Ortho-Est (Oral)
Generic name: estropipate [ es-troe-PIP-ate ]
Other brand names of estropipate include: Ogen .625, Ogen 1.25, Ogen 2.5, Ortho-Est
Drug class: Estrogens
Medically reviewed by Drugs.com. Last updated on Apr 25, 2025.
The Ortho-Est brand name has been discontinued in the U.S. If generic versions of this product have been approved by the FDA, there may be generic equivalents available.
Estrogen-Alone Therapy
Endometrial Cancer
There is an increased risk of endometrial cancer in a woman with a uterus who uses unopposed estrogens. Adding a progestin to estrogen therapy has been shown to reduce the risk of endometrial hyperplasia, which may be a precursor to endometrial cancer. Adequate diagnostic measures, including directed or random endometrial sampling when indicated, should be undertaken to rule out malignancy in postmenopausal women with undiagnosed persistent or recurring abnormal genital bleeding.
Cardiovascular Disorders and Probable Dementia
Estrogen-alone therapy should not be used for the prevention of cardiovascular disease or dementia. The Women's Health Initiative (WHI) estrogen-alone substudy reported increased risks of stroke and deep vein thrombosis (DVT) in postmenopausal women (50 to 79 years of age) during 7.1 years of treatment with daily oral conjugated estrogens (CE) [0.625 mg]- alone, relative to placebo. The WHI Memory Study (WHIMS) estrogen-alone ancillary study of the WHI reported an increased risk of developing probable dementia in postmenopausal women 65 years of age or older during 5.2 years of treatment with daily CE (0.625 mg) alone relative to placebo. It is unknown whether this finding applies to younger postmenopausal women. In the absence of comparable data, these risks should be assumed to be similar for other doses of CE and other dosage forms of estrogens. Estrogens with or without progestins should be prescribed at the lowest effective doses and for the shortest duration consistent with treatment goals and risks for the individual woman.
Estrogen Plus Progestin Therapy
Cardiovascular Disorders and Probable Dementia
Estrogen plus progestin therapy should not be used for the prevention of cardiovascular disease or dementia.
The WHI estrogen plus progestin substudy reported increased risks of DVT, pulmonary embolism (PE), stroke and myocardial infarction (MI) in postmenopausal women (50 to 79 years of age) during 5.6 years of treatment with daily oral CE (0.625 mg) combined with medroxyprogesterone acetate (MPA) [2.5 mg], relative to placebo. The WHIMS estrogen plus progestin ancillary study of the WHI reported an increased risk of developing probable dementia in postmenopausal women 65 years of age or older during 4 years of treatment with daily CE (0.625 mg) combined with MPA (2.5 mg), relative to placebo. It is unknown whether this finding applies to younger postmenopausal women.
Breast Cancer
The WHI estrogen plus progestin substudy also demonstrated an increased risk of invasive breast cancer. In the absence of comparable data, these risks should be assumed to be similar for other doses of CE and MPA, and other combinations and dosage forms of estrogens and progestins. Estrogens with or without progestins should be prescribed at the lowest effective doses and for the shortest duration consistent with treatment goals and risks for the individual woman .
Uses for Ortho-Est
Estropipate is used to treat moderate to severe symptoms of menopause. It is also used to treat changes in and around the vagina (such as vaginal dryness, itching, and burning) caused by low estrogen levels or menopause. This medicine is also used to treat certain conditions in women before menopause if their ovaries do not make enough estrogens naturally, and prevent osteoporosis after menopause.
Estropipate is an estrogen hormone that works by preventing symptoms, such as feelings of warmth in the face, neck, and chest, or sudden strong feelings of heat and sweating (hot flashes) in women during menopause.
This medicine is available only with your doctor's prescription.
Before using Ortho-Est
In deciding to use a medicine, the risks of taking the medicine must be weighed against the good it will do. This is a decision you and your doctor will make. For this medicine, the following should be considered:
Allergies
Tell your doctor if you have ever had any unusual or allergic reaction to this medicine or any other medicines. Also tell your health care professional if you have any other types of allergies, such as to foods, dyes, preservatives, or animals. For non-prescription products, read the label or package ingredients carefully.
Pediatric
Use of estropipate is not indicated in children.
Geriatric
Although appropriate studies on the relationship of age to the effects of estropipate have not been performed in the geriatric population, no geriatric-specific problems have been documented to date. However, elderly patients are more likely to have breast cancer, strokes, or dementia, which may require caution in patients receiving this medicine.
Breast Feeding
Studies suggest that this medication may alter milk production or composition. If an alternative to this medication is not prescribed, you should monitor the infant for side effects and adequate milk intake.
Interactions with Medicines
Although certain medicines should not be used together at all, in other cases two different medicines may be used together even if an interaction might occur. In these cases, your doctor may want to change the dose, or other precautions may be necessary. When you are taking this medicine, it is especially important that your healthcare professional know if you are taking any of the medicines listed below. The following interactions have been selected on the basis of their potential significance and are not necessarily all-inclusive.
