Adalimumab (Monograph)
Drug class: Tumor Necrosis Factor Inhibitors, Miscellaneous
Warning
- Serious Infections
-
Increased risk of serious infections involving various organ systems and sites that may require hospitalization or result in death; tuberculosis (frequently disseminated or extrapulmonary), invasive fungal infections (may be disseminated), bacterial (e.g., legionellosis, listeriosis) and viral infections, and other opportunistic infections reported.
-
Carefully consider risks and benefits prior to initiating adalimumab therapy in patients with chronic or recurring infections.
-
Evaluate patients for latent tuberculosis infection prior to and periodically during adalimumab therapy; if indicated, initiate appropriate antimycobacterial regimen prior to initiating adalimumab therapy.
-
Closely monitor patients for infection, including active tuberculosis in those with a negative tuberculin skin test, during and after treatment. Discontinue adalimumab if serious infection or sepsis occurs. Consider empiric antifungal therapy if serious systemic illness occurs in a patient at risk for invasive fungal infections.
- Malignancy
-
Lymphoma and other malignancies (some fatal) reported in children and adolescents receiving tumor necrosis factor (TNF) blocking agents.
-
Aggressive, usually fatal hepatosplenic T-cell lymphoma reported mainly in adolescents and young adults with Crohn disease or ulcerative colitis receiving TNF blocking agents, including adalimumab. Most of the patients received a combination of immunosuppressive agents, including TNF blocking agents and thiopurine analogs (azathioprine or mercaptopurine).
Introduction
Tumor necrosis factor (TNF) inhibitor and biologic disease-modifying antirheumatic drug (DMARD); a recombinant DNA-derived human immunoglobulin G1 (IgG1) monoclonal antibody.
Adalimumab-aacf (Idacio), adalimumab-aaty (Yuflyma), adalimumab-adaz (Hyrimoz), adalimumab-adbm (Cyltezo), adalimumab-afzb (Abrilada), adalimumab-aqvh (Yusimry), adalimumab-atto (Amjevita), adalimumab-bwwd (Hadlima), adalimumab-fkjp (Hulio), and adalimumab-ryvk (Simlandi) are biosimilar to adalimumab (Humira).
A biosimilar is a biological that is highly similar to an FDA-licensed reference biological with the exception of minor differences in clinically inactive components and for which there are no clinically meaningful differences in safety, purity, or potency. Biosimilars are approved through an abbreviated licensure pathway that establishes biosimilarity between proposed biological and reference biological but does not independently establish safety and effectiveness of the proposed biological. In order to be considered an interchangeable biosimilar, a biological product must meet additional requirements beyond demonstrating biosimilarity to its reference product. Adalimumab-aaty (Yuflyma), adalimumab-afzb (Abrilada), adalimumab-atto (Amjevita), adalimumab-adbm (Cyltezo), adalimumab-bwwd (Hadlima), adalimumab-adaz (Hyrimoz), adalimumab-fkjp (Hulio), and adalimumab-ryvk (Simlandi) are designated as interchangeable with adalimumab (Humira) at this time.
In this monograph, unless otherwise stated, the term “adalimumab products” refers to adalimumab (the reference drug) and its biosimilars (adalimumab-aacf, adalimumab-aaty, adalimumab-adaz, adalimumab-adbm, adalimumab-afzb, adalimumab-aqvh, adalimumab-atto, adalimumab-bwwd, adalimumab-fkjp, adalimumab-ryvk).
Uses for Adalimumab
Several adalimumab biosimilars are available. Biosimilarity of these products has been demonstrated for the indications described in Table 1.
|
FDA labeled indication |
RA |
JIA |
PsA |
AS |
CD (Adult and Pediatric) |
UC |
Ps |
HS |
UV |
|---|---|---|---|---|---|---|---|---|---|
|
Adalimumab-afzb (Abrilada) |
X |
X |
X |
X |
X |
X |
X |
X |
X |
|
Adalimumab-atto (Amjevita) |
X |
X |
X |
X |
X |
X |
X |
X |
X |
|
Adalimumab-adbm (Cyltezo) |
X |
X |
X |
X |
X |
X |
X |
X |
X |
|
Adalimumab-bwwd (Hadlima) |
X |
X |
X |
X |
X |
X |
X |
X |
X |
|
Adalimumab-fkjp (Hulio) |
X |
X |
X |
X |
X |
X |
X |
X |
X |
|
Adalimumab-adaz (Hyrimoz) |
X |
X |
X |
X |
X |
X |
X |
X |
X |
|
Adalimumab-aacf (Idacio) |
X |
X |
X |
X |
X |
X |
X |
X |
X |
|
Adalimumab-ryvk (Simlandi) |
X |
X |
X |
X |
X |
X |
X |
X |
X |
|
Adalimumab-aaty (Yuflyma) |
X |
X |
X |
X |
X |
X |
X |
X |
X |
|
Adalimumab-aqvh (Yusimry) |
X |
X |
X |
X |
X |
X |
X |
X |
X |
Originator adalimumab is labeled for use in adults and pediatric patients ≥5 years of age with UC; biosimilars are only labeled for use in adults with UC.
Originator adalimumab is labeled for use in adults and pediatric patients ≥12 years of age with HS; biosimilars are only labeled for use in adults with HS.
