Disopyramide (Monograph)
Brand names: Norpace, Norpace CR
Drug class: Class Ia Antiarrhythmics
VA class: CV300
CAS number: 22059-60-5
Warning
- Mortality
-
Excessive mortality or nonfatal cardiac arrest rate (7.7%) in encainide- or flecainide-treated patients with asymptomatic non-life-threatening ventricular arrhythmias (with MI history >6 days but <2 years) in NHLBI’s long-term CAST study relative to placebo. (See Mortality under Cautions.)
-
Applicability of CAST findings to other populations (e.g., those without recent MI) uncertain.
-
Because of disopyramide’s proarrhythmic properties and lack of evidence of improved survival for any antiarrhythmic drug, reserve disopyramide for life-threatening ventricular arrhythmias.
Introduction
Antiarrhythmic agent (class IA).
Uses for Disopyramide
Precise role in antiarrhythmic therapy has not been established. Some experts recommend that disopyramide be reserved for use as an alternative drug when lidocaine, quinidine, or procainamide is ineffective or adverse effects of these drugs are intolerable.
Limited information is available on combination therapy with other antiarrhythmic drugs such as lidocaine, quinidine, or procainamide to treat or prevent serious, refractory arrhythmias.
Ventricular Arrhythmias
Suppression and prevention of recurrent life-threatening ventricular arrhythmias (e.g., sustained VT). (See Boxed Warning.)
Because of disopyramide’s arrhythmogenic potential and lack of evidence for improved survival for class I antiarrhythmic agents, use for less severe arrhythmias is not recommended.
Avoid treatment of asymptomatic VPCs.
Atrial Arrhythmias
Has been used to convert atrial fibrillation, atrial flutter, and paroxysmal atrial tachycardia† [off-label] to normal sinus rhythm. However, other antiarrhythmic drugs (e.g., dofetilide, flecainide, ibutilide, propafenone, amiodarone) are preferred.
Disopyramide Dosage and Administration
General
-
Adjust dosage carefully according to individual requirements and response and the general condition and cardiovascular status of the patient.
-
Initiate disopyramide therapy only in a hospital setting.
-
ECG monitoring of cardiac function and determination of plasma concentrations are recommended, especially when given to patients with an increased risk of adverse reactions (e.g., those with severe heart disease, hypertension, hepatic or renal disease).
Administration
Administer orally.
Oral Administration
Conventional capsules: Administer orally every 6 hours or at intervals according to individual requirements.
Extended-release capsules: Administer orally every 12 hours.
For rapid control of ventricular arrhythmias, conventional capsules should be used; do not use extended-release capsules.
Dosage
Available as disopyramide phosphate; dosage expressed in terms of disopyramide.
Reduce dosage in patients with moderate or severe renal insufficiency, hepatic insufficiency, cardiomyopathy, possible cardiac decompensation, AMI, and in patients weighing <50 kg.
Pediatric Patients
Ventricular Arrhythmias
Oral
Optimum pediatric dosage has not been established; however, dosage recommendations have been made based on clinical experience.
Initiate dose titration at the lower end of the recommended ranges; monitor plasma drug concentrations and therapeutic response carefully.
For children unable to swallow the capsules, a suspension may be extemporaneously prepared by mixing the contents of disopyramide phosphate conventional capsules in cherry syrup to produce suspensions that contain 1–10 mg of disopyramide per mL. The extended-release capsules should not be used for the preparation of an extemporaneous suspension.
Give total daily dose in equally divided doses every 6 hours or at intervals according to individual requirements.
|
Age |
Total Daily Pediatric Dosage |
|---|---|
|
<1 year of age |
10–30 mg/kg |
|
1–4 years of age |
10–20 mg/kg |
|
4–12 years of age |
10–15 mg/kg |
|
12–18 years of age |
6–15 mg/kg |
Adults
Ventricular Arrhythmias
Oral (Conventional Capsules)
Usual dosage: 400–800 mg daily, given in divided doses.
Adults weighing ≥50 kg: Usually 150 mg every 6 hours.
Adults weighing <50 kg: Usually 100 mg every 6 hours.
Oral (Extended-release Capsules)
Usual dosage: 400–800 mg daily, given in divided doses.
Adults weighing ≥50 kg: Usually 300 mg every 12 hours.
Adults weighing <50 kg: Usually 200 mg every 12 hours.
Rapid Control
Oral (Conventional Capsules)Adults weighing ≥50 kg: Initially, 300 mg followed by 150 mg every 6 hours.
Adults weighing <50 kg: Initially, 200 mg followed by 150 mg every 6 hours.
