Aortic Disease
Medically reviewed by Drugs.com. Last updated on Sep 23, 2025.
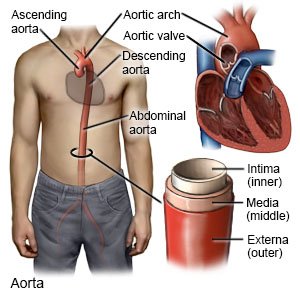
Aortic disease is a general term to describe conditions that affect the aorta or the aortic valve. The aorta is a large blood vessel that goes from your heart down into your abdomen. The valve opens to let blood go from your heart into your aorta. The valve then closes to prevent blood from flowing back into your heart. An aortic disease develops because the aorta or its valve is weakened, damaged, or not formed correctly. The main aortic diseases are aneurysms and dissections. An aneurysm is a bulge that may rupture (burst). A dissection is a tear that happens suddenly. A rupture or tear is a life-threatening emergency.
 |
DISCHARGE INSTRUCTIONS:
Call your local emergency number (911 in the US) or have someone call if:
- You have any of the following signs of a heart attack:
- Squeezing, pressure, or pain in your chest
- You may also have any of the following:
- Discomfort or pain in your back, neck, jaw, stomach, or arm
- Shortness of breath
- Nausea or vomiting
- Lightheadedness or a sudden cold sweat
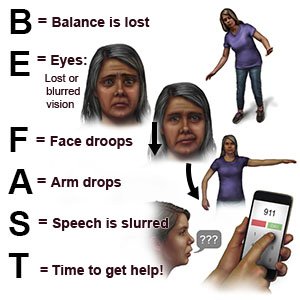
- You have any of the following signs of a stroke:
- Numbness or drooping on one side of your face
- Weakness in an arm or leg
- Confusion or difficulty speaking
- Dizziness, a severe headache, or vision loss
- You have sudden sharp pain in your back, abdomen, or groin.
- You cough or vomit up blood.
- You cannot feel anything from your waist to your toes.
- You have trouble breathing or shortness of breath.
- You feel dizzy, faint, or you lose consciousness.
Seek care immediately if:
- You have a fever.
- You have a pulsating lump or swelling in your abdomen.
- You have trouble swallowing.
- You have blood in your urine.
- You are urinating very little or not at all.
- You have at least 1 toe that looks blue or darker than usual.
- You have a foot that changes color and becomes cold to the touch.
- Your skin is pale, sweaty, or clammy.
Call your doctor if:
- You want to start family planning.
- You feel anxious or depressed about your condition.
- You have questions or concerns about your condition or care.
Medicines:
You may need any of the following:
- Blood pressure medicine may be needed to lower your blood pressure. This can help prevent a heart attack and your aortic disease getting worse.
- Cholesterol medicine may be needed to lower your cholesterol level and prevent atherosclerosis of your aorta. This can help prevent a heart attack or stroke.
- Antiplatelets , such as aspirin, help prevent blood clots. Take your antiplatelet medicine exactly as directed. These medicines make it more likely for you to bleed or bruise. If you are told to take aspirin, do not take acetaminophen or ibuprofen instead.
- Take your medicine as directed. Contact your healthcare provider if you think your medicine is not helping or if you have side effects. Tell your provider if you are allergic to any medicine. Keep a list of the medicines, vitamins, and herbs you take. Include the amounts, and when and why you take them. Bring the list or the pill bottles to follow-up visits. Carry your medicine list with you in case of an emergency.
Manage your aortic disease:
Your healthcare provider may recommend cardiac rehabilitation (rehab). Cardiac rehab is a program run by a team of specialists who will help you create a management plan. Your plan may include these or other guidelines:
- Manage other health conditions that increase the risk for new or worsening aortic disease. Examples are extra body weight, stress, and high BP. Ask your provider what a healthy weight is for you. Your provider can help you create a weight loss plan, if needed. Manage stress by learning new ways to relax, such as listening to music. Check your BP as directed if you have high BP. Your provider will show you how to do this. Check your BP 2 times, 1 minute apart. Check as often as directed each day. Keep a record of your readings and bring it to your follow-up visits.

- Do not use tobacco products or stimulating drugs. Nicotine and drugs such as cocaine increase your risk for a tear, rupture, or other problem in your aorta. Ask your provider for information if you currently use tobacco products or stimulating drugs and need help to quit. E-cigarettes or smokeless tobacco still contain nicotine. Do not use these in place of cigarettes. Avoid secondhand smoke.
- Know the risks if you choose to drink alcohol. Alcohol can increase your BP. Ask your healthcare provider if it is okay for you to drink any alcohol. Your provider can help you set limits for the number of drinks you have within 24 hours and within 1 week. A drink of alcohol is 12 ounces of beer, 5 ounces of wine, or 1½ ounces of liquor.
- Follow physical activity directions. Your physical activity plan may include low-intensity activity, such as walking, yoga, or swimming. You may need to avoid intense physical activity, such as weightlifting or running. Intense activity may raise your BP or put pressure on your aorta. These increase your risk for a tear or rupture. You may also need to avoid contact sports such as football to decrease your risk for a chest injury.
- Follow recommended meal plans. Talk to your provider or a dietitian about a heart-healthy or low-sodium meal plan. These meal plans may help you lower your cholesterol and BP levels, and reach or maintain a healthy weight. Heart-healthy meal plans are low in sodium, processed sugar, and some fats. They are high in potassium, calcium, heart-healthy fats, and fiber. These can be found in vegetables, fruit, and whole-grain foods.

- Get vaccines as directed. Some viruses can worsen aortic disease. Get an influenza (flu) vaccine as soon as recommended each year, usually in September or October. Get all recommended COVID-19 vaccine doses and boosters. A pneumonia vaccine may also be recommended. Your provider will tell you if you need other vaccines, and when to get them.
Talk to your specialist about family planning:
- Before you try to get pregnant, talk to your specialist about family planning. Genetic counseling may be needed if you have a condition that can pass on to your baby. You may need counseling if your condition can put you or your pregnancy at risk. You may instead need counseling about the risk of pregnancy making your aortic disease worse. You may also need scans of your aorta. These scans can help you and your provider plan treatment before and during your pregnancy. You may need surgery to protect your aorta and prevent a dissection or rupture.
- While you are pregnant, you may have 1 or more specialist caring for you. You may need medicine to help lower your blood pressure. You may need regular scans to check your aorta. You may need other medicines or surgery if your aorta dissects or ruptures. A cesarean section (C-section) may be needed if you have a history of aortic dissection. You may need a C-section if you have a high risk for an aortic dissection or rupture.
- After your baby is born, you may need scans to check your aorta. Your risk for an aortic dissection or rupture is high for up to 12 weeks.
Follow up with your doctor or specialist as directed:
You may need to return for regular scans to check your aorta for changes. These scans will help your provider monitor your aortic disease. You may need an endovascular procedure or surgery to repair your aorta. You will also need scans after an aorta repair. Your doctor or specialist will tell you how often to have the scans. Write down your questions so you remember to ask them during your visits.
© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