Originator adalimumab is labeled for use in adults and pediatric patients ≥2 years of age with UV; biosimilars are only labeled for use in adults with UV.
AS, ankylosing spondylitis; CD, Crohn disease; HS, hidradenitis suppurativa; JIA, juvenile idiopathic arthritis; Ps, plaque psoriasis; PsA, psoriatic arthritis; RA, rheumatoid arthritis; UC, ulcerative colitis ; UV, uveitis.
Rheumatoid Arthritis
Used to manage the signs and symptoms of rheumatoid arthritis, to induce a major clinical response, to improve physical function, and to inhibit progression of structural damage in adults with moderate to severe disease. Use alone or in combination with methotrexate or other nonbiologic disease-modifying antirheumatic drugs (DMARDs).
Disease-modifying treatments for rheumatoid arthritis include conventional DMARDs (e.g., hydroxychloroquine, leflunomide, methotrexate, sulfasalazine), biologic DMARDs (e.g., TNF blocking agents, abatacept, tocilizumab, sarilumab, rituximab), and/or targeted synthetic DMARDs (e.g., Janus kinase [JAK] inhibitors).
Guidelines generally support use of TNF blocking agents as add-on therapy to methotrexate in patients who do not meet treatment goals with methotrexate alone.
Specific agents for rheumatoid arthritis are selected according to current disease activity, prior therapies used, and presence of comorbidities.
Juvenile Idiopathic Arthritis
Used to manage signs and symptoms of moderately to severely active polyarticular juvenile idiopathic arthritis in pediatric patients ≥2 years of age. Use with or without methotrexate.
Drugs used to treat juvenile idiopathic arthritis include nonsteroidal antiinflammatory agents (NSAIAs), systemic and intra-articular corticosteroids, conventional DMARDs (e.g., methotrexate, sulfasalazine, hydroxychloroquine, leflunomide), and biologic DMARDs (e.g., TNF blocking agents, abatacept, tocilizumab, rituximab).
Guidelines generally support use of TNF blocking agents, as add-on therapy in patients with moderate to high disease activity despite the use of methotrexate.
Specific agents for juvenile idiopathic arthritis treatment are selected according to presence of certain risk factors (e.g., positive anti-cyclic citrullinated peptide antibodies, positive rheumatoid factor, joint damage), level of disease activity, involvement of specific joints, presence of certain comorbidities (e.g., uveitis), and prior therapies.
Psoriatic Arthritis
Used to manage the signs and symptoms of active psoriatic arthritis, to improve physical function and to inhibit progression of structural damage in adults. Use alone or in combination with other nonbiologic DMARDs.
Disease-modifying treatments for psoriatic arthritis include oral small molecules (OSMs; e.g., methotrexate, sulfasalazine, cyclosporine, leflunomide, apremilast), biologic DMARDs (e.g., TNF blocking agents, secukinumab, ixekizumab, ustekinumab, brodalumab, abatacept), and/or targeted synthetic DMARDs (e.g., tofacitinib).
Guidelines generally support use of TNF blocking agents as first-line treatment in patients with active psoriatic arthritis.
Recommendations for the use and selection of disease-modifying therapies in psoriatic arthritis vary based on the presence of certain disease characteristics (e.g., psoriatic spondylitis/axial disease, enthesitis) and comorbidities (e.g., inflammatory bowel disease, diabetes).
Ankylosing Spondylitis
Used to manage the signs and symptoms of active ankylosing spondylitis in adults.
Treatments for ankylosing spondylitis include NSAIAs, conventional DMARDs (e.g., methotrexate, sulfasalazine), biologic DMARDs (e.g., TNF blocking agents, secukinumab, ixekizumab), and/or targeted synthetic DMARDs (e.g., tofacitinib).
Guidelines generally support use of TNF blocking agents for treatment of ankylosing spondylitis in patients with active disease despite treatment with NSAIAs.
Recommendations for treatment selection in ankylosing spondylitis vary based on the presence of certain comorbidities (e.g., iritis, inflammatory bowel disease).
Crohn Disease
Used to treat moderately to severely active Crohn disease in adults and pediatric patients ≥6 years of age.
Guidelines generally support use of TNF blocking agents for use as induction and maintenance therapy in adults with moderate to severe Crohn disease. Specific treatments are selected according to the patient’s risk profile and disease severity.
Role of TNF blocking agents in pediatric Crohn disease is generally induction and maintenance therapy in patients who fail an adequate trial of steroids and exclusive enteral nutrition and/or immunomodulators, unless the patient has a complex perianal fistula at diagnosis.
Has been used in a limited number of patients with fistulizing Crohn disease† [off-label]. Has been used to prevent recurrence of Crohn disease after surgical treatment† [off-label], but place in therapy for this use remains to be determined.
Ulcerative Colitis
Used to treat moderately to severely active ulcerative colitis in adults and pediatric patients ≥5 years of age. Biosimilar products labeled for use in adults with moderately to severely active ulcerative colitis only.
Guidelines generally support first-line use of TNF blocking agents for induction and maintenance of remission in adults with moderate to severe ulcerative colitis. Specific treatments are selected according to disease severity, disease location/extent, disease prognosis, and previous therapies used.
Role of TNF blocking agents in pediatric ulcerative colitis is generally in patients with moderate to severe disease who fail therapy with 5-aminosalicylates/azathioprine and/or who are unable to wean from corticosteroids on 5-aminosalicylate/azathioprine therapy.