If there is no therapeutic response and if no toxic effects occur within 6 hours after the initial 300-mg dose, 200-mg doses may be given every 6 hours. If there is no response to this dosage in 48 hours, discontinue disopyramide and initiate alternative therapy.
Alternatively, the patient may be hospitalized, closely evaluated, and continuously monitored while the dosage is increased to 250 or 300 mg every 6 hours.
Severe Refractory VT
Oral (Conventional Capsules)Up to 400 mg every 6 hours may be required (resulting in plasma disopyramide concentrations up to 9 mcg/mL).
Patients should be hospitalized, closely evaluated, and continuously monitored.
Rapid Control In Patients with Cardiomyopathy or Possible Cardiac Decompensation
Oral (Conventional Capsules)Do not administer an initial loading dose.
Do not exceed an initial dosage of 100 mg every 6 hours.
Carefully adjust dosage in these patients while closely monitoring for hypotension and/or CHF. (See CHF and Hypotension under Cautions.)
Switching from Another Class I Antiarrhythmic Agent
Oral (Conventional Capsules or Extended-release Capsules)Administer the usual dosage of disopyramide (without an initial loading dose) 6–12 hours after the last dose of quinidine sulfate or 3–6 hours after the last dose of procainamide.
If withdrawal of quinidine or procainamide is likely to produce life-threatening arrhythmias, hospitalize and closely monitor patient.
Switching from Conventional to Extended-release Capsules
Oral (Extended-release)Initiate usual maintenance schedule (e.g., 300 mg every 12 hours) of extended-release capsules 6 hours after the last dose of the conventional capsules.
Dosage Modification for Toxicity
If increased anticholinergic adverse effects occur, monitor plasma concentrations of disopyramide and adjust dosage accordingly. Dosage may be reduced by one-third and the same dosing interval maintained (e.g., 600 mg daily reduced to 400 mg daily).
Prescribing Limits
Adults
Ventricular Arrhythmias
Patients with Cardiomyopathy or Possible Cardiac Decompensation
Oral (Conventional Capsules)Maximum initial dosage: 100 mg every 6 hours.
Special Populations
Hepatic Impairment
Oral
Usual dosage: 100 mg every 6 hours as conventional capsules or 200 mg every 12 hours as extended-release capsules.
Renal Impairment
Oral
Do not use extended-release capsules in patients with a Clcr ≤40 mL/minute.
Patients with moderately impaired renal function (Clcr >40 mL/minute): Usually, 100 mg every 6 hours as conventional capsules or 200 mg every 12 hours as extended-release capsules.
In patients with severely impaired renal function (Clcr ≤40 mL/minute), the usual dosage of conventional capsules is 100 mg (with or without an initial 150-mg dose) given at the following approximate intervals depending on the patient’s Clcr:
|
Clcr (mL/minute) |
Dosage Interval |
|---|---|
|
30–40 |
every 8 h |
|
15–30 |
every 12 h |
|
<15 |
every 24 h |
Geriatric Patients
Select dosage with caution (generally starting at the low end of the dosing range) because of age-related decreases in hepatic, renal, and/or cardiac function, and concomitant disease and drug therapy.
If adverse anticholinergic effects occur, monitor plasma disopyramide concentrations and adjust dosage as needed. (See Dosage Modification for Toxicity under Dosage and Administration.)
Cautions for Disopyramide
Contraindications
-
Preexisting 2nd or 3rd degree AV block (if an artificial pacemaker has not been inserted).
-
Cardiogenic shock.
-
Known hypersensitivity to disopyramide.
Warnings/Precautions
Warnings
Mortality
In CAST study, excessive rate of mortality and nonfatal cardiac arrest reported in patients with asymptomatic, non-life-threatening ventricular arrhythmias and recent MI (>6 days but <2 years previously) who were receiving encainide or flecainide compared with placebo.
Because of disopyramide’s arrhythmogenic potential and the lack of evidence for improved survival for class I antiarrhythmic agents, use disopyramide only for life-threatening arrhythmias. Use in less severe arrhythmias currently is not recommended, and treatment of asymptomatic VPCs should be avoided.
Initiate therapy only in a hospital setting.
CHF and Hypotension
May cause or worsen CHF or produce severe hypotension. Hypotension occurs more commonly in patients with primary cardiomyopathy or inadequately compensated CHF.
Do not use in patients with uncompensated or marginally compensated CHF or hypotension unless the CHF or hypotension is secondary to cardiac arrhythmia. In patients with a history of heart failure, cardiac function must be carefully maintained, including optimal digitalization.
