Flecainide (Monograph)
Drug class: Class Ic Antiarrhythmics
VA class: CV300
Chemical name: N-(2-Piperidinylmethyl)-2,5-bis(2,2,2-trifluoroethoxy)benzamide monoacetate
Molecular formula: C17H20F6N2O3•C2H4O2
CAS number: 54143-56-5
Warning
- Mortality
-
In the Cardiac Arrhythmia Suppression Trial (CAST), excessive mortality and nonfatal cardiac arrest reported in patients with asymptomatic non-life-threatening ventricular arrhythmias (e.g., premature ventricular contractions [PVCs]) and recent MI (>6 days, but <2 years previously) who were receiving flecainide (5.1%) compared with placebo (2.3%). (See Mortality under Cautions.)
-
Although not known whether these findings can be extrapolated to other patient populations (e.g., patients without recent MI), it is prudent to consider the risks of class Ic antiarrhythmic agents in addition to the lack of evidence of improved survival generally unacceptable in patients without life-threatening ventricular arrhythmias, even in patients experiencing unpleasant, but non-life-threatening symptoms.
- Proarrhythmic Effects in Patients with Atrial Fibrillation/Flutter
-
Do not use in patients with chronic atrial fibrillation because of risk of ventricular proarrhythmia (e.g., PVCs, VT, VF, death). (See Patients with Chronic Atrial Fibrillation under Cautions.)
-
Some patients with atrial flutter may develop 1:1 AV conduction. Paradoxically, an increase in ventricular rate also may occur in patients with atrial fibrillation; concomitant use of drugs with negative chronotropic effects (e.g., digoxin, β-adrenergic blocking agents) may reduce this risk.
Introduction
Local anesthetic-type class Ic antiarrhythmic agent.
Uses for Flecainide
Ventricular Arrhythmias
Suppression and prevention of recurrent ventricular arrhythmias (e.g., sustained VT) that, in the clinician’s judgment, are considered life-threatening. (See Boxed Warning.)
Because of arrhythmogenic potential and associated risk of death, use of flecainide for less severe arrhythmias (e.g., PVCs) not recommended.
No evidence that use is associated with beneficial effect on mortality or sudden death.
Supraventricular Tachyarrhythmias
Prevention of paroxysmal supraventricular tachycardia (PSVT), including AV nodal reentrant tachycardia and AV reentrant tachycardia (e.g., Wolff-Parkinson-White syndrome); other symptomatic, disabling, supraventricular tachycardias of unspecified mechanisms; and symptomatic, disabling paroxysmal atrial fibrillation/flutter (PAF) in patients without structural heart disease.
One of several drugs that may be used for ongoing management of PSVT in patients without structural or ischemic heart disease; however, because of adverse effects, use generally reserved for patients in whom other therapies (e.g., catheter ablation, β-adrenergic blocking agents, diltiazem, verapamil) are ineffective or contraindicated.
Considered a drug of choice for pharmacologic cardioversion of atrial fibrillation or flutter† [off-label].
May be used for ongoing management of other supraventricular tachycardias (e.g., focal atrial tachycardia† [off-label], junctional tachycardia† [off-label]).
Because of risk of proarrhythmia, do not use in patients with structural heart disease or ischemic heart disease.
Flecainide Dosage and Administration
General
-
Monitor plasma flecainide concentrations when feasible; monitoring is required in patients with severe hepatic or renal impairment, and recommended in other patients in whom elimination of the drug may be impaired (e.g., those with moderate renal impairment or CHF, or receiving concomitant amiodarone). Maintain trough plasma flecainide concentrations at <0.7–1 mcg/mL since concentrations above this range associated with higher rate of adverse cardiac effects. (See Plasma Concentrations under Pharmacokinetics.)
-
Clinical and ECG monitoring of cardiac function is recommended during therapy.
-
In patients with sustained VT, initiate therapy in hospital setting with ECG monitoring regardless of cardiac status. Some clinicians recommend that withdrawal of therapy also should occur in a hospital setting under continuous ECG monitoring.
-
If used in pediatric patients, administer under direct supervision of experienced cardiologist. (See Pediatric Use under Cautions.)