Efficacy in patients who have lost response to or were intolerant to TNF blocking agents not established.
Plaque Psoriasis
Used to manage moderate to severe chronic plaque psoriasis in adults who are candidates for systemic therapy or phototherapy and in whom other systemic therapies are medically less appropriate. Use only in patients who will be closely monitored and who will have regular follow-up visits with a clinician.
Guidelines generally support use of TNF blocking agents in moderate to severe psoriasis, either as monotherapy or in combination with topical, oral, or phototherapy.
Recommendations for use and selection of psoriasis therapies vary based on patient age, disease characteristics (e.g., severity, location, presence of psoriatic arthritis), and comorbidities (e.g., inflammatory bowel disease).
Hidradenitis Suppurativa
Used to manage moderate to severe hidradenitis suppurativa in adults and pediatric patients ≥12 years of age. Biosimilar products labeled for use in adults with moderate to severe hidradenitis suppurativa only.
Current guidelines recommend adalimumab to improve disease severity and quality of life in patients with moderate to severe hidradenitis suppurativa.
Uveitis
Management of noninfectious intermediate uveitis, posterior uveitis, and panuveitis in adults and pediatric patients ≥2 years of age. Biosimilar products labeled for use in adults with noninfectious intermediate uveitis, posterior uveitis, and panuveitis only.
Recommendations from an international expert panel support use of adalimumab in patients with noninfectious uveitis whose disease is inadequately controlled by corticosteroids and nonbiologic immunomodulatory therapies.
Adalimumab Dosage and Administration
General
Pretreatment Screening
-
Evaluate all patients for active and inactive tuberculosis prior to initiating therapy.
-
Screen at-risk patients for hepatitis B virus (HBV) infection before initiating therapy.
-
Do not initiate therapy in patients with an active infection, including clinically important localized infections.
-
Examine all patients for the presence of nonmelanoma skin cancer, particularly those with a medical history of prior prolonged immunosuppressant therapy or psoriasis patients with a history of psoralen and ultraviolet A radiation (PUVA) treatment.
Patient Monitoring
-
Monitor patients closely for signs or symptoms of infection during and after treatment; monitor for possible development of tuberculosis in patients who tested negative for latent tuberculosis prior to initiating therapy.
-
Perform periodic dermatologic evaluations in all patients, particularly those with a medical history of prior prolonged immunosuppressant therapy or psoriasis patients with a history of PUVA treatment.
-
Evaluate and monitor chronic carriers of HBV during treatment and for up to several months following treatment.
Dispensing and Administration Precautions
-
To avoid medication errors, the Institute for Safe Medication Practices (ISMP) recommends that prescribers communicate both the brand and generic names for adalimumab on the prescription order form.
-
Of the available adalimumab biosimilars, adalimumab-aaty (Yuflyma), adalimumab-afzb (Abrilada), adalimumab-atto (Amjevita), adalimumab-adbm (Cyltezo), adalimumab-bwwd (Hadlima), adalimumab-adaz (Hyrimoz), adalimumab-fkjp (Hulio) and adalimumab-ryvk (Simlandi) are designated as interchangeable with adalimumab (Humira).
-
Unbranded adalimumab products are also available under a manufacturer's approved Biologics License Application without the brand name on the label. FDA considers these products to be equivalent to the brand name biological products.
Other General Considerations
-
Methotrexate, other nonbiologic DMARDs, corticosteroids, NSAIAs, and/or analgesics may be continued in adults receiving adalimumab for the management of rheumatoid arthritis, psoriatic arthritis, or ankylosing spondylitis.
-
Methotrexate, corticosteroids, NSAIAs, and/or analgesics may be continued in pediatric patients receiving adalimumab for the management of juvenile idiopathic arthritis.
-
Aminosalicylates and/or corticosteroids may be continued in adults receiving adalimumab for the treatment of Crohn disease or ulcerative colitis. Azathioprine, mercaptopurine, or methotrexate may be continued, if necessary, in adults receiving adalimumab for the treatment of Crohn disease. Azathioprine and mercaptopurine may be continued, if necessary, in adults receiving adalimumab for the treatment of ulcerative colitis.
Administration
Sub-Q Injection
Administer by sub-Q injection.
Adalimumab products are available in various formulations including single-dose prefilled syringes, prefilled pens, autoinjectors, and vials for institutional use only; refer to the prescribing information of each individual product for further formulation information.
Various packaging configurations (e.g., starter packs) may be available; contact individual product manufacturers for more information. Some adalimumab products not available in presentations suitable for pediatric use, even if product is labeled for pediatric use; consult specific product information and manufacturer websites for details.
Adalimumab products contain no preservatives; discard any unused portions of solution.
Adalimumab products may sit outside of refrigeration for 15–30 minutes prior to administration to allow liquid to reach room temperature; do not remove cap or cover while the drug is warming to room temperature.
Administer sub-Q injections into anterior thighs or abdomen; do not administer abdominal injections within 5.18 cm (2 inches) of the umbilicus. Rotate injection sites. Administer new injections ≥2.54 cm (1 inch) from an old site; avoid injections into areas where the skin is tender, bruised, red, or hard, or into scars or stretch marks. Do not inject into psoriatic lesions.