If hypotension occurs or CHF worsens, discontinue disopyramide and, if necessary, resume therapy at a lower dosage only after establishing adequate cardiac compensation.
Increased risk of severe hypotension in patients with myocarditis or other cardiomyopathy. Do not administer a loading dose to such patients; select initial dosage and make subsequent dosage adjustments under close supervision. (See Patients with Cardiomyopathy or Possible Cardiac Decompensation under Dosage and Administration.)
Arrhythmogenic Effects
Possible worsening of existing arrhythmias or occurrence of new arrhythmias, including VT and VF associated with prolonged QT interval. Increased risk of such effects if used concomitantly with other drugs (i.e., quinidine) that prolong the QT interval.
If a QT prolongation >25% occurs and if ectopy continues, monitor patient closely. Consider discontinuance of disopyramide.
Hypoglycemia
Hypoglycemia reported rarely.
Monitor blood glucose concentrations closely in patients with compromised glucoregulatory mechanisms in the absence of food (e.g., patients with CHF, chronic malnutrition, hepatic or renal disease, those using alcohol or receiving certain drugs [e.g., β-adrenergic blockers]).
Concurrent Use with Other Antiarrhythmics
Reserve combined use for serious arrhythmias unresponsive to monotherapy; monitor closely.
Heart Block
Reduce dosage if first-degree AV heart block occurs. If the block persists, weigh the benefit of therapy against the potential risk of higher degrees of AV block.
If second- or third-degree AV block or unifascicular, bifascicular, or trifascicular block occurs, discontinue disopyramide therapy, unless the ventricular rate is adequately controlled by an artificial pacemaker.
Anticholinergic Effects
Possible anticholinergic effects; do not use in patients with glaucoma, myasthenia gravis, or urinary retention without instituting adequate overriding measures (e.g., pilocarpine ophthalmic drops for glaucoma, catheter drainage or operative relief for urinary retention).
Possible increased risk of urinary retention in males with benign prostatic hypertrophy.
Measure intraocular pressure before initiating therapy in patients with a family history of glaucoma.
May precipitate myasthenic crisis; use with caution in patients with myasthenia gravis.
Use with caution in geriatric patients. (See Geriatric Use under Cautions.)
General Precautions
Atrial Tachyarrhythmias
Possible enhanced AV conduction; patients with atrial flutter or fibrillation should be digitalized prior to administration.
Conduction Abnormalities
Use with caution in patients with sick sinus syndrome (including bradycardia-tachycardia syndrome), Wolff-Parkinson-White syndrome, or bundle-branch block, since effects of the drug in these conditions are unpredictable.
Potassium Imbalance
Correct abnormalities in serum potassium concentration before initiating therapy.
May be ineffective in patients with hypokalemia and toxic effects may be enhanced in patients with hyperkalemia.
Specific Populations
Pregnancy
Category C.
Lactation
Distributed into milk. Discontinue nursing or the drug.
Pediatric Use
Safety and efficacy not established. However, disopyramide has been used in children. (See Pediatric Patients under Dosage and Administration.)
Geriatric Use
Insufficient experience in patients ≥65 years of age to determine whether geriatric patients respond differently than younger adults.
Select dosage with caution because of age-related decreases in hepatic, renal, and/or cardiac function and potential for concomitant disease and drug therapy. (See Geriatric Patients under Dosage and Administration.)
Substantially eliminated by kidneys; assess renal function periodically and adjust dosage accordingly. (See Renal Impairment under Dosage and Administration.)
Possible anticholinergic effects; not generally recommended for use in patients with glaucoma, urinary retention, or benign prostatic hypertrophy unless adequate overriding measures are taken. (See Anticholinergic Effects under Warnings.)
Hepatic Impairment
Increased plasma half-life; dosage adjustment recommended. (See Hepatic Impairment under Dosage and Administration.)
Patients with cardiac dysfunction are more likely to have comorbid hepatic impairment.
Carefully monitor ECG for prolongation of PR interval, evidence of QRS widening, or other signs of toxicity.
Renal Impairment
Increased plasma half-life; dosage adjustments necessary based on degree of renal impairment. (See Renal Impairment under Dosage and Administration.)
Carefully monitor ECG for prolongation of PR interval, evidence of QRS widening, or other signs of toxicity.
Not recommended for use in patients with severe renal insufficiency (Clcr ≤40 mL/min).
Common Adverse Effects
Anticholinergic effects (e.g., dry mouth, urinary hesitancy, constipation, blurred vision, dry nose/eyes/throat), urinary frequency/urgency, urinary retention, nausea, pain/bloating/gas, dizziness, general fatigue/muscle weakness, headache, malaise, aches/pains.
