Ovarian Cyst
Medically reviewed by Drugs.com. Last updated on Aug 4, 2025.
What is an ovarian cyst?
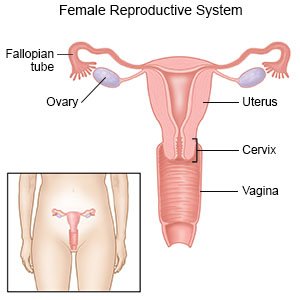
An ovarian cyst is a fluid-filled sac that grows in or on an ovary. You have 2 ovaries, 1 on each side of your uterus. They are small, about the size and shape of an almond. Ovarian cysts are common in women who have regular monthly cycles. During your monthly cycle, eggs are released from the ovaries. The cyst usually contains fluid but may sometimes have blood or tissue in it. Most ovarian cysts are harmless and go away without treatment in a few months. Some cysts can grow large, cause pain, or break open.
 |
What causes an ovarian cyst?
- Problems with your hormones
- Medicines that help you ovulate
- Endometriosis
- Pregnancy
- A severe infection in your pelvis
What are the signs and symptoms of an ovarian cyst?
You may have pressure, bloating or swelling in your lower abdomen on the side of the cyst. You may also have dull or sharp pain that may come and go. The following are less common signs and symptoms:
- A dull ache in your lower back and thighs
- Unusual vaginal bleeding
- Weight gain you did not expect or plan
- Pain during your monthly cycle
- Tenderness in your breasts
- Trouble completely emptying your bowels or bladder
- The need to urinate often
- Pain during sex
How is an ovarian cyst diagnosed?
- Blood tests may show what type of cyst you have and if you need treatment.
- A pelvic exam may help your healthcare provider feel an ovarian cyst.
- A pelvic ultrasound may show a cyst on your ovary. An ultrasound wand uses sound waves to show pictures on a monitor. The wand is inserted into your vagina and guided up toward your uterus.
How is an ovarian cyst treated?
Treatment will depend on your age, symptoms, and the kind of cyst you have. You may need any of the following:
- Watchful waiting may be recommended. This means the cyst is not treated right away. You will need to watch for any signs or symptoms that the cyst is growing. You may need to return for one or more ultrasounds after a certain period of time. These will show if your cyst has changed in size.
- Medicines:
- Birth control pills may help control your monthly cycle, prevent cysts, or cause them to shrink.
- Acetaminophen decreases pain and fever. It is available without a doctor's order. Ask how much to take and how often to take it. Follow directions. Read the labels of all other medicines you are using to see if they also contain acetaminophen, or ask your doctor or pharmacist. Acetaminophen can cause liver damage if not taken correctly.
- NSAIDs , such as ibuprofen, help decrease swelling, pain, and fever. This medicine is available with or without a doctor's order. NSAIDs can cause stomach bleeding or kidney problems in certain people. If you take blood thinner medicine, always ask your healthcare provider if NSAIDs are safe for you. Always read the medicine label and follow directions.
- Prescription pain medicine may be given. Ask your healthcare provider how to take this medicine safely. Some prescription pain medicines contain acetaminophen. Do not take other medicines that contain acetaminophen without talking to your healthcare provider. Too much acetaminophen may cause liver damage. Prescription pain medicine may cause constipation. Ask your healthcare provider how to prevent or treat constipation.
- Surgery may be needed to remove the ovarian cyst.
How can I manage ovarian cysts?
You can manage a current cyst and help healthcare providers find future cysts early.
- Apply heat to decrease pain and cramping from a cyst. Sit in a warm bath, or place a heating pad (turned on low) on your abdomen. Do this for 15 to 20 minutes every hour for comfort.
- Get regular pelvic exams or Pap smears. This will help providers find any new ovarian cysts. Tell your healthcare provider about any unusual changes in your monthly cycle.
Call your local emergency number (911 in the US) if:
- You have severe pain with fever and vomiting.
- You have sudden, severe abdominal pain.
- You are too weak, faint, or dizzy to stand up.
- You are breathing very quickly.
When should I call my doctor?
- Your periods are early, late, or more painful than usual.
- You have questions or concerns about your condition or care.
Care Agreement
You have the right to help plan your care. Learn about your health condition and how it may be treated. Discuss treatment options with your healthcare providers to decide what care you want to receive. You always have the right to refuse treatment. The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