Intended for use under the guidance and supervision of a clinician, but may be self-administered if the clinician determines that the patient and/or their caregiver is competent to safely administer the drug after appropriate training and with medical follow-up as necessary.
Dosage
Pediatric Patients
Juvenile Idiopathic Arthritis
Sub-Q
Pediatric patients ≥2 years of age weighing 10 to <15 kg: 10 mg once every other week.
Pediatric patients ≥2 years of age weighing 15 to <30 kg: 20 mg once every other week.
Pediatric patients ≥2 years of age weighing ≥30 kg: 40 mg once every other week.
Not studied for this use in patients <2 years of age or weighing <10 kg.
Crohn Disease
Sub-Q
Pediatric patients ≥6 years of age weighing 17 to <40 kg: 80 mg on day 1, followed by 40 mg once 2 weeks later (on day 15). Start maintenance dosage of 20 mg once every other week on day 29 (2 weeks after the 40-mg dose).
Pediatric patients ≥6 years of age weighing ≥40 kg: 160 mg on day 1 (given in one day or divided over 2 consecutive days), followed by 80 mg once 2 weeks later (on day 15). Start maintenance dosage of 40 mg once every other week on day 29 (2 weeks after the 80-mg dose).
Ulcerative Colitis
Sub-Q
Pediatric patients ≥5 years of age weighing 20 to <40 kg: 80 mg on day 1, followed by 40 mg once on day 8 (1 week after the 80-mg dose) and 40 mg once on day 15 (1 week after the first 40-mg dose). Start maintenance dosage of 40 mg once every other week or 20 mg once every week on day 29 (2 weeks after the second 40-mg dose).
Pediatric patients ≥5 years of age weighing ≥40 kg: 160 mg on day 1 (given in one day or divided over 2 consecutive days), followed by 80 mg once on day 8 (1 week after the 160-mg dose) and 80 mg once on day 15 (1 week after the first 80-mg dose). Start maintenance dosage of 80 mg once every other week or 40 mg once every week on day 29 (2 weeks after the second 80-mg dose).
Recommended pediatric dosage should be continued in patients who turn 18 years of age and who are well-controlled on their adalimumab regimen.
Biosimilars not labeled for use in pediatric patients with ulcerative colitis.
Hidradenitis Suppurativa
Sub-Q
Adolescents ≥12 years of age weighing 30 to <60 kg: 80 mg on day 1, followed by 40 mg once on day 8, then 40 mg once every other week.
Adolescents ≥12 years of age weighing ≥60 kg: 160 mg on day 1 (given in one day or divided over 2 consecutive days), followed by 80 mg once 2 weeks later (on day 15). Start dosage of 40 mg once every week or 80 mg once every other week on day 29 (2 weeks after the 80-mg dose).
Biosimilars not labeled for use in pediatric patients with hidradenitis suppurativa.
Uveitis
Sub-Q
Pediatric patients ≥2 years of age weighing 10 to <15 kg: 10 mg once every other week.
Pediatric patients ≥2 years of age weighing 15 to <30 kg: 20 mg once every other week.
Pediatric patients ≥2 years of age weighing ≥30 kg: 40 mg once every other week.
Not been studied for this use in patients <2 years of age or weighing <10 kg.
Biosimilars not labeled for use in pediatric patients with uveitis.
Adults
Rheumatoid Arthritis
Sub-Q
40 mg once every other week.
Patients not receiving methotrexate may obtain additional benefit from 40 mg once every week or 80 mg once every other week.
Psoriatic Arthritis
Sub-Q
40 mg once every other week.
Ankylosing Spondylitis
Sub-Q
40 mg once every other week.
Crohn Disease
Sub-Q
160 mg once on day 1 (given in one day or divided over 2 consecutive days), followed by 80 mg once 2 weeks later (on day 15). Start maintenance dosage of 40 mg once every other week on day 29 (2 weeks after the 80-mg dose).
Ulcerative Colitis
Sub-Q
160 mg on day 1 (given in one day or divided over 2 consecutive days), followed by 80 mg once 2 weeks later (on day 15). Start maintenance dosage of 40 mg once every other week on day 29 (2 weeks after the 80-mg dose). If clinical remission is not achieved by 8 weeks (day 57), discontinue adalimumab.
Plaque Psoriasis
Sub-Q
80 mg on day 1, followed by 40 mg once every other week (maintenance dosage) starting 1 week after the initial dose.
Hidradenitis Suppurativa
Sub-Q
160 mg on day 1 (given in one day or divided over 2 consecutive days), followed by 80 mg once 2 weeks later (on day 15). Start dosage of 40 mg once every week or 80 mg once every other week on day 29 (2 weeks after the 80-mg dose).
Uveitis
Sub-Q
80 mg on day 1, followed by 40 mg once every other week starting 1 week after the initial dose.
Special Populations
Hepatic Impairment
No dosage recommendations at this time.
Renal Impairment
No dosage recommendations at this time.
Geriatric Patients
No dosage recommendations at this time.
Cautions for Adalimumab
Contraindications
-
None.