Using this medicine with any of the following medicines is usually not recommended, but may be required in some cases. If both medicines are prescribed together, your doctor may change the dose or how often you use one or both of the medicines.
- Amifampridine
- Bupropion
- Donepezil
- Somatrogon-ghla
Using this medicine with any of the following medicines may cause an increased risk of certain side effects, but using both drugs may be the best treatment for you. If both medicines are prescribed together, your doctor may change the dose or how often you use one or both of the medicines.
- Ginseng
- Levothyroxine
- Licorice
- Tipranavir
Interactions with Food/Tobacco/Alcohol
Certain medicines should not be used at or around the time of eating food or eating certain types of food since interactions may occur. Using alcohol or tobacco with certain medicines may also cause interactions to occur. Discuss with your healthcare professional the use of your medicine with food, alcohol, or tobacco.
Other Medical Problems
The presence of other medical problems may affect the use of this medicine. Make sure you tell your doctor if you have any other medical problems, especially:
- Abnormal or unusual vaginal bleeding or
- Blood clots (eg, deep vein thrombosis, pulmonary embolism), active or history of or
- Breast cancer, known or suspected, or a history of or
- Heart attack, history of or
- Liver disease or
- Protein C, protein S, or other known blood clotting disorders or
- Stroke, history of or
- Tumors (estrogen-dependent), known or suspected—Should not be used in patients with these conditions.
- Asthma or
- Bone problems or
- Diabetes or
- Edema (fluid retention or body swelling) or
- Endometriosis or
- Epilepsy (seizures) or
- Gallbladder disease or
- Hereditary angioedema (swelling of the face, lips, tongue, or throat) or
- Hypercalcemia (high calcium in the blood) or
- Hypocalcemia (low calcium in the blood) or
- Hypothyroidism (an underactive thyroid) or
- Jaundice during pregnancy or from using hormonal therapy in the past or
- Liver tumors or
- Migraine headache or
- Porphyria (an enzyme problem) or
- Systemic lupus erythematosus (SLE)—Use with caution. May make these conditions worse.
- Heart disease or
- Hypercholesterolemia (high cholesterol or fats in the blood) or
- Hypertension (high blood pressure) or
- Hypertriglyceridemia (high triglycerides or fats in the blood) or
- Obesity, or history of or
- Prolonged periods of immobilization—Use with caution. These conditions may increase risk for more serious side effects.
Proper use of Ortho-Est
It is very important that you use this medicine exactly as directed by your doctor. Do not use more of it, do not use it more often, and do not use it for a longer time than your doctor ordered. To do so may cause unwanted side effects.
This medicine comes with a patient information leaflet. Read and follow the instructions carefully. Ask your doctor if you have any questions.
Do not eat grapefruit or drink grapefruit juice while you are using this medicine. Grapefruit and grapefruit juice may change the amount of this medicine that is absorbed in the body.
Dosing
The dose of this medicine will be different for different patients. Follow your doctor's orders or the directions on the label. The following information includes only the average doses of this medicine. If your dose is different, do not change it unless your doctor tells you to do so.
The amount of medicine that you take depends on the strength of the medicine. Also, the number of doses you take each day, the time allowed between doses, and the length of time you take the medicine depend on the medical problem for which you are using the medicine.
- For oral dosage form (tablets):
- For hot flashes and other symptoms caused by menopause:
- Adults—One Ogen® 0.625 (0.75 mg estropipate) tablet to two Ogen® 2.5 (3 mg estropipate) tablets per day.
- Children—Use is not recommended.
- For treatment of changes in and around the vagina (such as vaginal dryness, itching, and burning) caused by low estrogen levels or menopause.
- Adults—One Ogen® 0.625 (0.75 mg estropipate) tablet to two Ogen® 2.5 (3 mg estropipate) tablets per day.
- Children—Use is not recommended.
- For female hypogonadism, female castration, or primary ovarian failure:
- Adults—One Ogen® 1.25 (1.5 mg estropipate) tablet to three Ogen® 2.5 (3 mg estropipate) tablets per day may be given for the first 3 weeks of a cycle, followed by a rest period of 8 to 10 days. Your doctor may adjust your dose as needed and tolerated.
- Children—Use is not recommended.
- For prevention of osteoporosis after menopause:
- Adults—One Ogen® 0.625 (0.75 mg estropipate) tablet for 25 days of a 31-day cycle per month.
- Children—Use is not recommended.
- For hot flashes and other symptoms caused by menopause:
Missed Dose
If you miss a dose of this medicine, take it as soon as possible. However, if it is almost time for your next dose, skip the missed dose and go back to your regular dosing schedule. Do not double doses.
Storage
Store the medicine in a closed container at room temperature, away from heat, moisture, and direct light. Keep from freezing.
Keep out of the reach of children.
Do not keep outdated medicine or medicine no longer needed.
Ask your healthcare professional how you should dispose of any medicine you do not use.
