Methotrexate (Monograph)
Brand names: Jylamvo, Otrexup, Rasuvo, Trexall Xatmep
Drug class: Antineoplastic Agents
Warning
- Serious Toxic Reactions
-
Deaths reported with use in treatment of malignancy, psoriasis, and rheumatoid arthritis.
-
Use only for treatment of life-threatening neoplastic diseases or severe, recalcitrant, disabling psoriasis or rheumatoid arthritis in patients who have not responded adequately to other forms of therapy.
-
Closely monitor patients for bone marrow, hepatic, pulmonary, or renal toxicities.
-
Inform patients of risks involved with therapy and importance of remaining under care of clinician throughout therapy.
- High-Dose Regimens
-
Use of high-dose regimens recommended for treatment of osteosarcoma requires meticulous care.
-
Use of high-dose regimens for other neoplastic diseases is investigational; therapeutic advantage not established.
- Formulations or Diluents Containing Benzyl Alcohol
-
Do not use formulations or diluents containing preservatives (benzyl alcohol) for intrathecal administration or high-dose therapy; also avoid use in neonates and low birth-weight infants.
- Fetal/Neonatal Morbidity and Mortality
-
Fetal death and/or congenital anomalies reported. Not recommended for use in women of childbearing potential unless potential benefit clearly outweighs risks; do not use in pregnant women with non-neoplastic disorders (e.g., psoriasis or rheumatoid arthritis).
- Renal Toxicity
-
Renal toxicity leading to irreversible acute renal failure has occurred.
- Hepatotoxicity
-
Possible hepatotoxicity, fibrosis, cirrhosis, and fatal liver failure generally only after prolonged use.
-
Acute liver enzyme elevations frequently observed; usually transient and asymptomatic and do not appear predictive of subsequent hepatic disease.
-
Liver biopsy after sustained use often shows histologic changes. Fibrosis and cirrhosis may not be preceded by symptoms or abnormal liver function tests in patients with psoriasis; periodic liver biopsies usually recommended in such patients undergoing long-term therapy.
-
Persistent abnormalities in liver function tests may precede appearance of fibrosis or cirrhosis in patients with rheumatoid arthritis.
- Neurotoxicity
-
Severe acute and chronic neurotoxicity, which can be progressive, irreversible, and fatal, reported.
-
Generalized and focal seizures have occurred in pediatric patients receiving methotrexate.
-
Intermediate- and high-dose IV, intrathecal, and low-dose regimens can cause leukoencephalopathy (risk heightened with prior cranial radiation).
-
High-dose therapy can cause transient, acute stroke-like syndrome; intrathecal administration can cause acute chemical arachnoiditis or subacute myelopathy.
- Pulmonary Toxicity
-
Potentially fatal pulmonary lesions, not always reversible, may occur acutely at any dosage level.
-
Pulmonary symptoms (especially dry, nonproductive cough) may require therapy interruption and careful evaluation.
- GI Toxicity
-
Diarrhea, vomiting, stomatitis, hemorrhagic enteritis, and fatal intestinal perforation may occur; withhold or discontinue therapy if severe GI toxicity occurs.
- Secondary Malignant Lymphomas
-
Malignant lymphomas may occur in patients receiving low-dose oral therapy; such lymphomas may regress following methotrexate discontinuance and may not require cytotoxic therapy. If the lymphoma does not regress following discontinuance, institute appropriate therapy.
- Tumor Lysis Syndrome
-
May induce tumor lysis syndrome in patients with rapidly growing tumors; appropriate pharmacologic and supportive treatment may prevent or alleviate syndrome.
- Hypersensitivity and Dermatologic Reactions
-
Hypersensitivity reactions, including anaphylaxis, reported.
-
Severe, occasionally fatal skin reactions following single or multiple doses; reactions occurred within days of oral, IM, IV, or intrathecal administration. Recovery reported with discontinuance of therapy.
- Myelosuppression
-
Severe and life-threatening cases of pancytopenia, anemia, aplastic anemia, leukopenia, neutropenia, and thrombocytopenia reported.
- Serious Infections
-
Life-threatening or fatal bacterial, fungal, or viral infections have occurred.
- Concomitant Radiotherapy
-
Possible increased risk of soft tissue necrosis and osteonecrosis in patients receiving methotrexate concomitantly with radiotherapy.
Introduction
Antineoplastic agent and immunosuppressant; folic acid antagonist.
Uses for Methotrexate
Trophoblastic Diseases
Methotrexate injection and powder for injection used as part of a combination chemotherapy regimen for treatment of trophoblastic diseases (choriocarcinoma, invasive mole [formerly known as chorioadenoma destruens], hydatidiform mole) in adults.
First-line therapy in patients with low-risk gestational trophoblastic neoplasms (i.e., invasive mole or choriocarcinoma histology with 1) International Federation of Gynecology and Obstetrics [FIGO] stage I disease [confined to the uterus] or 2) FIGO stage II or III disease [extending to genital structures outside the uterus or to the lungs, respectively] and WHO risk score <7 [indicating low likelihood of resistance to single-agent chemotherapy]).
In patients with high-risk trophoblastic neoplasms, methotrexate in combination with etoposide, dactinomycin, vincristine, and cyclophosphamide (EMA-CO) is a standard treatment option.
Leukemias
Used as a part of a combination chemotherapy maintenance regimen to treat acute lymphoblastic leukemia. Injection, powder for injection, oral solution (Jylamvo only), and oral tablets approved for this indication in adults and pediatric patients. Xatmep (methotrexate oral solution) approved for this indication in pediatric patients only; designated an orphan drug by the FDA for this indication in pediatric patients 0–16 years of age.
Injection and powder for injection also used for prophylaxis and treatment of meningeal leukemia in adults and pediatric patients.
Osteosarcoma
High-dose therapy with injection or powder for injection, followed by leucovorin or levoleucovorin rescue, is used in combination chemotherapy regimens as adjunct to surgical resection or amputation of primary tumor in patients with nonmetastatic osteosarcoma (designated an orphan drug by FDA for this use).
Breast Cancer
Injection and powder for injection used for treatment (alone or, more commonly, as part of a combination chemotherapy regimen) of breast cancer.
Used in combination with cyclophosphamide and fluorouracil (CMF) as an alternative option to doxorubicin-cyclophosphamide when an anthracycline-taxane combination is contraindicated.
Lymphoma
Used for treatment of various types of lymphoma. Injection, powder for injection, tablets, and oral solution (Jylamvo only) used for the treatment of non-Hodgkin lymphomas in adults; non-injectable formulations of methotrexate specify that it should be used as part of a metronomic combination regimen for this indication.
Methotrexate injection and powder for injection also approved for the treatment of non-Hodgkin lymphomas in pediatric patients. Methotrexate powder for injection, tablets, and oral solution (Jylamvo only) also used as a single agent or as part of a combination chemotherapy regimen to treat mycosis fungoides (cutaneous T-cell lymphoma) in adults.