Warnings/Precautions
Warnings
Serious Infections
Increased risk of serious infections involving various organ systems and sites that may require hospitalization or result in death. Opportunistic infections caused by bacterial, mycobacterial, invasive fungal, viral, parasitic, or other opportunistic pathogens (e.g., aspergillosis, blastomycosis, candidiasis, coccidioidomycosis, histoplasmosis, legionellosis, listeriosis, pneumocystosis, tuberculosis) reported, particularly in patients receiving concomitant therapy with immunosuppressive agents (e.g., methotrexate, corticosteroids). Infections frequently are disseminated. (See Boxed Warning.)
Increased incidence of serious infections observed with concomitant use of a TNF blocking agent and anakinra or abatacept. Use of adalimumab in combination with other biologic DMARDs, including abatacept and anakinra, not recommended.
Patients >65 years of age, with comorbid conditions, and/or receiving concomitant therapy with immunosuppressive agents (e.g., corticosteroids, methotrexate) may be at increased risk of infection.
Do not initiate adalimumab in patients with active infections, including localized infections. Consider potential risks and benefits of the drug prior to initiating therapy in patients with a history of chronic, recurring, or opportunistic infections; patients with underlying conditions that may predispose them to infections; and patients who have been exposed to tuberculosis or who have resided or traveled in regions where tuberculosis or mycoses such as histoplasmosis, coccidioidomycosis, and blastomycosis are endemic.
Closely monitor patients during and after adalimumab therapy for signs or symptoms of infection, including the possible development of tuberculosis in patients who tested negative for latent tuberculosis prior to initiating therapy.
If new infection occurs during therapy, perform thorough diagnostic evaluation (appropriate for immunocompromised patient), initiate appropriate anti-infective therapy, and closely monitor patient. Discontinue adalimumab if serious infection or sepsis develops.
Evaluate all patients for active or latent tuberculosis and for risk factors for tuberculosis prior to and periodically during therapy. When indicated, initiate appropriate antimycobacterial regimen for treatment of latent tuberculosis infection prior to adalimumab therapy. Also consider antimycobacterial therapy prior to adalimumab therapy for individuals with a history of latent or active tuberculosis in whom an adequate course of antimycobacterial treatment cannot be confirmed and for individuals with a negative tuberculin skin test who have risk factors for tuberculosis. Consultation with a tuberculosis specialist is recommended when deciding whether to initiate antimycobacterial therapy.
Monitor all patients, including those with negative tuberculin skin tests, for active tuberculosis. Strongly consider tuberculosis in patients who develop new infections while receiving adalimumab, especially if they previously have traveled to countries where tuberculosis is highly prevalent or have been in close contact with an individual with active tuberculosis.
Consider empiric antifungal therapy in patients at risk for invasive fungal infections who develop severe systemic illness. Whenever feasible, consider consulting a specialist in invasive fungal infections.
Malignancies
Cases of lymphoma and other malignancies (some fatal) reported in children, adolescents, and adults receiving TNF blocking agents; most patients received other immunosuppressive agents concomitantly. Malignancies included lymphomas and various other malignancies (e.g., leukemia, melanoma, solid organ cancers). (See Boxed Warning.)
Consider possibility of and monitor for occurrence of malignancies during and following treatment with TNF blocking agents.
Consider risks and benefits of TNF blocking agents prior to initiating therapy in patients with a known malignancy (other than successfully treated nonmelanoma skin cancer) or when deciding whether to continue therapy in patients who develop a malignancy. Carefully consider risks and benefits of these agents, especially in adolescents and young adults and especially in the treatment of Crohn disease or ulcerative colitis.
Examine all patients, but particularly those with a history of prior prolonged immunosuppressive therapy or a history of psoralen and UVA light (PUVA) therapy, for nonmelanoma skin cancer before and during adalimumab therapy.
Sensitivity Reactions
Hypersensitivity Reactions
Anaphylaxis, angioedema, and other allergic reactions (e.g., allergic rash, anaphylactoid reactions, fixed drug reaction, nonspecified drug reaction, urticaria) observed. If serious allergic reaction or anaphylaxis occurs, immediately discontinue adalimumab and initiate appropriate therapy.
Latex Sensitivity
Needle covers of certain packaging configurations of reference product adalimumab (injection pen and prefilled syringes containing 40 mg in 0.8 mL) may contain dry natural rubber (latex) and should not be handled by individuals sensitive to latex.
Needle caps of adalimumab-adbm (Cyltezo) injection pens and prefilled syringes also contain natural rubber latex.
Other Warnings/Precautions
HBV Reactivation
Increased risk of reactivation of HBV infection in patients who are chronic carriers of the virus (i.e., hepatitis B surface antigen-positive [HBsAg-positive]). Use of multiple immunosuppressive agents may contribute to HBV reactivation.
Screen at-risk patients prior to initiation of therapy. Evaluate and monitor HBV carriers before, during, and for up to several months after therapy. Safety and efficacy of antiviral therapy for prevention of HBV reactivation not established.
Discontinue adalimumab and initiate appropriate treatment (e.g., antiviral therapy) if HBV reactivation occurs. Not known whether adalimumab can be readministered once control of a reactivated HBV infection is achieved; caution advised in this situation.
Neurologic Reactions
New onset or exacerbation of central or peripheral nervous system demyelinating disorders (e.g., multiple sclerosis, optic neuritis, Guillain-Barré syndrome) reported rarely in patients receiving adalimumab or other TNF blocking agents.