Precautions while using Ortho-Est
It is very important that your doctor check your progress at regular visits to make sure this medicine is working properly and does not cause unwanted effects. Blood tests, pelvic exam, breast exam, and mammogram (breast x-ray) may be needed to check for unwanted effects, unless your doctor tells you otherwise. Be sure to keep all appointments.
It is unlikely that a postmenopausal woman may become pregnant. But, you should know that using this medicine while you are pregnant could harm your unborn baby. If you think you have become pregnant while using the medicine, tell your doctor right away.
Using this medicine may increase your risk for having blood clots, strokes, or heart attacks. This risk may continue even after you stop using the medicine. Your risk for these serious problems is even greater if you have high blood pressure, high cholesterol in your blood, diabetes or are overweight or smoke cigarettes. Contact your doctor immediately if you experience chest pain, confusion, difficulty speaking, double vision, headaches, an inability to move arms, legs or facial muscle, or an inability to speak.
Using this medicine may increase your risk of endometrial cancer, breast cancer, or uterine cancer. Talk with your doctor about this risk. Do not use this medicine if you have had your uterus (womb) removed (hysterectomy). Check with your doctor immediately if your experience abnormal vaginal bleeding.
Using this medicine may increase your risk of dementia, especially in women 65 years of age and older.
Check with your doctor immediately if severe headache or sudden loss of vision or any other change in vision occurs while you are using this medicine. Your doctor may want you to have your eyes checked by an ophthalmologist (eye doctor).
Make sure any doctor or dentist who treats you knows that you are using this medicine. You may need to stop using this medicine before you have surgery or if you need to stay in bed for an extended time. This medicine may affect the results of certain medical tests.
Do not take other medicines unless they have been discussed with your doctor. This includes prescription or nonprescription (over-the-counter [OTC]) medicines and herbal (eg, St. John's wort) or vitamin supplements.
Side Effects of Ortho-Est
Along with its needed effects, a medicine may cause some unwanted effects. Although not all of these side effects may occur, if they do occur they may need medical attention.
Check with your doctor immediately if any of the following side effects occur:
Incidence not known
- Acid or sour stomach
- anxiety
- backache
- belching
- breast discharge, swelling, or pain
- change in vaginal discharge
- changes in skin color, pain, tenderness
- chest pain or discomfort
- chills
- clay-colored stools
- confusion
- constipation
- cough
- cramps
- darkened urine
- diarrhea
- difficulty speaking
- difficulty swallowing
- dizziness or lightheadedness
- double vision
- fainting
- fast heartbeat
- fever
- full or bloated feeling or pressure in the stomach
- headache
- heartburn
- heavy bleeding
- hives, itching, skin rash
- inability to move the arms, legs, or facial muscles
- inability to speak
- indigestion
- itching of the vagina or outside genitals
- loss of appetite
- nausea
- pain during sexual intercourse
- pain or discomfort in the arms, jaw, back, or neck
- pain or feeling of pressure in the pelvis
- pains in stomach, side, or abdomen, possibly radiating to the back
- puffiness or swelling of the eyelids or around the eyes, face, lips, or tongue
- slow speech
- stomach discomfort, upset, or pain
- sudden shortness of breath or troubled breathing
- sweating
- swelling of the abdominal or stomach area
- tightness in the chest
- unpleasant breath odor
- unusual tiredness or weakness
- unusually heavy or unexpected menstrual bleeding
- vaginal yeast infection
- vaginal bleeding or spotting
- vomiting
- vomiting of blood
- yellow eyes or skin
Some side effects may occur that usually do not need medical attention. These side effects may go away during treatment as your body adjusts to the medicine. Also, your health care professional may be able to tell you about ways to prevent or reduce some of these side effects. Check with your health care professional if any of the following side effects continue or are bothersome or if you have any questions about them:
Incidence not known
- Hair loss
- inability to have or keep an erection
- increased hair growth, especially on the face
- loss in sexual ability, desire, drive, or performance
- patchy brown or dark brown discoloration of the skin
- swelling of the breasts or breast soreness in males
- trouble wearing contact lenses
- weight gain or loss
Other side effects not listed may also occur in some patients. If you notice any other effects, check with your healthcare professional.
Call your doctor for medical advice about side effects. You may report side effects to the FDA at 1-800-FDA-1088.
Related/similar drugs
Commonly used brand name(s)
In the U.S.
- Ogen .625
- Ogen 1.25
- Ogen 2.5
- Ortho-Est
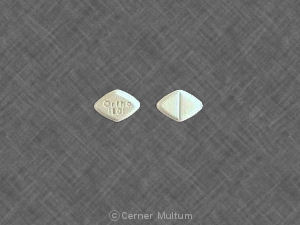
Available Dosage Forms:
- Tablet
Therapeutic Class: Endocrine-Metabolic Agent
Pharmacologic Class: Estrogen
More about Ortho-Est (estropipate)
- Check interactions
- Compare alternatives
- Drug images
- Side effects
- Dosage information
- During pregnancy
- Drug class: estrogens
Patient resources
Other brands
Professional resources
Other brands
Related treatment guides
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.