Psoriasis
Treatment of severe psoriasis in carefully selected adult patients (all formulations except Xatmep oral solution); powder for injection and injection for sub-Q use (Rasuvo and Otrexup) used specifically for symptomatic control of severe, recalcitrant, disabling psoriasis that is not adequately responsive to other forms of therapy. Guidelines generally support use of methotrexate, administered orally or sub-Q, for treatment of moderate to severe psoriasis in adults.
Recommendations for use and selection of psoriasis therapies vary based on patient age, disease characteristics (e.g., severity, location, presence of psoriatic arthritis), and comorbidities (e.g., inflammatory bowel disease).
Rheumatoid Arth
All formulations except Xatmep oral solution used for management of rheumatoid arthritis in adults; powder for injection and injection for sub-Q use (Rasuvo and Otrexup) used specifically in adults with severe, active disease who are intolerant to or whose symptoms progress despite adequate first-line treatment.
Disease-modifying treatments for rheumatoid arthritis include conventional DMARDs (e.g., hydroxychloroquine, leflunomide, methotrexate, sulfasalazine), biologic DMARDs (e.g., TNF blocking agents, abatacept, tocilizumab, sarilumab, rituximab), and/or targeted synthetic DMARDs (e.g., Janus kinase inhibitors).
Guidelines generally support use of methotrexate monotherapy first-line in DMARD-naïve patients with moderate to high disease activity.
Specific agents for rheumatoid arthritis are selected according to current disease activity, prior therapies used, and presence of comorbidities. Individualized “treat-to-target” approach is typically employed, with the goal of achieving remission or minimal/low disease activity.
Polyarticular Juvenile Idiopathic Arthritis
Used for the management of polyarticular juvenile idiopathic arthritis in pediatric patients; powder for injection, injection for sub-Q use (Rasuvo and Otrexup), and oral solution (Xatmep only) specifically used in pediatric patients with severe, active disease who are intolerant to or whose symptoms progress despite adequate first-line treatment. Xatmep designated an orphan drug by FDA for this use in pediatric patients.
Drugs used to treat juvenile idiopathic arthritis include NSAIAs, systemic and intra-articular corticosteroids, conventional disease-modifying antirheumatic drugs (DMARDs; e.g., methotrexate, sulfasalazine, hydroxychloroquine, leflunomide), and biologic DMARDs (e.g., TNF blocking agents, abatacept, tocilizumab, rituximab).
Guidelines generally support use of methotrexate monotherapy for treatment of pediatric juvenile idiopathic arthritis and active polyarthritis.
Specific agents for juvenile idiopathic arthritis treatment are selected according to presence of certain risk factors (e.g., positive anti-cyclic citrullinated peptide antibodies, positive rheumatoid factor, joint damage), level of disease activity, involvement of specific joints, presence of certain comorbidities (e.g., uveitis), and prior therapies. Individualized “treat-to-target” approach is typically employed, with the goal of achieving remission or minimal/low disease activity.
Head and Neck Cancer
Injection and powder for injection used for palliative treatment (alone and as part of combination therapy) of recurrent or metastatic head and neck carcinoma.
Combination chemotherapy regimens associated with increased response rates but no survival advantage compared to methotrexate monotherapy.
Crohn's Disease
Induction and maintenance of remission in patients with moderate to severe Crohn's disease† [off-label] .
Other Uses
Used in combination regimens with vinblastine and cisplatin, with or without doxorubicin for invasive and advanced bladder cancer† [off-label] .
Used IM for treatment of tubal ectopic pregnancy† [off-label] in women with the following characteristics: high clinical suspicion or confirmation of ectopic pregnancy, hemodynamically stable, unruptured mass, no absolute contraindications to methotrexate.
Used for immunosuppressive and/or anti-inflammatory effects in the treatment of atopic dermatitis† [off-label] , psoriatic arthritis† [off-label] , systemic lupus erythematosus† , antineutrophil cytoplasmic antibody-associated vasculitides† , dermatomyositis† , polymyositis† , and a variety of dermatologic and chronic refractory ocular diseases† .
Has also been used for prophylaxis of acute graft-versus-host disease† following stem cell transplantation for hematologic malignancies.
Although labeled for use in squamous cell type of non-small cell lung cancer, other agents are preferred.
Methotrexate Dosage and Administration
General
Pretreatment Screening
-
Verify pregnancy status in patients of reproductive potential.
-
Assess complete blood count (CBC) with differential, platelet counts, liver function tests, and renal function tests.
-
Obtain a chest X-ray.
-
Monitor electrolytes at baseline in patients who will receive high-dose therapy.
-
Administer all appropriate vaccines according to immunization guidelines.
-
Evacuate any significant third space accumulations prior to initiating methotrexate.
Patient Monitoring
-
Monitor hematologic tests periodically (some manufacturers recommend at least once per month) during treatment.
-
Monitor renal and hepatic function every 1–2 months during treatment.
-
More frequent monitoring of these parameters may be necessary during treatment initiation, when changing doses, or during periods of increased risk of elevated methotrexate blood levels (e.g., dehydration).
-
Monitor for signs of infection and toxicity (including bone marrow, gastrointestinal, renal, hepatic, neurologic, pulmonary, and dermatologic toxicity) during treatment.
-
If a high-dose regimen is utilized, monitor serum creatinine, electrolytes, and methotrexate concentrations at least daily during therapy.
Premedication and Prophylaxis
-
To decrease the risk of severe adverse reactions, administer rescue therapy with leucovorin or levoleucovorin in patients receiving high-dose (i.e., ≥500 mg/m2) methotrexate therapy; consider rescue therapy for intermediate-dose (100–500 mg/m2) methotrexate therapy.
-
Patients administered high-dose regimens should receive IV fluid hydration and urine alkalinization (to a urinary pH ≥7) throughout treatment. Consider such strategies for patients administered intermediate-dose regimens as well.
-
For non-oncologic indications (i.e., polyarticular juvenile idiopathic arthritis, rheumatoid arthritis, and psoriasis), administer folic acid or folinic acid along with methotrexate to reduce the risk of adverse reactions from methotrexate.
Dispensing and Administration Precautions
-
Based on the Institute for Safe Medication Practices (ISMP), methotrexate is a high-alert medication that has a heightened risk of causing significant patient harm when used in error.
-
Procedures for proper handling and disposal of antineoplastic drugs should be followed when preparing or administering methotrexate.
-
According to the ISMP, brand and generic methotrexate products can be confused with other drug products on the market and require special safeguards to reduce the risk of errors (e.g., using both brand and generic names on prescriptions and labels, including the purpose of the medication on prescriptions, configuring computer systems to require a minimum of the first 5 letters of a drug name during product searches, and changing the appearance of look-alike product names).
-
Use only preservative-free products when treating neonates or low-birth weight infants. Preservative-free formulations also must be used for intrathecal or high-dose regimens.
