Spontaneous Pneumothorax in Children
Medically reviewed by Drugs.com. Last updated on Sep 23, 2025.
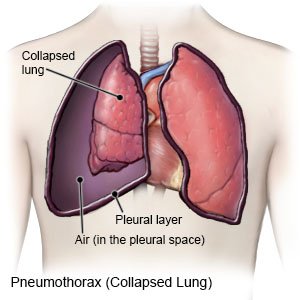
A spontaneous pneumothorax is a collapsed lung. Part or all of the lung may collapse. Air collects in the pleural space (the space between the lungs and chest wall). The trapped air prevents your child's lung from filling, and the lung collapses. A primary spontaneous pneumothorax occurs in a person with no known lung problems. A secondary spontaneous pneumothorax occurs in a person who has a known lung disease or medical condition. A spontaneous pneumothorax can happen in one or both lungs.
 |
WHILE YOU ARE HERE:
Informed consent
is a legal document that explains the tests, treatments, or procedures that your child may need. Informed consent means you understand what will be done and can make decisions about what you want. You give your permission when you sign the consent form. You can have someone sign this form for you if you are not able to sign it. You have the right to understand your child's medical care in words you know. Before you sign the consent form, understand the risks and benefits of what will be done to your child. Make sure all of your questions are answered.
A pulse oximeter
is a device that measures the amount of oxygen in your child's blood. A cord with a clip or sticky strip is placed on your child's foot, toe, hand, finger, or earlobe. The other end of the cord is hooked to a machine. Never turn the pulse oximeter or alarm off. An alarm will sound if your child's oxygen level is low or cannot be read.
Medicines:
- Antibiotics prevent or treat a bacterial infection.
- Pain medicine may be given.
Tests:
- Blood tests are used to check your child's oxygen and carbon dioxide levels. The results can tell healthcare providers how well your child's lungs are working.
- A heart monitor is used to record the electrical activity of your child's heart.
- X-ray pictures of the bones, lungs, and other tissues in your child's chest will show if he or she has broken ribs. The pictures may also show the size of the pneumothorax and if your child has fluid around his or her heart and lungs.
- CT scan or ultrasound pictures may be used to check for a pneumothorax that did not show up on x-rays. A CT may only be used if your child has Marfan syndrome. Your child may be given contrast liquid to help his or her lungs show up better in the pictures. Tell the healthcare provider if your child has had an allergic reaction to contrast liquid.
Treatment:
- Extra oxygen may be given if your child's oxygen level is too low. Oxygen may help the pneumothorax get better faster.
- Air removal may be done through a needle or a chest tube. A chest tube is attached to a container to remove air and collect any blood or fluid.
- Pleurodesis is a procedure used to irritate the walls of your child's pleural space. This causes the walls to close so air can no longer be trapped.
- Surgery may be used to repair your child's lung.
RISKS:
Air may continue to enter the pleural space and your child may get a tension pneumothorax. With a tension pneumothorax, the injured lung and trapped air push against your child's uninjured lung. A tension pneumothorax can lead to low blood pressure, decreased oxygen in his or her blood, and heart problems.
CARE AGREEMENT:
You have the right to help plan your child's care. Learn about your child's health condition and how it may be treated. Discuss treatment options with your child's healthcare providers to decide what care you want for your child.© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
