |
|
|
Lopinavir and ritonavir |
Fixed combination of lopinavir and ritonavir (lopinavir/ritonavir): Decreased lopinavir concentrations and AUC In vitro evidence of additive to antagonistic or additive to synergistic antiretroviral effects |
Lopinavir/ritonavir: Concomitant use not recommended |
|
Maraviroc |
No clinically important effect on maraviroc pharmacokinetics No in vitro evidence of antagonistic antiretroviral effects |
Recommended maraviroc dosage is 300 mg twice daily when used with ritonavir-boosted tipranavir, provided regimen does not include a potent CYP3A inhibitor or inducer |
|
Meperidine |
Potential for decreased meperidine concentrations, increased normeperidine concentrations |
Manufacturer of tipranavir does not recommend increasing meperidine dosage or concomitant long-term use because of potential for increased normeperidine concentrations and possible analgesic and CNS-stimulating activity (e.g., seizures) |
|
Methadone |
Decreased methadone concentrations; opiate withdrawal unlikely but may occur |
Methadone dosage adjustment may be necessary; monitor for opioid withdrawal and increase methadone dosage as clinically indicated |
|
Metronidazole |
Potential interaction with alcohol present in tipranavir capsules; possible disulfiram-like reaction |
|
|
Nelfinavir |
In vitro evidence of additive to antagonistic antiretroviral effects |
|
|
Nevirapine |
No clinically important effect on nevirapine concentrations; effect on tipranavir concentrations unknown In vitro evidence of additive antiretroviral effects |
Dosage adjustments not necessary |
|
Omeprazole |
Decreased omeprazole concentrations; no change in tipranavir concentrations |
Experts state concomitant use not recommended; if concomitant use necessary, consider increased omeprazole dosage based on clinical response |
|
Oral antidiabetic agents |
Canagliflozin: Decreased canagliflozin concentrations expected Glimepiride, glipizide, glyburide, pioglitazone, repaglinide, tolbutamide: Potential for altered concentrations of antidiabetic agents Saxagliptin or fixed combination of dapagliflozin and saxagliptin (dapagliflozin/saxagliptin): Increased saxagliptin concentrations expected |
Canagliflozin: If patient with estimated GFR >60 mL/minute per 1.73 m2 receiving canagliflozin 100 mg daily requires additional glycemic control, experts state consider increasing canagliflozin dosage to 300 mg daily Glimepiride, glipizide, glyburide, pioglitazone, repaglinide, tolbutamide: Careful glucose monitoring warranted Saxagliptin or dapagliflozin/saxagliptin: Use saxagliptin dosage of 2.5 mg once daily; do not use dapagliflozin/saxagliptin since the fixed combination contains 5 mg of saxagliptin |
|
Oxycodone |
Possible increased oxycodone concentrations |
Experts state monitor for oxycodone-associated adverse effects; oxycodone dosage reduction may be necessary |
|
Raltegravir |
Decreased raltegravir concentrations and AUC |
Raltegravir (Isentress): Dosage adjustments not needed Raltegravir 600-mg film-coated tablets (Isentress HD) : Concomitant use not recommended |
|
Ranolazine |
Increased ranolazine concentrations expected |
Experts state concomitant use contraindicated |
|
Rilpivirine |
Possible increased rilpivirine concentrations; not expected to affect tipranavir concentrations No in vitro evidence of antagonistic antiretroviral effects |
Dosage adjustments not necessary |
|
Ritonavir |
Increased tipranavir concentrations and AUC; concomitant low-dose ritonavir used to therapeutic advantage (ritonavir-boosted tipranavir) |
|
|
St. John’s wort (Hypericum perforatum) |
Potential decreased tipranavir concentrations; possible decreased antiretroviral efficacy and increased risk of antiretroviral resistance |
Concomitant use contraindicated |
|
Salmeterol |
Possible increased salmeterol concentrations and increased risk of salmeterol-associated adverse cardiovascular effects, including QT interval prolongation, palpitations, and sinus tachycardia |
Concomitant use not recommended |
|
Saquinavir |
Decreased saquinavir concentrations and AUC In vitro evidence of additive to antagonistic antiretroviral effects |
Concomitant use not recommended |
|
Selective serotonin-reuptake inhibitors (SSRIs) |
Citalopram, escitalopram, fluoxetine, paroxetine, sertraline: Specific data not available; possible increased SSRI concentrations Fluvoxamine: Possible altered (increased or decreased) tipranavir concentrations |
Citalopram, escitalopram, fluoxetine, paroxetine, sertraline: Titrate SSRI dosage based on clinical response Fluvoxamine: Experts state consider alternative to fluvoxamine |
|
Sildenafil |
Possible increased sildenafil concentrations and increased risk of sildenafil-associated adverse effects (e.g., hypotension, syncope, visual disturbances, prolonged erection) |