-
Deaths have occurred due to medication errors, most often when methotrexate was administered daily when a weekly regimen was prescribed. When a once weekly dosing regimen is prescribed, instruct patients and caregivers to take the dosage as directed. Instruct patients and caregivers on how to measure, dose, and administer the recommended dosage as directed.
Other General Considerations
-
Administer glucarpidase in patients with toxic plasma methotrexate concentrations (>1 µmol/L) and delayed methotrexate clearance due to impaired renal function.
-
When switching the dosing regimen between oral administration and IV, IM, or subcutaneous (sub-Q), consider potential differences in bioavailability; an alternative dosing regimen may be necessary.
Administration
Administer orally as tablets or oral solution or by IM, IV, sub-Q, or intrathecal injection; may also administer powder for injection intra-arterially. Some injectable preparations (Rasuvo and Otrexup) only administered sub-Q. Rasuvo only available in doses between 7.5–30 mg in 2.5 mg increments and Otrexup only available in doses between 10–25 mg in 2.5 mg increments; use a different formulation for dosing via oral, IM, IV, intraarterial, or intrathecal routes, weekly doses above or below available strengths for these products, high-dose regimens, or dosage adjustments in increments <2.5 mg.
Powder for injection requires reconstitution according to manufacturers’ directions. Injection is available as a single-dose vial that is ready for use. Rasuvo and Otrexup (injection for sub-Q use) are commercially available in single-use, prefilled auto-injectors.
Oral Tablets and Solution
Administer orally as tablets or oral solution.
Instruct patients or caregivers on proper dosing of oral solution, including the importance of an accurate measuring device; a household teaspoon is not an accurate measuring device. Jylamvo oral solution comes copackaged with a syringe and bottle adapter, which should be used to measure the dose.
Do not administer tablets to patients unable to swallow tablets.
Powder for Injection
Administer by IM, IV, sub-Q, or intrathecal injection; may also administer intra-arterially. Formulations or diluents containing preservatives must not be used for intrathecal administration or high-dose therapy; also use only preservative-free products when treating neonates or low-birth weight infants.
Reconstitution
Reconstitute lyophilized powder for injection immediately before use with a sterile, preservative-free solution (e.g., 5% dextrose injection, 0.9% sodium chloride injection).
Reconstitute 1 g vial with 19.4 mL of appropriate solution to yield a concentration of 50 mg/mL.
Dilution
When high doses are administered by IV infusion, dilute total dose of reconstituted solution in 5% dextrose injection.
If product is to be administered intrathecally, dilute to a concentration of 1 mg/mL with appropriate sterile, preservative-free medium such as 0.9% sodium chloride injection.
Injection
Administer by IM, IV, sub-Q, or intrathecal injection.
Dilution
May be diluted immediately prior to use with preservative-free 0.9% sodium chloride injection.
If product is to be administered intrathecally, dilute to a concentration of 1 mg/mL with appropriate sterile, preservative-free medium such as 0.9% sodium chloride injection.
Formulations or diluents containing preservatives must not be used for intrathecal administration or high-dose therapy; also use only preservative-free products when treating neonates or low-birth weight infants.
Injection for Sub-Q Use
Rasuvo and Otrexup available as single-dose autoinjectors for sub-Q use only; administer in abdomen or thigh.
Dosage
Available as methotrexate sodium; dosage is expressed in terms of methotrexate.
Pediatric Patients
Lymphoma
IV
Dosage of injection or powder for injection varies for this indication.
For combination chemotherapy regimens, dosage of 1000 or 3000 mg/m2 given IV over 24 hours.
When used for CNS-directed therapy, given as an IV infusion over 4 hours at a dosage of 8000 mg/m2 (as a single agent) or at doses ranging from 3000–8000 mg/m2 (in combination with immunochemotherapy).
Intrathecal
Dosage based on age. (see Leukemias under Pediatric Patients)
Osteosarcoma
IV
Initially, 12 g/m2 infused over 4 hours on weeks 4, 5, 6, 7, 11, 12, 15, 16, 29, 30, 44, and 45 after surgery on a schedule in combination with other chemotherapy agents (e.g., doxorubicin; cisplatin; combination of bleomycin, cyclophosphamide, and dactinomycin). If initial dosage is not sufficient to produce peak serum methotrexate concentrations of 454 mcg/mL (1000 µM [10-3 mol/L]) at the end of IV infusion, may increase dose to 15 g/m2 in subsequent treatments.
Polyarticular Juvenile Idiopathic Arthritis
Oral
Initially, 10 mg/m2 once weekly. May adjust dosage gradually to achieve optimal response. Children receiving 20–30 mg/m2weekly may have better absorption and fewer adverse GI effects if administered either IM or sub-Q.
IM or Sub-Q
Initially, 10 mg/m2 once weekly. May adjust dosage gradually to achieve optimal response. Children receiving 20–30 mg/m2 weekly may have better absorption and fewer adverse GI effects if administered either IM or sub-Q.
ALL (Maintenance Therapy)
Oral
When used as part of a combination chemotherapy maintenance regimen, dosage varies based on dosage form. Administer oral solution and tablets at dosage of 20 mg/m2 once weekly.
After treatment initiation, periodically monitor ANC and platelet count and adjust dosage as appropriate.
IM or IV
In general, dosages are highly variable and can range from 10–5000 mg/m2 IV. Individualize dose and schedule based on disease state, patient risk category, concurrent drugs used, phase of treatment, and response to treatment.
When used as part of a combination chemotherapy maintenance regimen, dosage varies based on dosage form.
Powder for injection has been administered twice weekly at a dose of 30 mg/m2 IM or once every 14 days at a dose of 2.5 mg/kg IV.
Meningeal Leukemia
Intrathecal
Injection and powder for injection approved for intrathecal administration for prophylaxis and treatment of meningeal leukemia.
For prophylaxis, administer no more than once weekly; for treatment, administer up to twice weekly.
Recommended intrathecal dosage based on age:
•<1 year: 6 mg
•1 to <2 years: 8 mg
•2 to <3 years: 10 mg
•3 to <9 years: 12 mg
•≥9 years: 12–15 mg
Adults
Breast Cancer
Various combination chemotherapy regimens have been used in the treatment of breast cancer; consult published protocols for dosages and method and sequence of administration.
IV
Prescribing information for methotrexate injection includes dosage of 40 mg/m2 as a component of a cyclophosphamide- and fluorouracil-based multi-drug regimen.
ALL (Maintenance Therapy)
Oral
When used as part of a combination chemotherapy maintenance regimen, dosage varies based on dosage form.
Administer oral solution and tablets at dosage of 20 mg/m2 once weekly.
After treatment initiation, periodically monitor ANC and platelet count and adjust dosage as appropriate.
IM or IV
In general, dosages are highly variable and can range from 10–5000 mg/m2 IV. Individualize dose and schedule based on disease state, patient risk category, concurrent drugs used, phase of treatment, and response to treatment.
When used as part of a combination chemotherapy maintenance regimen, dosage varies based on dosage form.