Transferring from Other Antiarrhythmic Agents
-
A transition period is suggested in patients transferring from therapy with another antiarrhythmic agent to flecainide. Allow ≥2–4 half-lives of the previous antiarrhythmic to elapse prior to initiating flecainide.
-
Consider hospitalization for transition if discontinuance of the current antiarrhythmic drug is likely to produce life-threatening arrhythmias.
Administration
Oral Administration
Administer orally in 2 equally divided doses daily at 12-hour intervals.
If arrhythmias are not adequately controlled or drug is not well tolerated with twice-daily dosing, may administer at 8-hour intervals.
Dosage
Available as flecainide acetate; dosage expressed in terms of the salt.
Adjust dosage carefully according to individual patient response and tolerance.
To minimize effects on cardiac conduction, use lowest possible effective dosage. (See Effects on Cardiac Conduction under Cautions.)
Steady-state plasma concentrations and optimum therapeutic effect may not be attained for 3–5 days (or longer in some patients); do not increase dosage more frequently than once every 4 days.
Oral loading doses generally not used since arrhythmogenicity and congestive heart failure may occur. However, single oral loading doses (e.g., 200–300 mg) have been used for conversion of recent-onset atrial fibrillation to normal sinus rhythm† [off-label] (“pill-in-the-pocket” approach) in individuals with mild or no structural heart disease.
Pediatric Patients
Supraventricular and Ventricular Arrhythmias
Oral
Consult specialized references. (See Pediatric Use under Cautions.)
Infants <6 months of age: Initial dosage approximately 50 mg/m2 daily, divided into 2 or 3 equally spaced doses.
Children ≥6 months of age: Initial dosage may be increased to 100 mg/m2 daily.
Obtain plasma trough (<1 hour before dosing) flecainide concentrations and ECG at steady state (after at least 5 doses) after initiation of therapy or after any change in dosing. Plasma drug concentrations may be labile in patients receiving higher dosages. Small changes in dosage may lead to disproportionate increases in plasma drug concentrations.
During first year of therapy, manufacturer suggests that a 12-lead ECG and plasma trough flecainide concentration be obtained whenever the patient is seen for clinical follow-up. Usual therapeutic concentration in children is 200–500 ng/mL, although concentrations up to 800 ng/mL may be required.
Adults
Ventricular Arrhythmias
Oral
Sustained VT: Initially, 100 mg every 12 hours. May increase dosage in increments of 50 mg twice daily every 4 days until optimum response is obtained; maximum recommended dosage is 400 mg daily.
Higher initial dosages and more rapid dosage increases associated with increased incidence of proarrhythmic events and congestive heart failure, particularly during first few days of therapy.
Dosages >300 mg daily generally not required.
Supraventricular Tachyarrhythmias
Oral
PSVT or PAF: Initially, 50 mg every 12 hours. May increase dosage in increments of 50 mg twice daily every 4 days until optimum response is obtained; maximum recommended dosage is 300 mg daily.
Self-administration for Conversion of PAF† [off-label]
OralPatients ≥70 kg: 300 mg as a single oral loading dose 5 minutes after onset of palpitations.
Patients <70 kg: 200 mg as a single oral loading dose 5 minutes after onset of palpitations.
Remain in sitting or supine position until resolution of palpitations or for ≥4 hours after dose. Seek medical advice if palpitations do not resolve within 6–8 hours, if previously unexperienced symptoms (e.g., dyspnea, presyncope, syncope) occur, or if marked increase in heart rate occurs.
Do not take more than one dose during a 24-hour period.
Prescribing Limits
Pediatric Patients
Supraventricular and Ventricular Arrhythmias
Oral
Maximum 200 mg/m2 daily.
Adults
Ventricular Arrhythmias
Oral
Maximum 400 mg daily.
Supraventricular Tachyarrhythmias
Oral
Maximum 300 mg daily for treatment of paroxysmal supraventricular arrhythmias.
Self-administration for Conversion of Paroxysmal Atrial Fibrillation†
OralMaximum 300 mg as single oral dose in 24-hour period for adults ≥70 kg.
Maximum 200 mg as single oral dose in 24-hour period for adults <70 kg.
Special Populations
Hepatic Impairment
Monitor plasma concentrations closely to guide dosage adjustments. (See Hepatic Impairment under Cautions.)
Increase dosage with caution and at intervals of >4 days.