Sildenafil for treatment of pulmonary arterial hypertension (PAH): Concomitant use with ritonavir-boosted tipranavir contraindicated Sildenafil for treatment of erectile dysfunction: Do not exceed sildenafil dosage of 25 mg once every 48 hours; closely monitor for sildenafil-associated adverse effects (e.g., hypotension, syncope, visual disturbances, prolonged erection) |
|
Simeprevir |
Possible altered (increased or decreased) simeprevir concentrations due to CYP3A4 inhibition or induction by HIV PI |
Concomitant use not recommended. |
|
Sofosbuvir |
Decreased concentrations of sofosbuvir and metabolite (GS-331007) expected; may result in decreased sofosbuvir therapeutic effects |
Concomitant use not recommended |
|
Sofosbuvir and velpatasvir |
Fixed combination of sofosbuvir and velpatasvir (sofosbuvir/velpatasvir): Decreased sofosbuvir and velpatasvir concentrations expected |
Sofosbuvir/velpatasvir: Do not use concomitantly |
|
Sofosbuvir, velpatasvir, and voxilaprevir |
Fixed combination of sofosbuvir, velpatasvir, and voxilaprevir (sofosbuvir/velpatasvir/voxilaprevir): Decreased sofosbuvir and velpatasvir concentrations expected; effect on voxilaprevir not known |
Sofosbuvir/velpatasvir/voxilaprevir: Do not use concomitantly |
|
Spironolactone |
Pharmacokinetic interaction not expected |
Experts state dosage adjustments not necessary |
|
Stavudine |
Pharmacokinetic interaction unlikely In vitro evidence of additive antiretroviral effects |
|
|
Suvorexant |
Increased suvorexant concentrations expected |
Experts state concomitant use not recommended |
|
Tadalafil |
Possible increased tadalafil concentrations and increased risk of tadalafil-associated adverse effects (e.g., hypotension, syncope, visual disturbances, prolonged erection) |
Tadalafil for treatment of PAH in patients who have been receiving ritonavir-boosted tipranavir for ≥1 week: Use initial tadalafil dosage of 20 mg once daily; if tolerated, may increase dosage to 40 mg once daily Ritonavir-boosted tipranavir in patients receiving tadalafil for PAH: Discontinue tadalafil for at least 24 hours prior to initiating ritonavir-boosted tipranavir; after ≥1 week of the antiretroviral agent, may resume tadalafil at dosage of 20 mg once daily and, if tolerated, may increase dosage to 40 mg once daily Tadalafil for treatment of erectile dysfunction: Do not exceed tadalafil dosage of 10 mg once every 72 hours; closely monitor for tadalafil-related adverse effects (e.g., hypotension, syncope, visual disturbances, prolonged erection, syncope) Tadalafil for treatment of benign prostatic hyperplasia: Do not exceed tadalafil dosage of 2.5 mg once daily |
|
Tenofovir |
Decreased tenofovir concentrations and AUC; possible decreased tipranavir concentrations and AUC In vitro evidence of additive antiretroviral effects |
Dosage adjustments not necessary |
|
Testosterone |
Possible decreased testosterone concentrations |
Experts state adjust testosterone dosage as needed based on clinical effects and endogenous hormone concentrations |
|
Trazodone |
Possible increased trazodone concentrations and AUC Increased risk of trazodone-associated adverse effects (e.g., nausea, dizziness, hypotension, syncope) |
Use with caution; consider reduced trazodone dosage; use lowest possible trazodone dosage and monitor for CNS and cardiovascular adverse effects |
|
Tricyclic antidepressants (amitriptyline, doxepin, desipramine, imipramine, nortriptyline) |
Amitriptyline, desipramine, doxepin, imipramine, nortriptyline: Possible increased concentrations of the tricyclic antidepressant |
Amitriptyline, imipramine, doxepin, nortriptyline: Use lowest possible antidepressant dosage; titrate antidepressant dosage based on clinical assessment and/or antidepressant concentrations Desipramine: Use reduced desipramine dosage and monitor plasma desipramine concentrations |
|
Valacyclovir |
No clinically important effect on tipranavir or acyclovir concentrations or AUC |
|
|
Vardenafil |
Possible increased vardenafil concentrations and increased risk of vardenafil-associated adverse effects (e.g., hypotension, syncope, visual disturbances, prolonged erection) |
Vardenafil for treatment of erectile dysfunction: Do not exceed vardenafil dosage of 2.5 mg once every 72 hours; closely monitor for vardenafil-related adverse effects (e.g., hypotension, syncope, visual changes, prolonged erection) |
|
Vitamin E |
Potential for increased risk of bleeding with high-dose vitamin E |
Use concomitantly with caution |
|
Zidovudine |
Decreased zidovudine AUC; clinical importance unknown In vitro evidence of additive antiretroviral effects |
Appropriate dosage for concomitant use not established |
|
Zolpidem |
Possible increased zolpidem concentrations |
Experts state initiate zolpidem using low dosage; reduced dosage may be needed |
Tipranavir Pharmacokinetics
Absorption
Bioavailability
Tipranavir is administered concomitantly with low-dose ritonavir (ritonavir-boosted tipranavir). Ritonavir decreases metabolism of tipranavir, resulting in increased tipranavir plasma concentrations.
