How to Recover From Covid-19 at Home
Medically reviewed by Drugs.com. Last updated on Aug 4, 2025.
AMBULATORY CARE:
What you need to know about recovering from COVID-19 at home:
COVID-19 can cause a range of symptoms, from mild to severe. If you do not need to be treated in a hospital, you will be given instructions to use at home. You will need to watch for worsening symptoms and seek immediate care if needed. You will also need to avoid spreading the virus to anyone.
Call your local emergency number (911 in the US) or an emergency department if:
- You have trouble breathing or shortness of breath at rest.
- You have chest pain or pressure that lasts longer than 5 minutes.
- You become confused or hard to wake.
Seek care immediately if:
- The skin on your face, fingers, or toes look blue or darker than usual.
Call your doctor if:
- You have a fever.
- You have new, returning, or worsening symptoms.
- Someone in your home has symptoms of COVID-19.
- You have questions or concerns about your condition or care.
Self-care:
Mild symptoms may get better on their own. The following may be used to manage your symptoms:
- Decongestants help reduce nasal congestion and help you breathe more easily. If you take decongestant pills, they may make you feel restless or cause problems with your sleep. Do not use decongestant sprays for more than a few days.
- Cough suppressants help reduce coughing. Ask your provider which type of cough medicine is best for you.
- To soothe a sore throat, gargle with warm salt water, or use throat lozenges or a throat spray. Drink more liquids to thin and loosen mucus and to prevent dehydration. Use decongestants or saline drops as directed for nasal congestion.
- NSAIDs , such as ibuprofen, help decrease swelling, pain, and fever. NSAIDs can cause stomach bleeding or kidney problems in certain people. If you take blood thinner medicine, always ask your healthcare provider if NSAIDs are safe for you. Always read the medicine label and follow directions.
- Acetaminophen decreases pain and fever. It is available without a doctor's order. Ask how much to take and how often to take it. Follow directions. Read the labels of all other medicines you are using to see if they also contain acetaminophen, or ask your doctor or pharmacist. Acetaminophen can cause liver damage if not taken correctly.
- Antiviral medicines may be given if you are at risk for developing severe or life-threatening symptoms.
Keep others safe while you are recovering at home:
Healthcare providers will give you specific instructions to follow. The following are general guidelines to remind you how to keep others safe until you are well:
- Wash your hands often. Use soap and water as much as possible. You can use hand sanitizer that contains alcohol if soap and water are not available. Do not share towels with anyone. If you use paper towels, throw them away in a lined trash can kept in your room or area. Use a covered trash can, if possible.

- Cover sneezes and coughs. Turn your face away and cover your mouth and nose with a tissue. Throw the tissue away. Use the bend of your arm if a tissue is not available. Then wash your hands well with soap and water or use hand sanitizer.
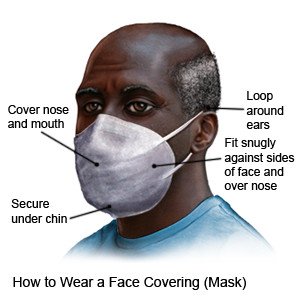
- Wear a face covering (mask) around others. Use a cloth covering with at least 2 layers. You can also create layers by putting a cloth covering over a disposable non-medical mask. Cover your mouth and your nose. The covering should fit snugly against the bridge of your nose. Securely fasten it under your chin and on the sides of your face.
- Do not go out of your home unless it is necessary. If possible, ask someone who is not infected to go out for groceries, medicines, and household items. Ask your provider for other ways to have appointments. Some providers offer phone, video, or other types of appointments. If you need to be seen in person, call ahead to make sure the office will be ready for you.
- Talk to your provider about your baby. If possible, ask someone who is well to care for your baby. You can put breast milk in bottles for the person to use, if needed. Wear a clean face covering if you need to breastfeed or express or pump breast milk. Tell your provider if you have any questions or concerns about caring for or bonding with your baby. Your provider will tell you when to bring your baby in for check-ups and vaccines. Your provider will also tell you what to do if you think your baby was infected with the coronavirus.
- Follow directions from your provider for when you can be around others. Your provider will give you specific instructions. In general, you will need to wait until your symptoms are gone. You will also need to have no fever for 24 hours without fever medicine. Do not travel until your provider says it is okay.
 |
Follow up with your doctor as directed:
Write down your questions so you remember to ask them during your visits.
For more information:
- Centers for Disease Control and Prevention
1600 Clifton Road
Atlanta , GA 30333
Phone: 1- 800 - 232-4636
Web Address: http://www.cdc.gov
© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