Powder for injection has been administered twice weekly at a dose of 30 mg/m2 IM or once every 14 days at a dose of 2.5 mg/kg IV.
Meningeal Leukemia
Intrathecal
Injection and powder for injection approved for intrathecal administration for prophylaxis and treatment of meningeal leukemia.
Recommended dosage in adults is 12–15 mg.
For prophylaxis, administer no more than once weekly; for treatment, administer up to twice weekly.
Non-Hodgkins Lymphoma
IV
Dosage of injection or powder for injection varies for this indication.
For combination chemotherapy regimens, dosage of 1000 or 3000 mg/m2 given IV over 24 hours.
When used for CNS-directed therapy, given as an IV infusion over 4 hours at a dosage of 8000 mg/m2 (as a single agent) or at dosages ranging between 3000–8000 mg/m2 (in combination with immunochemotherapy).
Oral
When used as part of a metronomic combination regimen to treat relapsed/refractory non-Hodgkin lymphomas, dosage is 2.5 mg orally given 2-4 times per week (maximum: 10 mg/week).
Intrathecal
12-15 mg.
Cutaneous T-cell Lymphoma; Mycosis Fungoides
Oral
Single agent: 25-75 mg once weekly.
As part of a combination chemotherapy regimen: 10 mg/m2 twice weekly.
IV
5-75 mg.
Combination chemotherapy regimens that include higher- dose methotrexate with leucovorin rescue have been used in advanced stages.
Osteosarcoma
IV
Initially, 12 g/m2 infused over 4 hours on weeks 4, 5, 6, 7, 11, 12, 15, 16, 29, 30, 44, and 45 after surgery on a schedule in combination with other chemotherapy agents (e.g., doxorubicin; cisplatin; combination of bleomycin, cyclophosphamide, and dactinomycin). If initial dosage is not sufficient to produce peak serum methotrexate concentrations of 454 mcg/mL (1000 µM [10-3 mol/L]) at the end of IV infusion, may increase dose to 15 g/m2 in subsequent treatments.
Psoriasis
Oral, IM, Sub-Q, or IV
Initially, 10–25 mg as a single dose once weekly until adequate response achieved. May gradually adjust dosage to achieve optimal response; do not exceed 30 mg weekly ordinarily. Once optimal response obtained, reduce dosage schedule to lowest possible dosage and longest possible rest period. Use of methotrexate to treat psoriasis may allow patients to return to using conventional topical treatments, which should be encouraged.
Rheumatoid Arthritis
Oral, IM, or Sub-Q
Initially, 7.5 mg once weekly, given orally, IM, or sub-Q. May gradually adjust dosage to achieve an optimal response.
At dosages >20 mg weekly, possible increased incidence and severity of serious toxic reactions, especially myelosuppression.
Trophoblastic Diseases
Oral or IM (Powder for Injection)
Usually, 15–30 mg daily for 5 days. Repeat course may be given after a period of ≥1 week, provided all signs of residual toxicity have disappeared; 3–5 courses are usually employed. Clinical assessment before each course is essential.
Therapy is usually evaluated by 24-hour quantitative analysis of urinary chorionic gonadotropin (hCG), which usually normalizes after third or fourth course; complete resolution of measurable lesions usually occurs 4–6 weeks later.
1 or 2 courses of therapy are usually given after normalization of urinary hCG concentrations is achieved.
IM or IV (Injection)
Dosage of methotrexate injection varies by level of disease risk.
Low-risk disease: 30–200 mg/m2 or 0.5–1 mg/kg IV or IM.
High-risk disease: 300 mg/m2 given as a component of a multi-drug regimen via IV infusion over 12 hours.
Crohn's Disease
IM or Sub-Q
Induction of Remission: 25 mg once weekly has been used.
Maintenance Therapy: 15 mg once weekly has been used.
Special Populations
Hepatic Impairment
Adverse reactions from methotrexate may be more likely in patients with hepatic impairment. Use of powder for injection or injection for sub-Q use (Rasuvo and Otrexup) contraindicated for treatment of psoriasis or rheumatoid arthritis in patients with alcoholism, alcoholic liver disease, or other chronic liver disease. Consider reducing dosage or discontinuing in patients with hepatic impairment as appropriate.
Renal Impairment
Methotrexate elimination reduced with renal impairment (Clcr <90 mL/minute using the Cockcroft-Gault calculation); associated with increased risk of adverse reactions. Follow recommendations to promote elimination of methotrexate and decrease risk of acute kidney injury and other toxicities in patients receiving intermediate- or high-dose regimens of methotrexate injection. Consider reducing dosage or discontinuing in patients with renal impairment as appropriate.
Geriatric Patients
No specific dosage recommendations. Select dosage with caution since hepatic and renal function and folate stores may be decreased; closely monitor for early signs of toxicity.
Cautions for Methotrexate
Contraindications
-
History of hypersensitivity to methotrexate.
-
Pregnancy (in patients with non-neoplastic diseases).
-
Lactation (powder for injection only).
-
Alcoholism, alcoholic liver disease, or other chronic liver disease in patients with psoriasis or rheumatoid arthritis.
-
Overt laboratory evidence of immunodeficiency syndromes in patients with psoriasis or rheumatoid arthritis.
-
Preexisting blood dyscrasias (i.e., bone marrow hypoplasia, leukopenia, thrombocytopenia, or significant anemia) in patients with psoriasis or rheumatoid arthritis.
Warnings/Precautions
Warnings
Fetal/Neonatal Morbidity and Mortality
Fetal death and/or congenital anomalies reported (See Boxed Warning). Verify pregnancy status before initiating treatment. Avoid pregnancy if either partner is receiving methotrexate; avoid pregnancy during therapy and for ≥3 months after therapy in male patients and for at least 6 months after therapy in female patients. If used during pregnancy or patient becomes pregnant, apprise of potential fetal hazard. Certain forms of methotrexate contain benzyl alcohol; injection and powder for injection can cross the placenta. If methotrexate injection is administered to treat a neoplastic disease in a pregnant patient, use a preservative-free formulation when possible.
Hypersensitivity and Dermatologic Reactions
Hypersensitivity and/or severe dermatologic reactions have occurred (See Boxed Warning). Hypersensitivity, including anaphylaxis, reported. If signs or symptoms of anaphylaxis or serious hypersensitivity occur, immediately discontinue therapy and institute appropriate management. Severe, occasionally fatal dermatologic reactions (e.g., Stevens-Johnson syndrome, exfoliative dermatitis, skin necrosis, erythema multiforme) reported following single or multiple doses of methotrexate administered via the oral, IM, IV, or intrathecal route in patients with neoplastic and non-neoplastic diseases. Lesions of psoriasis may be aggravated by concomitant exposure to ultraviolet radiation; possible “recall” radiation dermatitis and sunburn with methotrexate use. Monitor for dermatologic toxicity during therapy and counsel patients to use sun protection measures and avoid excessive sun exposure. Consider holding or permanently discontinuing treatment if dermatologic reactions occur.