Following >2 weeks of multiple oral doses given without regard to meals, peak plasma tipranavir concentrations attained approximately 3 hours after a dose.
Steady state attained in most patients after 7–10 days. Steady-state trough concentrations are 70% lower than day 1, presumably due to intestinal P-gp induction.
Food
Compared with administration in the fasting state, administration of tipranavir (as capsules or oral solution) and ritonavir (as capsules) with a meal (500–682 kcal, 23–25% calories from fat) does not have a clinically important effect on tipranavir peak plasma concentrations or AUC.
Effect of food on administration of tipranavir (as capsules or oral solution) with ritonavir (as tablets) not evaluated.
Distribution
Extent
Not known whether distributed into CSF or semen.
Not known whether distributed into milk.
Plasma Protein Binding
>99%.
Binds to albumin and α1-acid-glycoprotein.
Elimination
Metabolism
Tipranavir extensively metabolized by CYP3A4. Only minimal metabolism of tipranavir occurs when administered with ritonavir 200 mg.
Oral clearance of tipranavir decreased when administered with ritonavir; this may indicate decreased first-pass effect.
Elimination Route
Following administration of ritonavir-boosted tipranavir, eliminated principally in feces as unchanged tipranavir. Approximately 82% of tipranavir dose excreted in feces and 4% excreted in urine.
Half-life
Effective mean elimination half-life at steady-state is 4.8–6 hours following administration of ritonavir-boosted tipranavir with a light meal.
Special Populations
Renal impairment: Pharmacokinetics not studied, but decreased total body clearance not expected since renal clearance of tipranavir is negligible.
Mild hepatic impairment (Child-Pugh class A): Increased plasma concentrations, but dosage adjustments not needed.
Moderate or severe impairment (Child-Pugh class B and C): Pharmacokinetics not evaluated.
Higher tipranavir concentrations reported in females compared with males; dosage adjustments not required.
Stability
Storage
Oral
Capsules
2–8°C prior to opening bottle; after opening bottle, store at 25°C (may be exposed to 15–30°C) and use within 60 days.
Oral Solution
25°C (may be exposed to 15–30°C); do not refrigerate or freeze. After opening bottle, use within 60 days.
Actions and Spectrum
-
Tipranavir must be administered in conjunction with low-dose ritonavir (ritonavir-boosted tipranavir).
-
Tipranavir is extensively metabolized by CYP3A; ritonavir is a potent inhibitor of CYP3A. Concomitant use of these drugs results in decreased metabolism and increased plasma concentrations of tipranavir.
-
Antiretroviral activity is due to tipranavir.
-
Active against HIV-1; has some in vitro activity against HIV-2.
-
Tipranavir inhibits replication of HIV-1 by interfering with HIV proteases.
-
Tipranavir-resistant HIV-1, including strains with decreased susceptibility to other HIV PIs, has been reported.
Advice to Patients
-
Critical nature of compliance with HIV therapy and importance of remaining under the care of a clinician. Importance of taking as prescribed; do not alter or discontinue antiretroviral regimen without consulting clinician.
-
Importance of using tipranavir with low-dose ritonavir (ritonavir-boosted tipranavir); importance of using these 2 drugs in conjunction with other antiretrovirals.
-
Antiretroviral therapy is not a cure for HIV infection; opportunistic infections and other complications associated with HIV disease may still occur. Sustained decreases in plasma HIV RNA have been associated with reduced risk of progression to AIDS and death.