Appears to be metabolized principally by CYP3A4.
Drugs Affecting Hepatic Microsomal Enzymes
Inducers of hepatic microsomal enzymes: Potential pharmacokinetic interaction (decreased plasma disopyramide concentrations). When used concomitantly, closely monitor serum disopyramide concentrations to avoid subtherapeutic concentrations.
Inhibitors of CYP3A4: Potential pharmacokinetic interaction (increased plasma disopyramide concentrations).
Specific Drugs
|
Drug |
Interaction |
Comments |
|---|---|---|
|
Antiarrhythmic agents (e.g., quinidine, procainamide, lidocaine, encainide, flecainide, propafenone, propranolol) |
Possible additive or antagonistic cardiac effects; toxic effects may be additive Potential for severe negative inotropic effects or enhanced conduction prolongation, especially in cardiac decompensation Concomitant use with quinidine may result in slight increases in plasma disopyramide concentrations and slight decreases in plasma quinidine concentrations |
Reserve concomitant use for the management of life-threatening arrhythmias unresponsive to monotherapy; monitor closely |
|
Anticholinergic agents |
Possible additive effects |
|
|
Diazepam |
No interaction noted in healthy individuals |
|
|
Digoxin |
Concomitant use does not appear to increase serum digoxin concentrations |
|
|
Macrolide antibiotics (e.g., erythromycin, clarithromycin) |
Increased plasma disopyramide concentrations and increased risk of serious toxicity (e.g., prolongation of the QT-interval, widening of the QRS complex, polymorphic ventricular tachycardia, ventricular fibrillation) |
Close monitoring recommended |
|
Phenytoin |
Potential for increased metabolism of disopyramide |
Monitor serum disopyramide concentrations closely to avoid subtherapeutic concentrations |
|
Verapamil |
Potential for additive negative inotropic effects |
Concomitant use not recommended Discontinue disopyramide 48 hours prior to initiating verapamil therapy; do not reinstitute disopyramide until 24 hours after verapamil has been discontinued |
Disopyramide Pharmacokinetics
Absorption
Bioavailability
Rapidly absorbed (60–83%) after oral administration.
Bioavailability of disopyramide from the extended-release and conventional capsules appears similar.
Peak plasma concentrations attained in 2–2.5 or 4.9 hours after oral administration of conventional or extended-release capsules, respectively.
Onset
Onset of action usually is within 0.5–3 hours after oral administration of a single 300-mg dose (conventional capsules).
Duration
Antiarrhythmic effect persists 1.5–8.5 hours after oral administration of conventional capsules.
Plasma Concentrations
Plasma disopyramide concentrations of approximately 2–4 mcg/mL generally required to suppress ventricular arrhythmias; concentrations up to 9 mcg/mL have been required in a limited number of patients with severe refractory VT.
Plasma concentrations >9 mcg/mL associated with toxic effects.
Distribution
Extent
Distributed throughout the extracellular body water; not extensively bound to tissues.
Equally distributed between plasma and erythrocytes.
Disopyramide crosses the placenta and is distributed into milk.
Plasma Protein Binding
Approximately 50–65%; decreases as the concentration of disopyramide and its metabolites increase.
Special Populations
In patients with renal insufficiency, the volume of distribution is slightly decreased.
Patients with AMI (without CHF) may have lower peak plasma concentrations and smaller volumes of distribution compared with healthy individuals.
Elimination
Metabolism
Metabolized in the liver to an N-monodealkylated metabolite and other unidentified metabolites.
Plasma concentration of the N-monodealkylated metabolite is approximately 10% of the concentration of disopyramide.
The N-monodealkylated metabolite has less antiarrhythmic activity but greater anticholinergic activity than does disopyramide.
CYP3A4 involved in metabolism.
Elimination Route
After oral administration, 50% of an oral dose excreted in urine as unchanged drug, 20% as the N-monodealkylated metabolite, and about 10% as unidentified metabolites; about 10% is excreted in feces as unchanged drug and metabolites.
Urinary pH apparently does not affect the rate of renal excretion.
Half-life
Conventional capsules: Elimination half-life 4–10 hours.
Extended-release capsules: Elimination half-life 6.9–16.4 hours.
Special Populations
Plasma half-life prolonged in patients with hepatic or renal insufficiency.
In patients with Clcr <40 mL/minute, plasma half-life ranged from 8–18 hours.
Disopyramide is removed by hemodialysis.