Risk of Serious Adverse Reactions due to Benzyl Alcohol Preservative
Serious adverse reactions, including severe CNS toxicity or metabolic acidosis, reported when formulations of methotrexate injection or powder for injection containing benzyl alcohol administered to neonates or low-birth weight infants, or given intrathecally or in high-dose regimens (See Boxed Warning). Only administer preservative-free formulations in neonates and low-birth weight infants. If administering to infants who do not fall into these categories, consider combined daily metabolic load of benzyl alcohol from all sources (methotrexate injection contains 9.4 mg benzyl alcohol per mL). Only use preservative-free formulations for intrathecal administration and do not use preserved formulations for high-dose regimens unless it cannot be avoided.
Myelosuppression
Possible suppressed hematopoiesis, anemia, aplastic anemia, pancytopenia, leukopenia, neutropenia, and/or thrombocytopenia (See Boxed Warning). Use with caution in patients with malignancy and preexisting hematopoietic impairment. Perform CBCs at baseline and periodically throughout treatment; monitor patients for possible complications of myelosuppression. If myelosuppression occurs, dosage may need to be reduced, or the drug withheld or discontinued. If profound granulocytopenia and fever occur, evaluate patient immediately and consider initiating parenteral broad- spectrum antibiotic therapy.
Serious Infections
Life-threatening or fatal bacterial, fungal, or viral infections have occurred (See Boxed Warning). Immunizations administered during treatment may be ineffective; disseminated infections following administration of live vaccines in patients receiving methotrexate also reported. Administer all appropriate vaccines according to immunization guidelines prior to treatment initiation; live vaccines not recommended during treatment. Hypogammaglobulinemia reported rarely. Use with extreme caution in presence of active infection; powder for injection and injection for sub-Q use (Rasuvo and Otrexup) contraindicated in patients with overt or laboratory evidence of immunodeficiency syndromes. Monitor for signs and symptoms of infection during treatment; dose may need to be modified, withheld, or discontinued.
Renal Toxicity
May cause renal damage leading to irreversible acute renal failure (See Boxed Warning). Nephrotoxicity is due principally to precipitation of methotrexate and 7-hydroxymethotrexate in the renal tubules. Monitor renal function at baseline and periodically during treatment; withhold or discontinue methotrexate as needed if severe renal toxicity develops. Adequate hydration and urine alkalinization may help ensure safe administration. Follow recommendations to decrease risk of renal injury and mitigate renal toxicity in patients receiving high-dose methotrexate regimens. Consider administration of glucarpidase in patients with laboratory evidence of methotrexate toxicity and delayed clearance due to renal impairment.
Hepatotoxicity
Possible severe and potentially irreversible hepatotoxicity that may cause fibrosis, cirrhosis, and fatal liver failure (See Boxed Warning). Hepatotoxicity generally occurs after prolonged use (≥2 years) and after a total dose of ≥1.5 g. Acute elevations in liver enzymes occur frequently, and are usually transient and not associated with symptoms; such elevations do not appear to predict subsequent hepatic disease. Risk of hepatotoxicity in patients with psoriasis appears to be related to cumulative dose and may be enhanced by alcoholism, obesity, diabetes, and advanced age. Age at first use and duration of therapy reported as risk factors for hepatotoxicity in rheumatoid arthritis patients. Use with particular caution in patients with preexisting liver damage or hepatic impairment. Evaluate liver function prior to initiating therapy and throughout treatment. Perform pretreatment liver biopsy in patients with excessive alcohol consumption, chronic hepatitis B or C infection, or persistently elevated liver function tests at baseline. Liver biopsy should also be performed during treatment based on laboratory findings (e.g., persistent liver function abnormalities or a decrease in serum albumin below the normal range in those with well-controlled rheumatoid arthritis). Methotrexate may need to be withheld or discontinued as appropriate.
Neurotoxicity
Severe acute and chronic neurotoxicity, which can be progressive, irreversible, and fatal, reported (See Boxed Warning). Severe neurotoxic effects, manifested mainly by focal or generalized seizures, reported with increased frequency in pediatric patients receiving methotrexate. High-dose IV regimens, intrathecal administration, and low-dose regimens can cause leukoencephalopathy; risk of leukoencephalopathy further increased in those who have previously received cranial radiation. Transient acute stroke-like syndrome observed in patients receiving high-dosage regimens; manifestations of this stroke-like encephalopathy may include confusion, hemiparesis, transient blindness, seizures, and coma. Intrathecal administration may also cause acute chemical arachnoiditis (symptoms include headache, back pain, nuchal rigidity, and fever) or subacute myelopathy (symptoms include paraparesis or paraplegia). Monitor for neurotoxicity during treatment; withhold or discontinue therapy as appropriate. Avoid intrathecal administration of products that contain benzyl alcohol, which can increase the risk for serious neurotoxicity.
GI Toxicity
Risk of vomiting, diarrhea, stomatitis, hemorrhagic enteritis, and fatal intestinal perforation reported (See Boxed Warning); if severe GI toxicity occurs, withhold or discontinue drug and institute supportive care as appropriate. Use with caution in presence of peptic ulcer disease or ulcerative colitis.
Pulmonary Toxicity
Potentially fatal pulmonary toxicity (e.g., acute or chronic interstitial pneumonitis) may occur at any dosage at any time during therapy (See Boxed Warning). If manifestations (e.g., dry, nonproductive cough) occur, withhold or discontinue as appropriate.
Additional Boxed Warnings Unique to Specific Formulations
Powder for injection and Rasuvo (injection for sub-Q use) should only be used in select patients with severe disease (See Boxed Warning). Reserve treatment for life-threatening malignancies, or psoriasis or rheumatoid arthritis that is severe, recalcitrant, disabling, and unresponsive to other forms of therapy; deaths have been reported when used for these indications. Inform patients of these risks. Patients should remain under a physician’s care throughout treatment. Use of high-dose regimens for treatment of osteosarcoma requires meticulous care; use of high-dose regimens for other malignancies is investigational. Secondary malignant lymphomas reported in patients prescribed low-dose therapy; boxed warning included in prescribing information for powder for injection and Rasuvo (injection for sub-Q use) (See Boxed Warning). Lymphomas may regress following treatment discontinuation; institute appropriate treatment if lymphoma does not regress. Other formulations include a warning pertaining to this risk. Tumor lysis syndrome has occurred in patients with rapidly growing tumors; boxed warning included in prescribing information for powder for injection and Rasuvo(injection for sub-Q use) (See Boxed Warning). May be alleviated or prevented with appropriate supportive care and pharmacologic measures. Other formulations include a warning pertaining to this risk. Soft tissue necrosis and osteonecrosis have occurred with concomitant radiotherapy; boxed warning included in prescribing information for powder for injection and Rasuvo (injection for sub-Q use) (See Boxed Warning). Some other formulations include a warning pertaining to this risk.
