Decision Aid for Clinically Localized Prostate Cancer
Medically reviewed by Drugs.com. Last updated on Aug 4, 2025.
What do I need to know about decisions for clinically localized prostate cancer?
Screening is a test done to find prostate cancer early. Screening is different from diagnosis because screening is used before you first start to have signs or symptoms. This means management or treatment can start early. Your healthcare provider may send you to other prostate cancer specialists such as a urologist or radiation oncologist. These providers can help you make informed decisions.
What do I need to know about clinically localized prostate cancer?
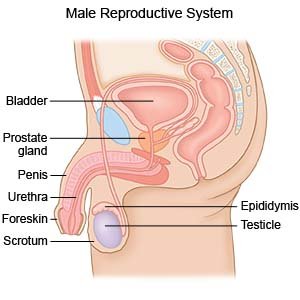
- The prostate is a small gland that is part of the reproductive system. It sits around your urethra (tube that carries urine out of your bladder). Cancer cells start to grow inside the prostate gland. The cells form a mass that continues to grow if left untreated. Clinically localized means that the cancer has not moved beyond the prostate gland.
- Prostate cancer is the second most common form of cancer in men (skin cancer is most common). About 17% of men in the US develop prostate cancer. About 3% of men in the US die from prostate cancer.
- Prostate cancer often grows slowly. Sometimes the tumor does not grow at all. The cancer may not grow quickly enough to be life-threatening in your lifetime.
- The risk for prostate cancer increases with age. Your risk is highest if you are older than 65 years. Your risk is lowest if you are younger than 45 years. Your risk is also increased if your father, brother, or son had prostate cancer.
- You may have no signs or symptoms of prostate cancer until the tumor grows large. You may have trouble urinating or keeping a strong urine stream because of the tumor. At later stages, prostate cancer can spread to your bones or lymph nodes. You may have bone pain or fractures.
Am I a good candidate for prostate cancer screening?
Screening may be helpful for you if any of the following is true:
- You are 45 to 69 years old.
- You have not had prostate cancer.
- You have a family history of prostate cancer or other prostate problems.
- You do not have signs or symptoms of prostate cancer.
- You do not have another health condition that may prevent you from living longer than another 10 years.
- You want to have treatment as early as possible if needed.
- You are willing to have screening as often as recommended by your healthcare provider.
How is screening done?
- A digital rectal exam (DRE) is used to check your prostate. Your healthcare provider will insert a gloved finger into your rectum. The provider will be able to feel your prostate for lumps or hard areas that could be tumors. The DRE may be repeated over time to check for new or worsening problems.
- A prostate-specific antigen (PSA) test is used to measure the amount of a protein made by your prostate gland. A blood sample is taken for this test. A high PSA level may be a sign of prostate cancer.
- A prostate cancer gene 3 (PCA3) test is used if your PSA level is high but a biopsy does not show prostate cancer. Your urine is tested after a DRE to find the amount of PCA3 it contains. Another biopsy may be recommended if your PCA3 level is higher than normal.
What are the benefits and risks of screening?
Talk with your healthcare provider about the risks and benefits of screening:
- Benefits include the following:
- Screening may show you do not have prostate cancer. This can help lower anxiety if you have risk factors for prostate cancer. You will still need to have screening as directed. You may develop prostate cancer later on.
- Prostate cancer that is found may be at an early stage. Cancer treatment is often more successful when it starts early. This means you can make more decisions about treatment.
- Risks include the following:
- You may have a false belief that you will not develop prostate cancer if your screening result is negative. You can still develop prostate cancer later on.
- If you do develop prostate cancer, treatment may cause new health problems. The treatment may not have been needed. Prostate cancer may grow so slowly that it would not have become life-threatening in your lifetime. Prostate cancer does not always cause signs or symptoms that need to be treated.
- A PSA test can give a false-negative result. This means the result looks like you do not have cancer even though you do. Treatment or monitoring may be delayed because the tests suggested you do not have cancer.
- The PSA test can also give a false-positive result. This means you do not actually have cancer but the test shows you do. You may get more tests, a biopsy, or even treatments that are not needed. It can also be stressful to think you have prostate cancer when you do not.
What questions should I ask my healthcare provider to help me make decisions about screening?
- How high is my risk for prostate cancer?
- How often do I need to have screening?
- Where is the screening done?
- Do I need to do anything to get ready to have screening?
What happens after I have screening?