-
Advise patients that effective antiretroviral regimens can decrease HIV concentrations in blood and genital secretions and strict adherence to such regimens in conjunction with risk-reduction measures may decrease, but cannot absolutely eliminate, the risk of secondary transmission of HIV to others. Importance of continuing to practice safer sex (e.g., using latex or polyurethane condoms to minimize sexual contact with body fluids), never sharing personal items that can have blood or body fluids on them (e.g., toothbrushes, razor blades), and never reusing or sharing needles.
-
Importance of reading patient information provided by the manufacturer.
-
Importance of taking tipranavir at the same time as ritonavir. If tipranavir is taken with ritonavir capsules or oral solution, take the drugs with or without meals. If tipranavir is taken with ritonavir tablets, take the drugs with a meal.
-
Importance of swallowing tipranavir capsules whole; capsules should not be chewed.
-
If a dose is missed, take the dose as soon as it is remembered and take next dose at regularly scheduled time. If a dose is skipped, do not take a double dose to make up for the missed dose.
-
Importance of patient informing their clinician if they are allergic to sulfonamides.
-
Possibility of fatal or nonfatal intracranial hemorrhage. Importance of informing clinician of unusual or unexplained bleeding.
-
Advise patients that severe liver disease (including fatalities) reported. Importance of discontinuing ritonavir-boosted tipranavir and seeking medical attention if signs or symptoms of liver disease (fatigue, malaise, anorexia, nausea, jaundice, bilirubinuria, acholic stools, liver tenderness, hepatomegaly) occur.
-
Need for periodic clinical and laboratory monitoring, including liver function tests, prior to and during treatment. Importance of extra vigilance in HIV-infected patients with chronic HBV or HCV coinfection because of increased risk of hepatotoxicity.
-
Possibility of rash. Importance of discontinuing ritonavir-boosted tipranavir and seeking medical attention if rash with or without joint pain or stiffness, throat tightness, generalized itching, muscle aches, fever, redness, blisters, or skin peeling occurs.
-
Redistribution/accumulation of body fat may occur with antiretroviral therapy, with as yet unknown long-term health effects.
-
Importance of informing clinicians of existing or contemplated concomitant therapy, including prescription and OTC drugs (e.g., vitamin E supplements) and herbal products (e.g., St. John’s wort), and any concomitant illnesses.
-
Advise patients receiving selective phosphodiesterase type 5 (PDE5) inhibitors (e.g., sildenafil, tadalafil, vardenafil) that they may be at increased risk of PDE5 inhibitor-associated adverse effects (e.g., hypotension, syncope, visual disturbances, priapism) and that any symptoms should be promptly reported to their clinician. Ritonavir-boosted tipranavir should not be used concomitantly with sildenafil used for treatment of pulmonary arterial hypertension (PAH).
-
Importance of women using a reliable nonhormonal (e.g., barrier) method of contraception because of the potential interaction with hormonal contraceptives.
-
Importance of women informing clinicians if they are or plan to become pregnant or plan to breast-feed. Advise HIV-infected women not to breast-feed.
-
Importance of advising patients of other important precautionary information. (See Cautions.)
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
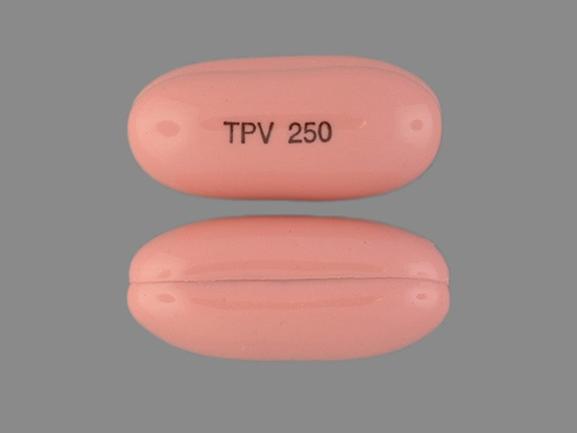
Oral |
Capsules |
250 mg |
Aptivus |
Boehringer Ingelheim |
|
Solution |
100 mg/mL |
Aptivus |
Boehringer Ingelheim |
AHFS DI Essentials™. © Copyright 2024, Selected Revisions March 5, 2018. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
Reload page with references included
More about tipranavir
- Check interactions
- Compare alternatives
- Side effects
- Dosage information
- During pregnancy
- Drug class: protease inhibitors
- Breastfeeding
- En español