Tachycardia
Medically reviewed by Drugs.com. Last updated on Aug 4, 2025.
What do I need to know about tachycardia?
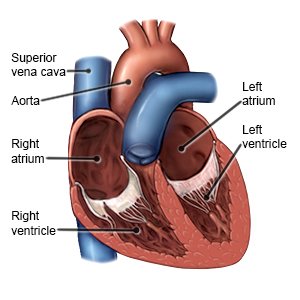
Tachycardia (fast heart rate) is when your heart rate is 100 beats per minute or more at rest.
 |
What causes or increases my risk for tachycardia?
It is normal for the heart rate to increase with activity or exercise and then decrease when you stop. A fast heart rate at rest may be caused by any of the following:
- Anxiety, stress, or pain
- Fever
- Physical fatigue or strenuous exercise
- Large amounts of caffeine such as coffee, tea, and energy drinks
- Heavy alcohol use, cigarette smoking, or drugs such as cocaine
- Some medicines, such as inhalers, cold medicines, and hypertension medicines
- Increased thyroid hormone level
What other symptoms may I have with a fast heart rate?
You may have no other symptoms with your fast heart rate, or you may have any of the following:
- Dizziness or lightheadedness
- Chest pain
- Fluttering or pounding heart
- Shortness of breath
How is a fast heart rate treated?
You may need treatment if your fast heart rate continues or happens often. You may need medicine, procedures, or surgery. Your provider may also send you to a cardiologist for other tests.
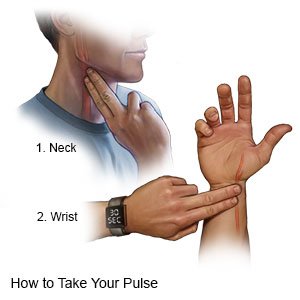
How do I check my heart rate (pulse)?
Your healthcare provider will show you how to check your pulse, and how often to check it. Write down how fast your pulse is and if it feels regular or like it is skipping beats. Also write down the activity you were doing if your heart rate is above 100. Bring the information with you to your follow-up appointment.
 |
What can I do to help manage or prevent a fast heart rate?
- Talk to your healthcare provider about all your current medicines. He or she may change a medicine if it is causing your fast heart rate. Do not stop taking any medicine unless directed by your provider.
- Have less caffeine. Caffeine can increase your heart rate.
- Limit or do not drink alcohol. Alcohol can increase your heart rate. Ask your healthcare provider if it is okay for you to drink any alcohol. He or she can help you set limits for the number of drinks you have in 24 hours and in a week. A drink of alcohol is 12 ounces of beer, 5 ounces of wine, or 1½ ounces of liquor.
- Do not smoke. Nicotine and other chemicals in cigarettes can cause damage to your heart. Ask your healthcare provider for information if you currently smoke and need help to quit. E-cigarettes or smokeless tobacco still contain nicotine. Talk to your healthcare provider before you use these products.
- Do not use illegal drugs. Drugs such as meth and cocaine can increase your heart rate. Talk to your healthcare provider if you use illegal drugs and want to quit.
- Get more rest. Fatigue can cause your heart rate to increase. Ask your healthcare provider about the best exercise plan for you.
- Eat heart-healthy foods. These include fruits, vegetables, whole-grain breads, low-fat dairy products, beans, lean meats, and fish. Replace butter and margarine with heart-healthy oils such as olive oil and canola oil.

- Exercise regularly and maintain a healthy weight. Ask about the best exercise plan for you. Ask your healthcare provider what a healthy weight is for you. Ask him or her to help you create a safe weight loss plan if you are overweight.
- Learn ways to cope with stress. Stress, fear, and anxiety can cause a fast heart rate. Your healthcare provider may recommend relaxation techniques and deep breathing exercises. Your healthcare provider may recommend you talk to someone about your stress or anxiety, such as a counselor or a trusted friend.
Call your local emergency number (911 in the US) or have someone call if:
- You have any of the following signs of a heart attack:
- Squeezing, pressure, or pain in your chest
- You may also have any of the following:
- Discomfort or pain in your back, neck, jaw, stomach, or arm
- Shortness of breath
- Nausea or vomiting
- Lightheadedness or a sudden cold sweat
- You cannot be woken.
When should I call my doctor?
- Your pulse is faster than you were told it should be.
- You have a fast heart rate often.
- You feel weak or dizzy.
- You have questions or concerns about your condition or care.
Care Agreement
You have the right to help plan your care. Learn about your health condition and how it may be treated. Discuss treatment options with your healthcare providers to decide what care you want to receive. You always have the right to refuse treatment. The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
Learn more about Tachycardia
Treatment options
Care guides
Symptoms and treatments
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