Folic Acid Supplementation
Patients with neoplastic diseases: products containing folic acid or derivatives may reduce effectiveness of methotrexate; avoid unless clinically indicated. Patients with non-neoplastic diseases: Folate deficiency may increase likelihood of methotrexate-associated adverse reactions; administer concomitant folic acid or folinic acid.
Infertility
Impaired fertility, oligospermia, and menstrual dysfunction reported; unknown if reversible. Discuss risk of infertility with patients of reproductive potential prior to treatment initiation.
Increased Toxicity Due to Third Space Accumulation
Exits slowly from third-space compartments (e.g., pleural effusions, ascites), resulting in prolonged half-life and associated toxicity in patients with substantial third-space accumulations. Evacuation of fluid recommended before treatment.
Risk of Severe Adverse Reactions with Medication Errors
Serious adverse reactions, including death, have occurred due to medication errors (most commonly daily administration when a weekly regimen was prescribed). Verify dosage in all patients prescribed methotrexate. Measure oral solution using an accurate milliliter measuring device. A household teaspoon is not an accurate measuring device, and use of such could result in overdosage leading to serious adverse reactions. Advise patients to ask their pharmacist to recommend an appropriate measuring device and counsel on how to use it.
Dizziness and Fatigue
Dizziness and fatigue reported with powder for injection and injection for sub-Q use (Rasuvo and Otrexup); can affect ability to drive or operate machinery.
Specific Populations
Pregnancy
Abortion, fetal death, and/or congenital anomalies have occurred, especially during the first trimester. Methotrexate contraindicated in the management of all non-neoplastic disorders (i.e., psoriasis or rheumatoid arthritis [including polyarticular juvenile idiopathic arthritis]) in pregnant women. Verify pregnancy status prior to treatment initiation. Advise female patients of reproductive potential to use effective contraception during treatment and for 6 months after discontinuation; advise males with such female partners to use effective contraception during treatment and for 3 months after discontinuation. Inform women of childbearing potential of the potential hazard to the fetus.
If methotrexate injection is administered to treat a neoplastic disease in a pregnant patient, use a preservative-free formulation when possible.
Lactation
Distributed into milk; reported breast milk to plasma concentration ratio as high as 0.08:1. Potential effects on the breast-fed infant or on milk production not known. Powder for injection is contraindicated in nursing women because of risk to nursing infant. Advise patients taking all other formulations to avoid breast-feeding during treatment and for 1 week after discontinuation.
Females and Males of Reproductive Potential
Defective oogenesis or spermatogenesis, oligospermia, menstrual dysfunction, and infertility reported. Can cause fetal malformations and fetal death when administered during pregnancy. Can cause chromosomal damage to sperm cells.
Verify pregnancy status prior to treatment initiation. Advise female patients of reproductive potential to use effective contraception during treatment and for 6 months after discontinuation. Advise male patients with such female partners to use effective contraception during treatment and for 3 months following discontinuation.
Pediatric Use
Safety and efficacy established (all formulations) in pediatric patients for treatment of polyarticular juvenile idiopathic arthritis.
Safety and efficacy also established for injection and powder for injection in pediatric patients for treatment of acute lymphoblastic leukemia (ALL), meningeal leukemia prophylaxis and treatment, non-Hodgkin lymphoma, and osteosarcoma. Severe neurotoxic effects (e.g., focal or generalized seizures) reported in pediatric patients with ALL who received intermediate-dose IV therapy (1 g/m2). Safety and efficacy of injection and powder for injection have not been established in pediatric patients for other types of cancer, including breast cancer, squamous cell carcinoma of the head and neck, and gestational trophoblastic diseases.
Safety and efficacy of oral solution and tablets established in pediatric patients for the treatment of ALL, but not established for treatment of other neoplastic diseases. Safety and efficacy of Rasuvo and Otrexup (methotrexate injection for sub-Q use) not established in pediatric patients for treatment of any neoplastic diseases.
Safety and efficacy (all formulations) not established in pediatric patients for treatment of rheumatoid arthritis or psoriasis.
Geriatric Use
Insufficient experience in patients ≥65 years of age to determine whether geriatric patients respond differently than younger adults; select dosage with caution due to greater frequency of decreased hepatic and renal function and folate stores and possibility of concomitant diseases and drug therapy observed in the elderly. Occurrence of bone marrow suppression, thrombocytopenia, and pneumonitis may increase with age.
Hepatic Impairment
Pharmacokinetics not known in patients with hepatic impairment. Powder for injection and injection for sub-Q use (Rasuvo and Otrexup) contraindicated in patients with psoriasis or rheumatoid arthritis who have alcoholism, alcoholic liver disease, or other chronic liver disease. Patients with obesity, diabetes, hepatic fibrosis, or steatohepatitis at increased risk for hepatic injury and fibrosis from methotrexate; monitor such patients closely. Consider dosage reduction or discontinuance in patients with hepatic impairment.
Renal Impairment
Elimination reduced with renal impairment (i.e., Clcr <90 mL/minute using the Cockcroft-Gault calculation). Follow recommendations to promote methotrexate elimination and decrease risk of acute kidney injury and other toxicities in patients receiving intermediate- or high-dose regimens. Carefully monitor patients with renal impairment during treatment; consider dosage reduction or discontinuance in patients with renal impairment.
Debilitated Patients
Use with caution.
Common Adverse Effects
The most common adverse effects reported in patients receiving methotrexate injection, powder for injection, oral solution, and tablets include ulcerative stomatitis, leukopenia, nausea, and abdominal distress. Elevated liver function tests are also commonly reported in patients receiving Xatmep oral solution.
The most common adverse effects reported in patients receiving methotrexate injection for sub-Q use include nausea, abdominal pain, dyspepsia, stomatitis/mouth sores, rash, nasopharyngitis, diarrhea, liver function test abnormalities, vomiting, headache, bronchitis, thrombocytopenia, alopecia, leukopenia, pancytopenia, dizziness, photosensitivity, and "burning of skin lesions."
Drug Interactions
Protein-bound Drugs and Weak Organic Acids
Possible increased methotrexate toxicity because of displacement from protein binding sites. If coadministration cannot be avoided, monitor for adverse reactions from methotrexate during therapy.
Hepatotoxic Agents
Increase in adverse effects expected. If coadministration cannot be avoided, monitor for adverse reactions from methotrexate during therapy.
Nephrotoxic Drugs
Increase in adverse effects expected. If coadministration cannot be avoided, monitor for adverse reactions from methotrexate during therapy.