Renal Impairment
In patients with severe renal impairment (Clcr ≤35 mL/minute), initial dosage of 100 mg once daily or 50 mg twice daily recommended. (See Renal Impairment under Cautions.)
In patients with moderate renal impairment, initial dosage of 100 mg every 12 hours recommended.
Monitor plasma concentrations closely to guide dosage adjustments.
Increase dosage with caution and at intervals of >4 days; closely monitor for adverse cardiac effects or other toxicity.
Cautions for Flecainide
Contraindications
-
Preexisting 2nd or 3rd degree AV block or bifascicular block (right bundle branch block associated with left hemiblock) unless pacemaker is in place.
-
Cardiogenic shock.
-
Known hypersensitivity to flecainide.
Warnings/Precautions
Warnings
Mortality
Increased risk of mortality or nonfatal cardiac arrest reported in post-MI patients with non-life-threatening ventricular arrhythmias. (See Boxed Warning.)
Limit use of flecainide in patients with ventricular arrhythmias to those with life-threatening arrhythmias; use in patients with less severe ventricular arrhythmias, even when symptomatic, is not recommended.
Do not use in patients with recent or prior MI.
Patients with Chronic Atrial Fibrillation
Manufacturer states not adequately studied and not recommended in patients with chronic atrial fibrillation; possible VT or VF or paradoxical increase in ventricular rate. (See Boxed Warning.)
Arrhythmogenic Effects
Potential for new and/or more severe or potentially fatal arrhythmias (principally ventricular tachyarrhythmias but also increased PVCs or supraventricular arrhythmias). Risk appears to be related to dosage and underlying cardiac disease.
Clinical and ECG evaluations are essential prior to and during therapy. Follow recommended dosage schedule closely. Monitor plasma drug concentrations and avoid concentrations >1 mcg/mL. If possible, avoid concomitant use of other antiarrhythmic agents. (See Antiarrhythmic Agents under Interactions.)
Heart Failure
Potential for new or worsened CHF, particularly in patients with cardiomyopathy, preexisting severe CHF (NYHA class III or IV), or ejection fraction <30%.
If CHF or myocardial dysfunction develops, dosage reduction, discontinuance of therapy, or modification of other drug therapy (e.g., digoxin, diuretics) may be necessary.
Use with caution in patients with a history of CHF or myocardial dysfunction, particularly those with advanced failure or dysfunction. Carefully monitor such patients; do not exceed recommended initial dosage. Monitor plasma flecainide concentrations and adjust dosage to maintain trough concentrations <0.7–1 mcg/mL.
Effects on Cardiac Conduction
To minimize effects on cardiac conduction, use lowest possible effective dosage.
Consider dosage reduction if PR interval increases to ≥300 ms, QRS duration increases to ≥180 ms, or QTc interval increases substantially.
If 2nd or 3rd degree AV block or bifascicular block occurs, discontinue flecainide unless a temporary or implanted artificial ventricular pacemaker is in place to ensure adequate ventricular rate.
Torsades de pointes-type arrhythmia reported rarely.
Patients with Sinus Node Dysfunction
Potential for sinus bradycardia, pause, or arrest in patients with sick sinus syndrome (including bradycardia-tachycardia syndrome); use with extreme caution, if at all, in such patients.
Changes in Endocardial Pacing Threshold
Potential for increased endocardial pacing threshold and suppression of ventricular escape rhythms.
Use with caution in patients with permanent artificial pacemakers or temporary pacing electrodes; do not administer to patients with existing poor thresholds or nonprogrammable artificial pacemakers unless suitable pacing rescue is available.
In patients with pacemakers, determine pacing threshold before and 1 week after initiating therapy and at regular intervals thereafter.
Potassium Imbalance
Correct any preexisting potassium imbalance before initiating flecainide.
Specific Populations
Pregnancy
Category C.
Lactation
Distributed into milk.
Pediatric Use
Safety and efficacy not established in randomized controlled studies. Limited data suggest that flecainide may be useful for management of refractory supraventricular tachycardias in pediatric patients.
Possible proarrhythmic effects. Has been associated with cardiac arrest and sudden death in pediatric patients with structural heart disease. Because of these risks, flecainide generally not a preferred antiarrhythmic drug in pediatric patients.
