Achilles Tendon Lengthening
Medically reviewed by Drugs.com. Last updated on Sep 23, 2025.
AMBULATORY CARE:
Achilles tendon lengthening
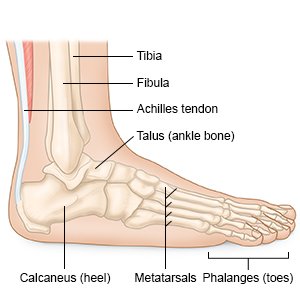
is surgery to stretch the Achilles tendon so you can point your foot up. The Achilles tendon connects your calf muscle to your heel bone. If the tendon becomes too tight, you will only be able to point your foot down. This means you cannot put your heel down when you walk. You may walk on your toes or put your weight on the front of your foot. Pressure injuries can develop, especially if you have diabetes. Surgery allows your ankle to move freely so you can walk with your foot flat on the floor.
 |
How to prepare for surgery:
- Your surgeon will tell you how to prepare. He or she may tell you not to eat or drink anything after midnight on the day of surgery. Arrange to have someone drive you home when you are discharged from the hospital.
- Tell your surgeon about all medicines you currently take. He or she will tell you if you need to stop any medicine for surgery, and when to stop. He or she will tell you which medicines to take or not take on the day of surgery.
What will happen during surgery:
Your surgeon may do surgery through one or more small incisions into your skin. This type of surgery allows your body to try to lengthen the tendon as it heals. He or she may instead do open surgery. Open surgery is the most common surgery. Your surgeon will make one large incision for open surgery to see all or some of the tendon. Your surgeon will talk to you about which kind of surgery is right for you.
- General anesthesia may be given to keep you asleep and free from pain during surgery. Regional anesthesia may instead be given to numb the surgery area. Your surgeon will make one or more incisions. He or she will then make cuts in the tendon so it can be stretched. The cuts may be along the tendon, or only at one or both ends.
- Your foot movement will be checked to make sure the foot moves properly. Your surgeon may make a few adjustments if the movement is still limited. Your foot will then be held in the correct position. If you have open surgery, the tendon will be sewn back together after it is stretched.
- The incision or incisions will be closed with stitches or staples. A splint, cast, or walking boot will be used to keep your foot in the correct position while the tendon heals.
What to expect after surgery:
- You will wear a splint, cast, or walking boot for 6 to 8 weeks to keep your foot from moving.
- You will be given instructions for activities to avoid for 6 to 8 weeks after surgery. The instructions will include when it is okay to put weight on your foot.
- Physical therapy may be started after the splint, cast, or boot is removed. A physical therapist can help you strengthen your ankle and improve mobility and flexibility.
Risks of Achilles tendon lengthening:
The entire tendon may be cut instead of small portions. Damage to tissues and other areas near the tendon can keep blood from flowing to the tendon. Healing can take longer if this happens. The tendon length can also become too long. This may cause you to walk with more weight on your heel. Pressure injuries can form on the heel over time. The tendon may still be tight after surgery. The tendon can also tear during or after surgery. You may need surgery to repair the torn tendon.
Seek care immediately if:
- You have a splint or cast and it gets damaged, starts to feel tighter, or your skin turns blue or pale.
- You have severe pain that does not go away after you take pain medicine.
- Your leg feels warm, tender, and painful. It may look swollen and red.
- Blood soaks through your bandage.
- Your stitches come apart.
Call your doctor or surgeon if:
- You have a fever or chills.
- Your wound is red, swollen, or draining pus.
- Your skin is itchy, swollen, or you have a rash.
- You have questions or concerns about your condition or care.
Medicines:
You may need any of the following:
- NSAIDs , such as ibuprofen, help decrease swelling, pain, and fever. NSAIDs can cause stomach bleeding or kidney problems in certain people. If you take blood thinner medicine, always ask your healthcare provider if NSAIDs are safe for you. Always read the medicine label and follow directions.
- Prescription pain medicine may be given. Ask your healthcare provider how to take this medicine safely. Some prescription pain medicines contain acetaminophen. Do not take other medicines that contain acetaminophen without talking to your healthcare provider. Too much acetaminophen may cause liver damage. Prescription pain medicine may cause constipation. Ask your healthcare provider how to prevent or treat constipation.
- Antibiotics help prevent or treat a bacterial infection.
- Take your medicine as directed. Contact your healthcare provider if you think your medicine is not helping or if you have side effects. Tell your provider if you are allergic to any medicine. Keep a list of the medicines, vitamins, and herbs you take. Include the amounts, and when and why you take them. Bring the list or the pill bottles to follow-up visits. Carry your medicine list with you in case of an emergency.
Care for the surgery area:
- Do not swim, soak in a hot tub, or take a bath until your healthcare provider says it is okay. Your healthcare provider will tell you when it is okay to shower after surgery. You may need to cover the area with plastic bags to keep it dry.
- Care for your splint or cast as directed. Do not get your splint or cast wet. If your healthcare provider says you can shower, cover it with a plastic bag. Do not put pressure on it until your healthcare provider says it is okay. Do not put objects under your splint or cast to scratch your skin. This may cause an infection. Check your skin around the splint or cast for redness, swelling, or open areas. Ask your healthcare provider for more information on how to care for your splint or cast.
- Wear a walking boot as directed if it was applied instead of a cast. A walking boot helps keep your foot stable so it can heal. It can keep your weight off your ankle as it heals. You may need to wear the boot for 6 to 8 weeks after surgery. Your healthcare provider will give you instructions for how long to wear it each day.

Self-care:
- Rest your leg as directed. Keep weight off of your leg as directed. You may need to wait at least 12 weeks before you can play sports. Ask your healthcare provider when you can return to your normal activities.
- Apply ice on your leg for 15 to 20 minutes every hour or as directed. Use an ice pack, or put crushed ice in a plastic bag. Cover it with a towel. Ice helps prevent tissue damage and decreases swelling and pain.
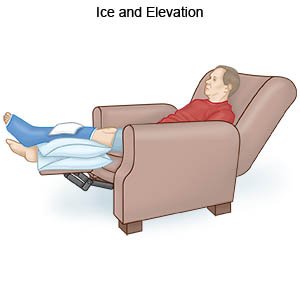
- Elevate your leg above the level of your heart as often as you can. This will help decrease swelling and pain. Prop your leg on pillows or blankets to keep it elevated comfortably.
- Keep pressure off your leg as directed. Use crutches or a cane as directed. Do not stand on your leg. This could cause your stitches to come apart. Ask your healthcare provider when you can put weight on your leg.
- Go to physical therapy as directed. A physical therapist teaches you exercises to help improve range of motion (ROM) and strength, and to decrease pain. He or she will teach you ROM exercises. ROM exercises are gentle movements of your joint. ROM exercises will prevent stiffness and help build strength. Do not do ROM exercises unless your healthcare provider says it is okay.
Follow up with your doctor or surgeon as directed:
Write down your questions so you remember to ask them during your visits.
© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
