Lay Person CPR On Children
Medically reviewed by Drugs.com. Last updated on Aug 4, 2025.
What is lay person CPR on children?
Lay person cardiopulmonary resuscitation (CPR) is an emergency procedure for a child who is at least 1 year old. A lay person is someone who is not a trained healthcare worker. CPR may combine chest compressions with rescue breathing or may be chest compressions only. A chest compression means you put pressure on and off the child's chest. Rescue breathing means you give breaths to the child through his or her mouth.
What are some important things to remember about CPR for children?
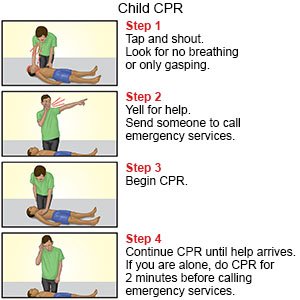
- Start CPR before you call or go for help if you are alone when you find the child. Do CPR for 2 minutes. Then call your local emergency number (911 in the US) to get emergency help as quickly as possible. If you are with another person, one person can start CPR and the other can call or go for help.
- Learn the steps used to give CPR to children by remembering C-A-B. This stands for chest C ompressions, A irway, and rescue B reathing.
- Do chest compressions even if you cannot give rescue breaths. Chest compressions alone make it more likely that the child will live than if you do nothing at all.
 |
What should I do if I find a child who is not breathing normally?
- Make sure the area is safe to enter, and approach the child. Tap the child's shoulder. Ask loudly, "Are you okay?" Move him or her if the area is dangerous, such as in a fire. You may also need to move the child if he or she is on a soft surface, such as a sofa or mattress. The child needs to be on a firm surface for chest compressions to be effective.
- Kneel beside the child. Look to see if his or her head, neck, or back may be hurt. Carefully turn the child onto his or her back while you support the head and neck. Keep the child's body straight as you turn him or her.
- Begin CPR if the child is not breathing or is only gasping. Do 30 compressions immediately. Then open the child's airway. Hold the airway open and give 2 rescue breaths. A cycle is 30 chest compressions and 2 rescue breaths.
- Call or go for help after 2 minutes of CPR.
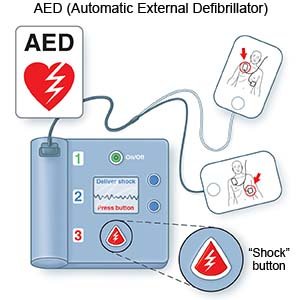
- Continue CPR cycles until the child responds, help arrives, or an automated external defibrillator (AED) becomes available. An AED is a device that gives a person's heart a shock if it is needed. AEDs are often kept in public areas and are usually mounted to a wall.
How do I give chest compressions?
Chest compressions press the heart between the spine and sternum (breastbone). This forces blood out of the heart and to the child's brain and body.
- Use one of the following methods, based on the child's size. Give chest compressions with one hand if the child is small. Use both hands if the child is large. For both positions, point your fingers up, and keep them off the child's chest. Compressions are done over the sternum. This is where the child's ribs meet in the middle of his or her chest. Do not lay your fingers on the chest, because you may do compressions in the wrong place. Incorrect hand positioning can break the ribs during compressions. Get up on your knees and position your body right over the child.
- One hand: Put the heel of your hand on the lower half of the child's sternum. Keep your other hand on the child's forehead. With the heel of your hand, press straight down on the child's chest 2 inches (5 centimeters). This should be at least ⅓ the depth of the child's chest. Keep your arm straight when you do chest compressions. Look down at your hand.
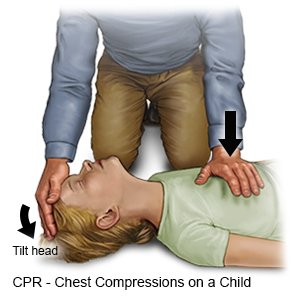
- Both hands: Put one of your hands on top of the other. Put the heel of your bottom hand on the lower half of the child's sternum. Press both hands straight down on the child's chest 2 inches (5 centimeters). This should be at least ⅓ the depth of the child's chest. Keep your arms straight when you do chest compressions. Look down at your hands.