Use should be supervised directly by a cardiologist experienced in the treatment of arrhythmias in children. Initiate therapy in hospital setting equipped with ECG monitoring.
Hepatic Impairment
Elimination may be markedly prolonged; use in patients with substantial hepatic impairment only if benefits clearly outweigh risks. Monitor plasma concentrations. (See Hepatic Impairment under Dosage and Administration.)
Renal Impairment
Elimination may be impaired; use with caution. Monitor plasma concentrations. (See Renal Impairment under Dosage and Administration.)
Common Adverse Effects
Dizziness, visual disturbances, dyspnea, headache, nausea, fatigue, palpitation, chest pain.
Drug Interactions
Metabolized by CYP2D6.
Antiarrhythmic Agents
Potential for increased risk of arrhythmogenic effects; additive, synergistic, or antagonistic cardiac effects; or additive adverse effects.
Avoid concomitant use with other antiarrhythmic agents if possible; reserve such concomitant therapy for carefully selected patients with severe refractory arrhythmias. (See Transferring from Other Antiarrhythmic Agents under Dosage and Administration.)
Diuretics
No apparent interaction when used concomitantly with diuretics.
Drugs Affecting Hepatic Microsomal Enzymes
CYP2D6 inhibitors: Possible increase in plasma flecainide concentrations, particularly in extensive metabolizers.
Protein-bound Drugs
Pharmacokinetic interaction unlikely.
Specific Drugs and Foods
|
Drug or Food |
Interaction |
Comments |
|---|---|---|
|
Acidifying agents (e.g., ammonium chloride) |
Urinary excretion of flecainide increased and elimination half-life decreased in presence of very acidic urine |
Flecainide dosage adjustment may be necessary |
|
Alkalinizing agents (e.g., high-dose antacids, carbonic anhydrase inhibitors, sodium bicarbonate) |
Urinary excretion of flecainide decreased and elimination half-life increased in presence of very alkaline urine |
Flecainide dosage adjustment may be necessary |
|
Amiodarone |
Increased plasma flecainide concentrations by twofold |
Reduce flecainide dosage by 30–50% and monitor patient closely; monitor plasma flecainide concentrations and adjust dosage as necessary |
|
Antacids |
No effect on rate or extent of flecainide absorption |
|
|
β-adrenergic blocking agents (e.g., propranolol) |
Potential for additive negative inotropic effects; effects on PR interval were less than additive Increased plasma concentrations of flecainide and propranolol by 20 and 30%, respectively |
|
|
Carbamazepine |
Increased rate of flecainide elimination |
|
|
Cimetidine |
Possible reduction in nonrenal and renal clearance of flecainide Increased elimination half-life and plasma concentrations of flecainide by 10 and 30%, respectively |
Possible flecainide dosage reduction; further study needed |
|
Clozapine |
Possible increased plasma flecainide concentrations |
Use with caution and monitor closely, especially patients with extensive-metabolizer phenotype Adjust flecainide and/or clozapine dosage as necessary |
|
Digoxin |
Possible increased plasma digoxin concentrations |
Monitor for signs of digoxin toxicity |
|
Diltiazem |
Experience is too limited to recommend concomitant use |
|
|
Disopyramide |
Potential for negative inotropic effects |
Use concomitantly only if potential benefits outweigh risk |
|
Milk |
Possible reduction of flecainide absorption in infants |
Consider reducing flecainide dosage when milk is removed from infant’s diet |
|
Nifedipine |
Experience is too limited to recommend concomitant use |
|
|
Phenytoin |
Possible increased rate of flecainide elimination |
|
|
Phenobarbital |
Possible increased rate of flecainide elimination |
|
|
Quinidine |
Possible increased plasma flecainide concentrations |
|
|
Verapamil |
Potential for additive negative inotropic effects |
Use concomitantly only if potential benefits outweigh risk |
Flecainide Pharmacokinetics
Absorption
Bioavailability
Rapidly and almost completely absorbed following oral administration, with peak plasma concentrations generally reached within approximately 3 hours (range: 1–6 hours). Absolute bioavailability is approximately 85–90%.
No substantial first-pass metabolism.
Food
Food may slightly decrease rate but does not affect extent of absorption.
Milk may inhibit absorption in infants.
Plasma Concentrations
Trough plasma concentrations are 0.2–1 mcg/mL in most patients successfully treated with flecainide.