Specific Drugs
|
Drug |
Interaction |
Comments |
|---|---|---|
|
Azathioprine |
Possible increased risk of hepatotoxicity |
Closely monitor for toxicity |
|
Chloramphenicol |
Possible increased methotrexate toxicity because of displacement from protein binding sites |
Closely monitor for toxicity |
|
Co-trimoxazole |
Sulfonamides can displace methotrexate from plasma protein-binding sites resulting in increased free methotrexate concentrations |
Monitor closely for adverse effects |
|
Folic acid (e.g., multivitamins) |
Potential for decreased methotrexate effectiveness |
Advise patients to only take folic acid or folinic acid products as directed by their healthcare provider |
|
Mercaptopurine |
Increased plasma mercaptopurine concentrations |
May require dosage adjustment |
|
Neomycin |
Possible increased methotrexate plasma concentrations |
Carefully monitor patients during concomitant use |
|
Nitrous oxide anesthesia |
Potentiation of methotrexate's effects on folate-dependent metabolic pathways, increasing the risk for severe adverse reactions from methotrexate |
Avoid concomitant use Consider alternative therapies in patients who previously received nitrous oxide anesthesia |
|
NSAIAs (including aspirin/salicylates) |
Severe, sometimes fatal, hematologic and GI toxicity reported when NSAIAs used concomitantly with high-dose methotrexate Possible increased methotrexate toxicity because of displacement from protein binding sites by salicylates |
If coadministration cannot be avoided, monitor closely for toxicity |
|
Oral antibiotics |
Possible increased methotrexate plasma concentrations |
Carefully monitor patients during concomitant use |
|
Oral anticoagulants |
Possible increased methotrexate toxicity because of displacement from protein binding sites |
Closely monitor for toxicity |
|
Penicillins |
Possible increased methotrexate plasma concentrations |
Carefully monitor patients during concomitant use |
|
Phenytoin |
Possible increased methotrexate toxicity because of displacement from protein binding sites |
Closely monitor for toxicity |
|
Probenecid |
Increased plasma concentrations of methotrexate |
Consider alternate drugs or carefully monitor |
|
Proton-pump inhibitors (e.g., esomeprazole, omeprazole, pantoprazole) |
Possible increased serum concentrations of methotrexate |
If coadministration cannot be avoided, closely monitor for toxicity |
|
Retinoids |
Possible increased risk of hepatotoxicity |
Closely monitor for toxicity |
|
Sulfasalazine |
Possible increased risk of hepatotoxicity |
Closely monitor for toxicity |
|
Sulfonamides |
Possible increased methotrexate toxicity because of displacement from protein binding sites |
Monitor closely for adverse effects |
|
Sulfonylureas |
Possible increased methotrexate toxicity because of displacement from protein binding sites |
Monitor closely for adverse effects |
|
Tetracyclines |
Possible increased methotrexate toxicity because of displacement from protein binding sites |
Monitor for adverse reactions if used concomitantly. |
|
Theophylline |
Possible increased theophylline serum concentrations |
Monitor serum theophylline concentrations and adjust dosage as appropriate |
Methotrexate Pharmacokinetics
Absorption
Bioavailability
Oral absorption appears to be highly variable and dose dependent. At lower doses (i.e., ≤30 mg/m2), dose is well absorbed with a mean bioavailability of approximately 60%. Bioavailability decreases with increasing oral doses; absorption may be substantially reduced at doses >80 mg/m2.
Appears to be completely absorbed following parenteral administration. Peak serum concentrations attained within 0.75-6 hours after oral administration and 30–60 minutes after IM administration.
Food
Food delays absorption and decreases peak serum concentrations following oral administration.
Distribution
Extent
Actively transported across cell membranes. At concentrations >0.1 µmol/mL, passive diffusion becomes a major means of intracellular transport.
Does not reach therapeutic concentrations in the CSF when administered orally or parenterally; high CSF concentrations can be attained following intrathecal administration.
Plasma Protein Binding
About 50%.
Elimination
Metabolism
Undergoes hepatic and intracellular metabolism to polyglutamate metabolites; partially metabolized by intestinal flora after oral administration.
Polyglutamate metabolites may be converted back to methotrexate by hydrolysis, and metabolites may remain in tissues for extended periods of time.
Elimination Route
Excreted principally by the kidneys (up to 90%) and to a lesser extent via feces (≤10%).
Half-life
At low-doses (<30 mg/m2), terminal half-life is about 3–10 hours. At high IV doses, elimination half-life is about 8–15 hours in adults. In pediatric patients, terminal half-life ranges from 0.7-5.8 hours in those with acute lymphoblastic leukemia or 0.9-2.3 hours in those with polyarticular juvenile idiopathic arthritis.
Stability
Storage
Oral
Solution
Jylamvo (methotrexate 2 mg/mL oral solution): 20–25°C; excursions permitted between 15–30°C. Once in use, store at 20–25°C and keep bottle tightly closed. Discard any unused medicine after 3 months from date of opening. Xatmep (methotrexate 2.5 mg/mL oral solution): 2–8°C, tightly closed in the original container. Once dispensed, can be stored refrigerated at 2–8°C or at room temperature at 20–25°C, with excursions permitted between 15–30°C. Discard any unused medicine after 60 days if stored at room temperature. Avoid freezing and exposure to excessive heat.
Tablets
2.5 mg tablets: 20–25°C; excursions permitted between 15–30°C.
High-dose tablets (Trexall): 20–25°C. Protect from light.
Parenteral
Injection
20–25°C. Protect from light.
Use preservative-free solution immediately after further dilution.
Injection, for Sub-Q Use
20–25°C (excursions permitted between 15–30°C). Protect from light.
Powder for Injection
20–25°C. Protect from light.
Actions
-
Methotrexate and its polyglutamate metabolites reversibly inhibit dihydrofolate reductase (enzyme that reduces folic acid to tetrahydrofolic acid); inhibition of tetrahydrofolate formation limits availability of one-carbon fragments necessary for synthesis of purines and pyrimidines and various other reactions necessary for DNA synthesis and cell reproduction.
-
In cancer, malignant cells are unable to synthesize DNA and RNA without purine and pyrimidine precursors and thus, become unable to proliferate.
-
Tissues with high rates of cellular proliferation (e.g., neoplasms, buccal and intestinal mucosa, bone marrow, bladder, fetal cells) are most sensitive.
-
Mechanism(s) of action in rheumatoid arthritis, polyarticular juvenile idiopathic arthritis, and psoriasis not known; however, may have effects on immune system.
Advice to Patients
-
Advise patients to read the FDA-approved patient labeling (Patient Information).
-
Inform patients of the risks of infections and organ toxicity, including gastrointestinal, hematologic, hepatic, neurologic, pulmonary, renal, and skin toxicity, as well as possible signs and symptoms for which they should contact their healthcare provider. Advise patients of the need for close follow-up, including periodic laboratory tests to monitor toxicity.
-
For patients prescribed a once weekly regimen of methotrexate, advise patients and caregivers that the dose is taken once weekly and that mistaken daily use of the recommended dose has led to fatal toxicity.
-
Rasuvo and Otrexup are intended for use under the guidance and supervision of a physician. Patients should not self-administer until they receive training from a healthcare professional. Assess the patient or caregiver's ability to administer these medications.
-
When administering Rasuvo and Otrexup, patients should be instructed to use administration sites on the abdomen or the thigh. Administration should not be made within 2 inches of the navel. Instruct patients not to administer to the arms or any other areas of the body, as delineated in the Instructions for Use.
