Laparoscopic Hiatal Hernia Repair
Medically reviewed by Drugs.com. Last updated on Aug 4, 2025.
What do I need to know about laparoscopic hiatal hernia repair?
Laparoscopic hernia repair is surgery to repair a hiatal hernia.
 |
How do I prepare for laparoscopic hiatal hernia repair?
- Your surgeon will talk to you about how to prepare for surgery. You may be told not to eat or drink anything after midnight on the day of your surgery. Arrange to have someone drive you home when you are discharged.
- Tell your surgeon about all your current medicines. Your surgeon will tell you if you need to stop any medicine for surgery, and when to stop. You surgeon will tell you which medicines to take or not take on the day of your surgery.
- Tell your surgeon about any allergies you have, including to anesthesia or medicines. You may be given an antibiotic to help prevent a bacterial infection.
- Your surgeon will tell you if you need any tests before your surgery, and when to have them.
What will happen during laparoscopic hiatal hernia repair?
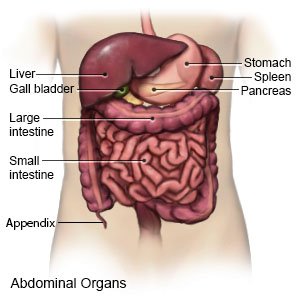
- You will be given general anesthesia to keep you asleep and free from pain during surgery. Your surgeon will make a small incision above your bellybutton. Your surgeon will insert a laparoscope through this incision. A laparoscope is a long metal tube with a light and camera on the end. Your surgeon will insert other instruments by making 2 to 4 smaller incisions at different places on your abdomen. Tools are used to remove the sac that contains your herniated stomach.

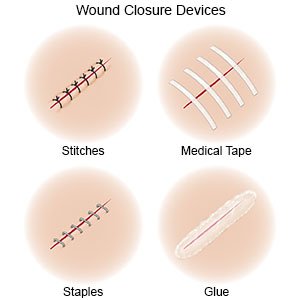
- Your stomach will then be placed back into its normal position. Stitches or mesh may be placed to close or decrease the size of your enlarged hiatus (opening in the diaphragm). Your healthcare provider may wrap a portion of your stomach around the esophagus. Your stomach will then be stitched and attached to the abdominal wall. The incisions will be closed with stitches or steristrips and covered with bandages.
What should I expect after laparoscopic hiatal hernia repair?
- You will need to do deep breathing exercises after your surgery to decrease your risk for a lung infection. Deep breaths help open your airway. These exercises will be painful because they put pressure on your incisions. You will be shown how to hold a pillow while you do breathing exercises to help decrease pain.
- You may need to have only soft foods for up to 4 weeks after your surgery.
- Do not drive for a week after your surgery. Do not lift heavy objects. Your healthcare provider will tell you when you can return to your daily activities.
What are the risks of laparoscopic hiatal hernia repair?
Your esophagus, stomach, blood vessels, or nerves may get injured during the surgery. You may bleed more than expected or get an infection. Problems may happen during your laparoscopic repair that may lead to a laparotomy (open surgery). You may develop another hernia even after you have this surgery. You may also have trouble swallowing and gastroesophageal reflux disease (GERD). You may get a blood clot in your leg or arm. This may become life-threatening.
Care Agreement
You have the right to help plan your care. Learn about your health condition and how it may be treated. Discuss treatment options with your healthcare providers to decide what care you want to receive. You always have the right to refuse treatment. The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
