Hypoglycemia in Adolescents with Diabetes
Medically reviewed by Drugs.com. Last updated on Sep 23, 2025.
What is hypoglycemia?
Hypoglycemia is a serious condition that happens when your blood glucose (sugar) level drops too low. The blood sugar level is usually too high in a person with diabetes, but the level can also drop too low. It is important to follow your diabetes management plan to keep your blood sugar level steady.
What increases my risk for hypoglycemia?
- A missed meal, or a meal eaten later than usual
- Vomiting
- Certain medicines, or too much insulin or other diabetes medicine
- More exercise than usual, without extra food
- Pregnancy
- Decreased liver or kidney function
- Alcohol use
What are the signs and symptoms I need to watch for?
- Headache, hunger, or being nervous
- Trouble thinking, or being moody
- Sweating, or a pounding heartbeat
- Being forgetful or confused, or double vision
- Feeling weak, or trouble walking
- Numbness and tingling around your mouth
- Seizures or loss of consciousness
How do I check my blood sugar level?
You will be given information on when and how to check your blood sugar level. Make a list of the times you checked your blood sugar level and the results of your checks. Take the list to all follow-up appointments.
- A glucose meter is a device that uses a test strip to check your blood sugar level. You put a small drop of blood from a finger on the test strip. The strip is put into the device. The device then figures out how much sugar is in your blood.

- A continuous glucose monitor (CGM) uses a sensor to check your blood sugar level. The sensor is placed on your abdomen or arm. A transmitter on the sensor gets a glucose reading. CGM data may be linked to an insulin pump. A CGM may be recommended if you are at increased risk for low blood sugar.

How do I manage hypoglycemia?
Always carefully follow your healthcare provider's instructions on how to treat low blood sugar levels. The following are general guidelines:
- Check your blood sugar level right away if you have symptoms. Hypoglycemia is usually 70 mg/dL or below. Ask your diabetes care team provider what blood sugar level is too low for you.
- If your blood sugar level is too low, eat or drink 15 grams of fast-acting carbohydrate. Examples are 4 ounces (½ cup) of fruit juice or regular soft drink, or 2 tablespoons of raisins. You may instead use 1 tube of glucose gel. Check your blood sugar level 15 minutes later. Sit still as you wait. If the level is still low (less than 100 mg/dL), have another 15 grams of carbohydrate. When the level returns to 100 mg/dL, eat a meal if it is time. If your meal time is more than 1 hour away, eat a snack. This will help prevent another drop in blood sugar. The snack should contain carbohydrates, such as the following:
- ¾ cup of cereal
- 1 cup of skim or low fat milk
- 6 soda crackers
- ½ of a turkey sandwich
- 15 fat-free chips
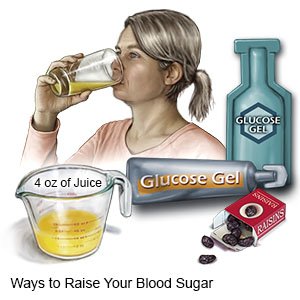
- Always carry a source of fast-acting carbs. If you have symptoms and you do not have a blood glucose meter, have a source of fast-acting carbs anyway. Avoid foods that are high in fat. The fat content may make the carbs take longer to increase your blood sugar level. Ask your provider if you should carry a glucagon kit. Glucagon is a medicine given as a shot when you develop severe signs or symptoms and become unconscious. Check the expiration date every month and replace it before it expires.
- Teach others how to help you if you have signs of low blood sugar. Tell them the signs to watch for. Ask them to give you a source of fast-acting carbs if you cannot get it yourself. Ask them to give you a glucagon shot if you have signs and you become unconscious or have a seizure. Ask them to call the local emergency number (911 in the US) . This is an emergency. Tell them never to try to make you swallow anything if you faint or have a seizure. Ask for support with your diabetes care at school, if needed.
- Wear medical alert jewelry or carry a card that says you have diabetes. Ask where to get these items.

How do I prevent hypoglycemia?
- Check your blood sugar level as directed. You may need to check the level at least 3 times each day. Ask when and how often to check. Ask your healthcare provider what your blood sugar levels should be before and after you eat. Record your blood sugar level results and take the record with you when you see your care team. They may use it to make changes to your medicine, food, or exercise schedules.
- Take diabetes medicine as directed. Do not double the amount of medicine you take unless instructed by your diabetes care team provider. You may need non-insulin diabetes medicine, insulin, or both to help control your blood sugar levels. Insulin may be given through a pump or pen, or injected. You and your care team will discuss the best method for you:
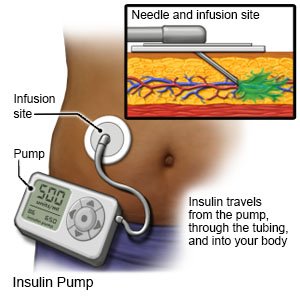
- An insulin pump is a wearable medical device that gives continuous insulin. An insulin pump prevents the need for multiple insulin injections in a day.
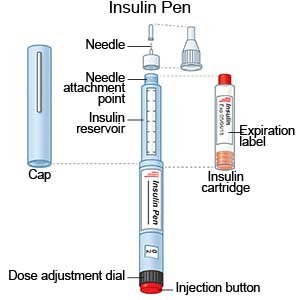
- An insulin pen is a device prefilled with insulin. Most insulin pens are disposable. You throw the pen away after it is empty or used for a certain amount of time. Some pens have a replaceable cartridge filled with insulin. You keep the pen and only throw away the cartridge.
- Insulin injections are given with a needle and syringe. You and your family members will be taught how to draw up and give insulin if this is the best method for you. You will also be taught how to dispose of used needles and syringes.
- An insulin pump is a wearable medical device that gives continuous insulin. An insulin pump prevents the need for multiple insulin injections in a day.
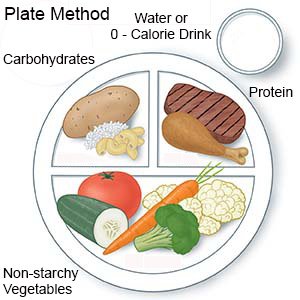
- Eat meals and snacks as directed. Talk to your dietitian or provider about a meal plan that is right for you. Do not skip meals.
- Check your blood sugar level before you exercise. Physical activity, such as exercise, can decrease your blood sugar level. If your blood sugar level is less than 100 mg/dL, have a carbohydrate snack. Examples are 4 to 6 crackers, ½ banana, 8 ounces (1 cup) of nonfat or 1% milk, or 4 ounces (½ cup) of juice. If you will be active for more than 1 hour, you may need to check your blood sugar level every 30 minutes. Your provider may also recommend that you check your blood sugar level after your activity.
Call your local emergency number (911 in the US), or have someone call, if:
- You have a seizure or pass out.
- Your blood sugar is less than 50 mg/dL and does not respond to treatment.
- You feel you are going to pass out.
- You have trouble thinking clearly.
When should I call my doctor or diabetes care team provider?
- You have had symptoms of low blood sugar several times.
- You are very worried or fearful about developing low blood sugar.
- You have questions about the amount of insulin or diabetes medicine you are taking.
- You have questions or concerns about your condition or care.
Care Agreement
You have the right to help plan your care. Learn about your health condition and how it may be treated. Discuss treatment options with your healthcare providers to decide what care you want to receive. You always have the right to refuse treatment. The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