-
Advise patients of the potential risk of hypersensitivity and that methotrexate is contraindicated in patients with a history of severe hypersensitivity to methotrexate. Advise patients to seek immediate medical attention if signs or symptoms of a hypersensitivity reaction occur.
-
Inform patients and their caregivers that methotrexate can cause myelosuppression and that frequent monitoring of blood cell counts is needed. Advise patients to contact their healthcare provider immediately for new onset fever, symptoms of infection, easy bruising, or persistent bleeding.
-
Inform patients that adverse reactions such as dizziness and fatigue may affect their ability to drive or operate machinery.
-
Advise patients that methotrexate can cause renal toxicity. Advise patients to immediately contact their healthcare provider for signs or symptoms of renal toxicity, such as marked increases or decreases in urinary output.
-
Advise patients to report signs or symptoms of hepatic toxicity and to avoid alcohol during methotrexate treatment.
-
Advise patients to contact their healthcare provider immediately if they develop new neurological symptoms.
-
Advise patients to contact their healthcare provider if they develop diarrhea, vomiting, or stomatitis. Advise patients to immediately contact their healthcare provider for high fever, rigors, persistent or severe abdominal pain, severe constipation, hematemesis, or melena.
-
Advise patients to contact their healthcare provider for new or worsening symptoms of cough, fever, and dyspnea.
-
Advise patients that methotrexate injection can cause serious skin rash and to immediately contact their healthcare provider for new or worsening skin rash. Advise patients to avoid excessive sun exposure and to use sun protection measures.
-
Advise patients on the risk of second primary malignancies during treatment with methotrexate.
-
Advise patients to avoid receiving vaccines during treatment with methotrexate because they may not be effective and live virus vaccines may cause infection.
-
Advise women to inform their clinician if they are or plan to become pregnant. Advise females of reproductive potential that methotrexate should not be started until pregnancy is excluded.
-
Advise women to inform their clinician if they are or plan to breast-feed. Advise women not to breast-feed during treatment with methotrexate[r6] and for 1 week after the final dose.
-
Advise females and males of reproductive potential that methotrexate may cause impairment of fertility. Methotrexate can also cause oligospermia and menstrual dysfunction.
-
Advise females of reproductive potential to use effective contraception during methotrexate therapy and for 6 months after the final dose. Advise males of reproductive potential to use effective contraception during methotrexate therapy and for 3 months after the final dose.
-
Advise patients to inform their clinician of existing or contemplated concomitant therapy, including prescription and OTC drugs and dietary and herbal supplements, as well as any concomitant illnesses.
-
Instruct patients being treated for neoplastic indications to not take products containing folic acid or folinic acid unless directed to do so by their healthcare provider.
-
Advise patients on how to properly store and dispose of methotrexate products. Inform patients and caregivers of the need for proper disposal of Rasuvo and Otrexup after use, including the use of a sharps disposal container.
-
Instruct patients and caregivers how to measure, dose, and administer the recommended dosage of methotrexate oral solution using an appropriate measuring device and that a household teaspoon is not an appropriate measuring device.
-
Advise patients of other important precautionary information.
Additional Information
The American Society of Health-System Pharmacists, Inc. represents that the information provided in the accompanying monograph was formulated with a reasonable standard of care, and in conformity with professional standards in the field. Readers are advised that decisions regarding use of drugs are complex medical decisions requiring the independent, informed decision of an appropriate health care professional, and that the information contained in the monograph is provided for informational purposes only. The manufacturer’s labeling should be consulted for more detailed information. The American Society of Health-System Pharmacists, Inc. does not endorse or recommend the use of any drug. The information contained in the monograph is not a substitute for medical care. For further information on the handling of antineoplastic agents, see the ASHP Guidelines on Handling Hazardous Drugs at [Web].
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
* available from one or more manufacturer, distributor, and/or repackager by generic (nonproprietary) name
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Solution |
2 mg (of methotrexate) per mL |
Jylamvo |
|
|
2.5 mg (of methotrexate) per mL |
Xatmep |
|||
|
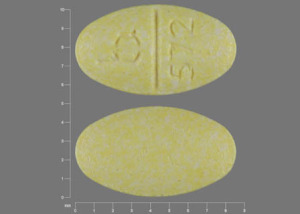
Tablets |
2.5 mg (of methotrexate)* |
Methotrexate Sodium Tablets (scored) |
||
|
Tablets, film-coated |
5 mg (of methotrexate) |
Trexall (scored) |
Teva |
|
|
7.5 mg (of methotrexate) |
Trexall (scored) |
Teva |
||
|
10 mg (of methotrexate) |
Trexall (scored) |
Teva |
||
|
15 mg (of methotrexate) |
Trexall (scored) |
Teva |
||
|
Parenteral |
For injection |
1 g (of methotrexate)* |
Methotrexate Sodium for Injection |
|
|
Injection |
25 mg (of methotrexate) per mL* |
Methotrexate Sodium Injection Isotonic |
||
|
Injection, for subcutaneous use |
10 mg/0.4 mL |
Otrexup (available as single-dose prefilled auto-injectors) |
||
|
12.5 mg/0.4 mL |
Otrexup (available as single-dose prefilled auto-injectors) |
|||
|
15 mg/0.4 mL |
Otrexup (available as single-dose prefilled auto-injectors) |
|||
|
17.5 mg/0.4 mL |
Otrexup (available as single-dose prefilled auto-injectors) |
|||
|
20 mg/0.4 mL |
Otrexup (available as single-dose prefilled auto-injectors) |
|||
|
22.5 mg/0.4 mL |
Otrexup (available as single-dose prefilled auto-injectors) |
|||
|
25 mg/0.4 mL |
Otrexup (available as single-dose prefilled auto-injectors) |
|||
|
50 mg/mL |
Rasuvo (available as single-dose prefilled auto-injectors in 7.5, 10, 12.5, 15, 17.5, 20, 22.5, 27.5, and 30 mg dosage strengths) |
AHFS DI Essentials™. © Copyright 2025, Selected Revisions March 10, 2025. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
† Off-label: Use is not currently included in the labeling approved by the US Food and Drug Administration.
Reload page with references included
Related/similar drugs
Frequently asked questions
- How long does chemo take? Sessions and recovery time?
- How soon can you start chemo after port placement?
- Why should I take folic acid with methotrexate?
- How long does it take for methotrexate to work?
- Does methotrexate cause weight gain?
- How do I know if methotrexate is working for rheumatoid arthritis?
- Radiation vs. Chemo: Which cancer treatment is right for you?
- What is chemo brain and how long does it last?
- What are the different brands of methotrexate?
More about methotrexate
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (339)
- Drug images
- Side effects
- Dosage information
- Patient tips
- During pregnancy
- Support group
- Drug class: antimetabolites
- Breastfeeding
Patient resources
Professional resources
Other brands
Otrexup, Rasuvo, Trexall, Xatmep, ... +3 more