Exercise caution when considering adalimumab therapy in patients with preexisting or recent-onset central or peripheral nervous system demyelinating disorders. Consider discontinuing adalimumab if any such disorders develop during therapy.
Intermediate uveitis is known to be associated with central demyelinating disorders.
Hematological Reactions
Possible pancytopenia (including aplastic anemia), leukopenia, or thrombocytopenia. Consider discontinuance in patients with confirmed hematologic abnormalities.
Heart Failure
Worsening heart failure and new-onset heart failure reported in patients receiving adalimumab or other TNF blocking agents. Use with caution and carefully monitor patients with heart failure.
Autoimmunity
Possible formation of autoimmune antibodies. Lupus-like syndrome reported. If manifestations suggestive of lupus-like syndrome develop, discontinue adalimumab.
Immunogenicity
Antibodies to adalimumab may develop. Long-term immunogenicity remains to be determined.
In adults with rheumatoid arthritis, incidence of antibodies to adalimumab is lower in patients receiving adalimumab with methotrexate compared with those receiving adalimumab monotherapy. Incidence also may be lower with weekly compared with every-other-week monotherapy. In patients receiving every-other-week monotherapy, clinical response achieved in fewer antibody-positive patients than antibody-negative patients.
In pediatric patients with juvenile idiopathic arthritis, incidence of antibodies to adalimumab is lower in those receiving adalimumab with methotrexate compared with those receiving adalimumab monotherapy.
In adults with noninfectious uveitis, no association observed between antibody development and adalimumab safety or efficacy.
In pediatric patients with ulcerative colitis, development of antibodies to adalimumab associated with reduced serum adalimumab concentrations; no association between antibody development and adalimumab safety observed. Association between antibody development and efficacy not assessed.
In patients with hidradenitis suppurativa, development of antibodies to adalimumab associated with reduced serum adalimumab concentrations (magnitude of reduction generally greater with increasing antibody titers); no apparent association between antibody development and adalimumab safety.
Immunization
Patients may receive inactivated vaccines. No data available on secondary transmission of infection by live vaccines in adalimumab-treated patients. Avoid live vaccines.
When considering adalimumab for pediatric patients, review vaccination status of child and administer all age-appropriate vaccines included in current immunization guidelines.
In utero exposure to adalimumab may affect immune response of infants. Consider risks and benefits of administering live vaccines to infants exposed to the drug in utero; safety of live vaccines in such infants is unknown.
Specific Populations
Pregnancy
Available studies do not reliably establish an association between adalimumab and major birth defects. In a pregnancy registry cohort study, a higher incidence of major birth defects observed in females exposed to adalimumab; however, methodologic limitations preclude definitive conclusions.
No fetal harm or malformations observed in animal studies.
Data suggest increased disease activity in females with rheumatoid arthritis or inflammatory bowel disease is associated with increased risk of adverse pregnancy outcomes (e.g., preterm delivery, low birth weight, small size for gestational age at birth).
As pregnancy progresses, monoclonal antibodies are increasingly transported across the placenta. Adalimumab is actively transferred across the placenta during the third trimester of pregnancy. Some data suggest adalimumab may be detectable in serum of infants exposed to the drug in utero for ≥3 months following birth.
In utero exposure to adalimumab may affect immune response of infants. Consider risks and benefits of administering live vaccines to infants exposed to the drug in utero; safety of live vaccines in such infants is unknown.
Lactation
Distributes into human milk in small amounts (0.1–1% of maternal serum concentrations); systemic exposure in nursing infants is likely to be low because drug is degraded in GI tract. However, effects of local GI tract exposure are unknown. No reports of adverse effects on breast-fed infants or effects on milk production.
Consider developmental and health benefits of breast-feeding along with the mother's clinical need for adalimumab and any potential adverse effects on the breast-fed child from the drug or from the underlying maternal condition.
Pediatric Use
Safety and efficacy for uses other than polyarticular juvenile idiopathic arthritis, Crohn disease, ulcerative colitis, and noninfectious uveitis not established in pediatric patients. Clinical trials in adults support use for management of hidradenitis suppurativa in adolescents. For marketing exclusivity reasons, adalimumab biosimilars are not labeled for use in pediatric patients with ulcerative colitis, hidradenitis suppurativa, or noninfectious uveitis.
Review vaccination status of the child and administer all age-appropriate vaccines, if possible, prior to initiation of adalimumab.
Geriatric Use
In geriatric patients with rheumatoid arthritis, no substantial differences in efficacy relative to younger adults.
The incidence of serious infection and malignancy in adalimumab-treated patients >65 years of age is higher than the incidence in younger adults. The overall incidence of infection and malignancy is higher in the geriatric population than in younger adults; consider risks and benefits of adalimumab in geriatric patients and closely monitor for development of infection or malignancy.
Hepatic Impairment
No pharmacokinetic data available.
Renal Impairment
No pharmacokinetic data available.
Common Adverse Effects
Common adverse effects (≥10%) include infections (e.g., upper respiratory, sinusitis), injection site reactions, headache, rash.
Drug Interactions
Administered concomitantly with aminosalicylates, methotrexate, other DMARDs, corticosteroids, other immunomodulatory agents (e.g., azathioprine, mercaptopurine), and/or NSAIAs in clinical studies.