In patients with heart disease, including left ventricular dysfunction, the mean plasma half-life was slightly prolonged to 7.8 hours (range: 5–9.5 hours).
Stability
Storage
Oral
Capsules (Conventional and Extended-release)
25°C (may be exposed to 15–30°C).
Suspension
Oral suspensions of disopyramide phosphate prepared extemporaneously from conventional capsules of the drug and cherry syrup at concentrations ranging from 1–10 mg/mL reportedly are stable for 1 month when stored at 2–8°C.
Dispense in amber glass bottles.
Actions
-
A class I (membrane-stabilizing) antiarrhythmic agent with actions similar to those of procainamide and quinidine.
-
Regarded as a myocardial depressant because it decreases myocardial excitability and conduction velocity, and may depress myocardial contractility.
-
Possesses anticholinergic properties, which may modify the direct myocardial effects of the drug.
-
Exact mechanism of antiarrhythmic action has not been established; is believed to combine with fast sodium channels in their inactive state and thereby inhibit recovery after repolarization in a time- and voltage-dependent manner that is associated with subsequent dissociation of the drug from the sodium channels.
-
Exhibits electrophysiologic effects characteristic of class IA antiarrhythmic agents (i.e., exhibits intermediate rates of attachment and dissociation transmembrane sodium channels).
-
Suppresses automaticity in the His-Purkinje system.
-
Decreases the automaticity of ectopic atrial and ventricular pacemakers, shortens or does not change the sinus node recovery time, and decreases conduction velocity in the atria and ventricles.
-
Has little effect on conduction velocity through the AV node or the His-Purkinje system, but accessory pathway conduction velocity is decreased.
-
Generally prolongs the effective refractory period (ERP) of the atria and the ventricles.
-
Usually has little effect on the ERP of the AV node or the His-Purkinje system; however, the effect on the AV node is unpredictable in patients with preexisting conduction disturbances.
-
Generally causes little or no prolongation of the PR interval or the QRS complex, but the QT interval or QT interval corrected for rate (QTc) may be prolonged.
-
Generally has little effect on resting sinus rate and has a direct negative inotropic effect on the heart.
-
Usually decreases cardiac output 10–15% in patients without compromised myocardial function.
-
It has not been established whether disopyramide has local anesthetic properties.
Advice to Patients
-
Potential for toxicity (e.g., cardiovascular, anticholinergic).
-
Importance of women informing their clinician if they are or plan to become pregnant or plan to breast-feed.
-
Importance of informing clinicians of existing or contemplated concomitant therapy, including prescription and OTC drugs, as well as concomitant illnesses.
-
Importance of informing patients of other important precautionary information. (See Cautions.)
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
* available from one or more manufacturer, distributor, and/or repackager by generic (nonproprietary) name
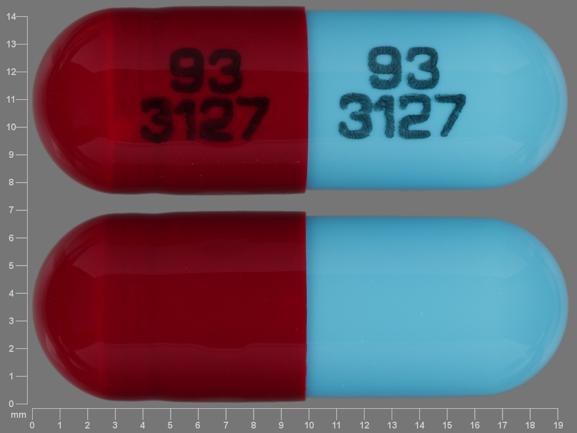
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Capsules |
100 mg (of disopyramide)* |
Disopyramide Phosphate Capsules |
|
|
Norpace |
Searle |
|||
|
150 mg (of disopyramide)* |
Disopyramide Phosphate Capsules |
|||
|
Norpace |
Searle |
|||
|
Capsules, extended-release |
100 mg (of disopyramide)* |
Disopyramide Phosphate Extended-Release Capsules |
Ethex |
|
|
Norpace CR |
||||
|
150 mg (of disopyramide)* |
Disopyramide Phosphate Extended-release Capsules |
Ethex |
||
|
Norpace CR |
AHFS DI Essentials™. © Copyright 2025, Selected Revisions November 4, 2016. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
† Off-label: Use is not currently included in the labeling approved by the US Food and Drug Administration.
Reload page with references included
Related/similar drugs
More about disopyramide
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (7)
- Drug images
- Side effects
- Dosage information
- During pregnancy
- Drug class: group I antiarrhythmics
- Breastfeeding
- En español