In children, usual therapeutic concentration is 0.2–0.5 mcg/mL, although concentrations up to 0.8 mcg/mL may be required.
Increased risk of adverse cardiac effects (e.g., conduction defects, bradycardia) at plasma concentrations >0.7–1 mcg/mL, particularly when concentrations >1 mcg/mL.
Distribution
Extent
Distributed into milk.
Plasma Protein Binding
About 40–50%.
Elimination
Metabolism
Extensively metabolized, probably in the liver, to 2 major metabolites and at least 3 unidentified minor metabolites; unlikely that major metabolites contribute substantially to therapeutic or toxic effects.
CYP2D6 involved in metabolism.
Elimination Route
Excreted almost completely in urine; only small amounts of drug and/or metabolites excreted in feces.
Plasma clearance is decreased when urine pH ≥8.
Half-life
Biphasic; elimination half-life is about 11.5–16 hours following single or multiple doses in healthy adults. Elimination half-life following multiple doses in patients with PVCs slightly longer, averaging 19–22 hours (range: 12–30 hours).
Special Populations
In patients with PVCs, CHF, or renal or hepatic impairment, elimination half-life is prolonged.
In children, elimination half-life tends to decrease with age (around 29 hours at birth, 11–12 hours by 3 months of age, 6–8 hours by 1–12 years of age, and 11–12 hours by 12–15 years of age).
Stability
Storage
Oral
Tablets
Tight, light-resistant containers at 20–25°C.
Actions
-
Membrane-stabilizing antiarrhythmic agent; exhibits local anesthetic effects.
-
Principal effect on cardiac tissue appears to be concentration-dependent inhibition of transmembrane influx of extracellular sodium ions via fast sodium channels.
-
Combines with fast sodium channels within the myocardium and inhibits rapid sodium influx, which decreases the maximal rate of depolarization of phase 0 of the action potential.
-
Combines with fast sodium channels in their inactive state and inhibits recovery after repolarization in a time- and voltage-dependent manner, which is associated with subsequent dissociation of the drug from the sodium channels.
-
Exhibits electrophysiologic effects characteristic of class Ic antiarrhythmic agents, which slowly attach to and dissociate from transmembrane sodium channels.
-
Produces dose-related decrease in intracardiac conduction throughout the heart, with the most marked effect on conduction within the His-Purkinje system.
-
Produces dose-related increases in PR, QRS, and, to a lesser degree, QT intervals.
-
May increase atrial effective refractory period (ERP) and ventricular ERP.
-
Exhibits a mild to moderate negative inotropic effect.
Advice to Patients
-
Importance of not altering therapy without first consulting clinician.
-
Advise patients who self-administer loading dose for conversion of paroxysmal atrial fibrillation to remain in a supine or sitting position until resolution of palpitations or for a period of at least 4 hours following the dose. Importance of informing clinician if palpitations do not resolve within 6–8 hours, previously unexperienced symptoms (e.g., dyspnea, presyncope, syncope) occur, or a marked increase in heart rate develops.
-
Importance of informing clinicians of existing or contemplated concomitant therapy, including prescription and OTC drugs, as well as any concomitant illnesses.
-
Importance of women informing clinicians if they are or plan to become pregnant or to breast-feed.
-
Importance of advising patients of other important precautionary information. (See Cautions.)
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
* available from one or more manufacturer, distributor, and/or repackager by generic (nonproprietary) name
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
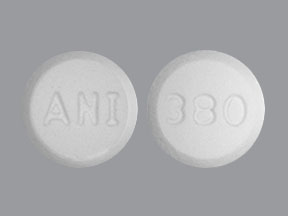
Oral |
Tablets |
50 mg* |
Flecainide Acetate Tablets |
|
|
100 mg* |
Flecainide Acetate Tablets |
|||
|
150 mg* |
Flecainide Acetate Tablets |
AHFS DI Essentials™. © Copyright 2024, Selected Revisions October 15, 2018. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
† Off-label: Use is not currently included in the labeling approved by the US Food and Drug Administration.
Reload page with references included
More about flecainide
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (173)
- Drug images
- Side effects
- Dosage information
- During pregnancy
- Support group
- Drug class: group I antiarrhythmics
- Breastfeeding
- En español