Drugs Metabolized by Hepatic Microsomal Enzymes
Because increased levels of TNF during chronic inflammation may suppress formation of CYP isoenzymes, antagonism of TNF activity by adalimumab may normalize formation of CYP enzymes.
Drugs metabolized by CYP isoenzymes that have a low therapeutic index: Monitor therapeutic effect and/or serum concentrations following initiation or discontinuance of adalimumab; adjust dosage as needed.
Biologic Antirheumatic Agents
For other biologic agents used in the management of rheumatoid arthritis, psoriatic arthritis, ankylosing spondylitis, Crohn disease, ulcerative colitis, plaque psoriasis, noninfectious uveitis, or hidradenitis suppurativa, manufacturer states data regarding concomitant use with adalimumab are insufficient.
Concomitant use of adalimumab and other biologic DMARDs not recommended.
Vaccines
Patients may receive inactivated vaccines.
Avoid live vaccines. No data available on secondary transmission of infection by live vaccines in adalimumab-treated patients.
Specific Drugs
|
Drug |
Interaction |
Comments |
|---|---|---|
|
Abatacept |
Increased incidence of infection, without additional clinical benefit, reported with abatacept and TNF blocking agents in rheumatoid arthritis |
Concomitant use not recommended |
|
Anakinra |
Increased incidence of serious infections and neutropenia, without additional clinical benefit, reported with anakinra and another TNF blocking agent in rheumatoid arthritis |
Concomitant use not recommended |
|
Cyclosporine |
Possible effect on cyclosporine metabolism; increased levels of TNF during chronic inflammation may suppress formation of CYP isoenzymes, and adalimumab may antagonize this effect |
Monitor therapeutic effect and concentrations of cyclosporine following initiation or discontinuance of adalimumab; adjust dosage as needed |
|
Influenza virus vaccine inactivated |
Antibody titers in adalimumab-treated rheumatoid arthritis patients were protective, but titers to influenza antigens were moderately reduced |
|
|
Methotrexate |
Decreased adalimumab clearance |
Dosage adjustment not necessary |
|
Pneumococcal polysaccharide vaccine |
Concurrent use did not affect antibody response to vaccine |
|
|
Rituximab |
Increased risk of serious infection reported in patients who received rituximab and subsequently received a TNF blocking agent |
|
|
Theophylline |
Possible effect on theophylline metabolism; increased levels of TNF during chronic inflammation may suppress formation of CYP isoenzymes, and adalimumab may antagonize this effect |
Monitor therapeutic effect and serum concentrations of theophylline following initiation or discontinuance of adalimumab; adjust dosage as needed |
|
TNF blocking agents |
Concomitant use not recommended |
|
|
Warfarin |
Possible effect on warfarin metabolism; increased levels of TNF during chronic inflammation may suppress formation of CYP isoenzymes, and adalimumab may antagonize this effect |
Monitor therapeutic effect of warfarin following initiation or discontinuance of adalimumab; adjust dosage as needed |
Adalimumab Pharmacokinetics
Absorption
Bioavailability
Bioavailability is approximately 64%. Peak serum concentrations achieved in 131 hours.
Distribution
Extent
Distributed into synovial fluid.
Distributed into human milk in small amounts. Crosses placenta.
Elimination
Metabolism
Metabolic fate undetermined.
Elimination Route
Unknown.
Half-life
2 weeks (range: 10–20 days).
Special Populations
In patients with adalimumab antibodies, clearance of adalimumab is higher.
Clearance of adalimumab is lower with increasing age in patients 40 to >75 years of age.
Stability
Storage
Parenteral
Injection
Storage requirements for the adalimumab products vary dependent upon the individual product and/or formulation; refer to the prescribing information of each individual product for further information.
Actions
-
Potent antagonist of TNF biologic activity.
-
Has high specificity and affinity for TNF (TNF-α); does not bind to or inactivate lymphotoxin α (TNF-β). Prevents the binding of TNF to cell surface TNF receptors, thereby blocking the biologic activity of TNF.
-
Produced by recombinant DNA technology in a mammalian cell expression system; purified by a process that includes specific viral inactivation and removal steps.
Advice to Patients
-
Advise patients to read the manufacturer’s patient information (medication guide) prior to initiation of therapy and each time the prescription is refilled.
-
Instruct patients and/or caregivers regarding proper dosage and administration of adalimumab, including the use of aseptic technique, and proper disposal of needles, syringes, and used pens if it is determined that the patient and/or caregiver is competent to safely administer the drug.
-
Advise patients that if a dose is missed, the missed dose should be administered as soon as it is remembered and then the regular dosing schedule should be resumed.
-
Increased susceptibility to infection. Advise patients to seek immediate medical attention if signs and symptoms suggestive of infection (e.g., fever; fatigue; cough; warm, red, or painful skin; sores on the body; muscle aches; diarrhea; stomach pain; shortness of breath; weight loss; burning on urination; urinary frequency) develop.
-
Risk of lymphoma, including hepatosplenic T-cell lymphoma, leukemia, or other malignancies with use of TNF blocking agents. Counsel patients about the risk of malignancy with adalimumab. Advise patients to inform clinicians if signs and symptoms of malignancies (e.g., unexplained weight loss; fatigue; abdominal pain; persistent fever; night sweats; easy bruising or bleeding; swollen lymph nodes in the neck, underarm, or groin; hepatomegaly or splenomegaly) occur.