- You will meet with your healthcare provider to go over the results of your screening.
- You may need more tests to diagnose anything that showed up on the screening test. Only a biopsy (tissue sample) can show for sure that you have prostate cancer.
- After cancer is found, your healthcare provider will assign a number called a Gleason score. The number can help you understand how quickly the cancer is likely to grow, and if it may spread:
- A number of 6 or lower means the cancer is likely to grow more slowly.
- A score of 7 means it is likely to grow faster, but it may not spread to other areas.
- A score of 8 to 10 means it is likely to grow more quickly and also spread.
- Your healthcare provider will also assign a T stage to the tumor. This number shows the growth of the tumor and if it is likely to spread to other areas.
- You and your healthcare provider will use the Gleason score, T stage, and PSA results to talk about your treatment options. Your provider will tell you if your prostate cancer is at low, medium, or high risk for growing and spreading. The need for more tests and the range of treatment options depend on the risk level. Together you and your provider can create a treatment plan that is right for you.
How is clinically localized prostate cancer treated, and what are the benefits of treatment?
- Watchful waiting means you do not receive treatment right away. If the cancer does not grow or spread, you may never need treatment. Watchful waiting may be used if your tumor risk is low. The benefit of this option is that you will not have invasive or difficult treatment. You can choose a different treatment option if tests show the tumor is growing or spreading over time.
- Active surveillance also means you do not receive treatment right away. You will need to have tests over time to continue to check the tumor. A benefit of this option is that follow-up tests can show a change early. Treatment options may be less invasive than if the tumor is found at a later stage.
- Cryoablation is used to kill cancer cells by freezing them. This is a less invasive treatment. You may have little or no pain after this procedure.
- Radiation may be used to destroy the cancer cells. Radiation is about as effective as surgery to remove the prostate gland. This treatment leaves the prostate in place and only targets the cancer cells.
- Surgery is used to remove the prostate gland. The tumor is in the gland, so it will be removed along with the gland.
- Hormone therapy may be added to surgery or radiation treatment. Your testosterone level is lowered, or it is blocked. This can stop the cancer cells from growing, or slow the growth. Hormone therapy may be given as an injection every 1 to 6 months. Another way to lower your testosterone level is to have surgery to remove your testicles. Your body will no longer make testosterone if your testicles are removed.
What are the risks of treatment?
- Watchful waiting and active surveillance can cause you to worry that the cancer is growing or spreading.
- Surgery can damage tissue around your prostate. Surgery can increase your risk for trouble urinating, incontinence (leaking), or urinary retention. Surgery can also cause problems with your ability to have or keep an erection. You may bleed more than expected during surgery or develop an infection. You may also need to be treated again if the surgery you have does not relieve your symptoms. Surgery may not be able to remove all the tumor cells.
- Radiation may not kill all the cancer cells. Radiation can cause urinary problems such as pain, retention, loss of control, or leakage. Your skin can become dry or irritated. You may develop problems with having bowel movements, such as pain, diarrhea, or constipation. Radiation can also cause problems with your ability to have or keep an erection.
- Cryoablation may not kill all the cancer cells. You may develop scar tissue. You can also have swelling, problems urinating, or pain in your pelvis or scrotum. Tissue outside the prostate may be damaged during cryoablation. You may have permanent erection problems.
What questions should I ask my healthcare provider to help me make decisions about treatment?
- What is my Gleason score, T score, and risk number?
- How often will I need follow-up tests if I choose active surveillance first?
- How will each treatment option affect my daily activities?
- What is the risk for erectile dysfunction or impotence with each treatment?
- Am I a good candidate for surgery?
- Which surgery may work best to treat my symptoms?
- Where is the surgery done?
- How long is recovery after surgery?
- Will my insurance cover treatment?
What do I need to think about to help me make decisions about treatment?
- If my cancer risk is low, will I be comfortable with watchful waiting or active surveillance instead of immediate treatment? How will I feel if the cancer grows or spreads?
- Will I go in for follow-up tests over time if I do not want treatment right away?
- If I have treatment and lose my ability to have an erection, how will I feel?
- Am I willing to accept problems with urinating or having a bowel movement that might happen with treatment?
- How will my family or others in my life be affected by my treatment decisions?
Care Agreement
You have the right to help plan your care. Learn about your health condition and how it may be treated. Discuss treatment options with your healthcare providers to decide what care you want to receive. You always have the right to refuse treatment. The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