- One hand: Put the heel of your hand on the lower half of the child's sternum. Keep your other hand on the child's forehead. With the heel of your hand, press straight down on the child's chest 2 inches (5 centimeters). This should be at least ⅓ the depth of the child's chest. Keep your arm straight when you do chest compressions. Look down at your hand.
- Do not push your hands forward when you press down. Go only up and down. The compressions should be constant and equal. This means that it should take the same amount of time to press down as it does to go back up. Allow the chest to relax completely between compressions. This allows blood to come back into the heart before you compress again. Leave your hands on the child's chest in the correct hand position between compressions.
- Do 30 chest compressions at a rate of at least 100 to 120 every minute. Push hard and push fast. Hard, fast compressions are more likely to keep the child's brain and heart alive. Count the compressions out loud to help you do them at a steady, even speed.
How do I open the child's airway?
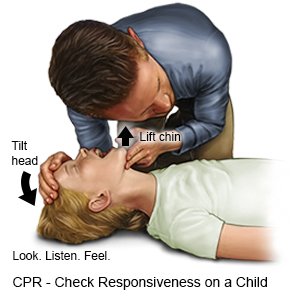
- Put 1 hand on the child's forehead and press firmly backward to tilt his or her head back. Do not place your hand on the back of his or her neck to tilt the head.
- Lift the child's chin with your other hand. Hold his or her mouth open. Do not press deeply into the soft tissue under his or her chin, because this can close the airway.
- Look into the child's mouth for something that may be blocking his or her airway. Examples are food and small toys. If you see something that looks easy to get, carefully scoop it out with your finger. Do not put your fingers in the back of the child's throat unless you see something to remove.
How do I give rescue breaths?
- Take a deep breath and put your lips around the child's mouth, nose, or both, making an airtight seal. If your mouth only covers the child's mouth, gently pinch the child's nose closed. This stops air from escaping through the nose.
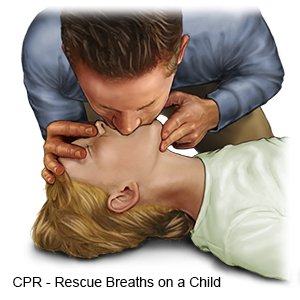
- Give 2 breaths (1 breath every 2 to 3 seconds) into the child's mouth. The child's chest will rise each time you give a rescue breath if his or her airway is open. Do not give large breaths. Do not breathe hard or fast. Take a normal breath for yourself after each breath that you give.
- Change the child's head position to reopen his or her airway, if needed. If you cannot get air in, the airway may be blocked by an object. Look again to see if you find an object you can remove.
What can I do to help prevent respiratory and cardiac arrest in children?
- Do not leave small objects within the reach of children. Children tend to put small objects into their mouths. Examples include batteries, coins, marbles, buttons, balloons, and small toys or toy parts. Do not allow your child to hold anything small enough to fit through a toilet paper roll. This includes foods such as hot dogs, grapes, nuts, popcorn, and hard candy.
- Do not leave plastic bags within a child's reach. Children may put plastic bags over their heads.
- Keep drapery and extension cords out of the reach of children. Do not put any type of cord or string around a child's neck. Some examples are cords or strings with pacifiers or jewelry attached to them.
- Do not leave your child alone in or near water. This includes a pool, bathtub, or pail of water.
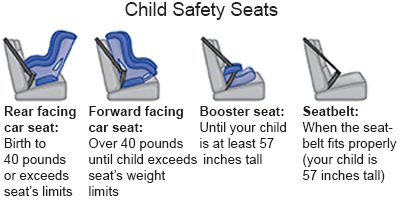
- Keep children secured in a car safety seat while you are driving. Never leave children in a car alone.
- Do not leave a child alone on a high surface, such as a changing table. Use toddler gates at the top of stairs. Stand near your child when he or she climbs on high playground equipment.
- Keep cleaning supplies and other harmful products out of children's reach and locked up tightly.

Where can I find more information about CPR?
- American Heart Association
7272 Greenville Avenue
Dallas , TX 75231-4596
Phone: 1- 800 - 242-8721
Web Address: http://www.heart.org
Care Agreement
You have the right to help plan your child's care. Learn about your child's health condition and how it may be treated. Discuss treatment options with your child's healthcare providers to decide what care you want for your child. The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
Learn more about Lay Person CPR On Children
Care guides
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