-
Advise patients to inform clinicians of any new or worsening medical conditions (e.g., neurologic conditions, heart failure, autoimmune disorders, psoriasis, cytopenias). Advise patients to report symptoms suggestive of cytopenias (e.g., bruising, bleeding, persistent fever).
-
Advise patients to alert their clinician if allergy to latex exists. Advise latex-sensitive patients that the needle cover or cap included in adalimumab-adbm (Cyltezo) and certain packaging configurations of reference product adalimumab (injection pens and prefilled syringes containing 40 mg in 0.8 mL) may contain natural rubber latex.
-
Advise patients to promptly contact a clinician if manifestations of an allergic reaction (e.g., urticaria, facial swelling, difficulty breathing) occur.
-
Advise patients to take the drug as prescribed and to not discontinue therapy without first consulting with a clinician.
-
Advise females to inform their clinicians if they are or plan to become pregnant or plan to breast-feed.
-
Advise patients to inform their clinicians of existing or contemplated concomitant therapy, including prescription and OTC drugs, as well as any concomitant illnesses or any history of cancer, tuberculosis, HBV infection, or other chronic or recurring infections.
-
Inform patients of other important precautionary information.
Additional Information
The American Society of Health-System Pharmacists, Inc. represents that the information provided in the accompanying monograph was formulated with a reasonable standard of care, and in conformity with professional standards in the field. Readers are advised that decisions regarding use of drugs are complex medical decisions requiring the independent, informed decision of an appropriate health care professional, and that the information contained in the monograph is provided for informational purposes only. The manufacturer’s labeling should be consulted for more detailed information. The American Society of Health-System Pharmacists, Inc. does not endorse or recommend the use of any drug. The information contained in the monograph is not a substitute for medical care.
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Parenteral |
Injection, for subcutaneous use |
10 mg/0.1 mL |
Humira (available as disposable prefilled syringes) |
AbbVie |
|
20 mg/0.2 mL |
Humira (available as disposable prefilled syringes ) |
AbbVie |
||
|
40 mg/0.4 mL |
Humira (available as disposable prefilled syringes and prefilled injection pens ) |
AbbVie |
||
|
40 mg/0.8 mL |
Humira (available as disposable prefilled syringes and prefilled injection pens ) |
AbbVie |
||
|
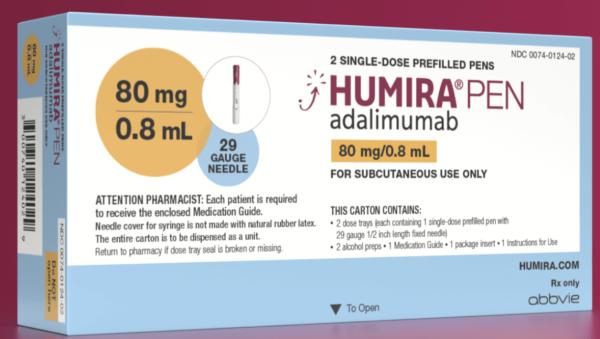
80 mg/0.8 mL |
Humira (available as disposable prefilled syringes and prefilled injection pens ) |
AbbVie |
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Parenteral |
Injection, for subcutaneous use |
40 mg/0.8 mL |
Idacio (available as disposable prefilled syringes, prefilled injection pens, vial kit for institutional use only) |
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Parenteral |
Injection, for subcutaneous use |
20 mg/0.2 mL |
Yuflyma (available as prefilled syringes) |
|
|
40 mg/0.4 mL |
Yuflyma (available as disposable prefilled syringe, prefilled syringe with safety guard, and prefilled autoinjectors) |
|||
|
80 mg/0.8 mL |
Yuflyma (available as disposable prefilled syringe, prefilled syringe with safety guard, and prefilled autoinjectors) |
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Parenteral |
Injection, for subcutaneous use |
10 mg/0.1 mL |
Hyrimoz (available as disposable prefilled syringes) |
|
|
20 mg/0.2 mL |
Hyrimoz (available as disposable prefilled syringes) |
|||
|
40 mg/0.4 mL |
Hyrimoz (available as disposable prefilled syringes and prefilled injection pens) |
|||
|
80 mg/0.8 mL |
Hyrimoz (available as disposable prefilled syringes and prefilled injection pens) |
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Parenteral |
Injection, for subcutaneous use |
10 mg/0.2 mL |
Cyltezo (available as prefilled glass syringes) |
|
|
20 mg/0.4 mL |
Cyltezo (available as prefilled glass syringes) |
|||
|
40 mg/0.8 mL |
Cyltezo (available as prefilled glass syringes and prefilled injection pens) |
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Parenteral |
Injection, for subcutaneous use |
10 mg/0.2 mL |
Abrilada (available as disposable prefilled syringes) |
|
|
20 mg/0.4 mL |
Abrilada (available as disposable prefilled syringes) |
|||
|
40 mg/0.8 mL |
Abrilada (available as disposable prefilled syringes, prefilled injection pens, and vial for institutional use only) |
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Parenteral |
Injection, for subcutaneous use |
40 mg/0.8 mL |
Yusimry (available as disposable prefilled injection pens) |
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Parenteral |
Injection, for subcutaneous use |
10 mg/0.2 mL |
Amjevita (available as disposable prefilled syringes) |
|
|
20 mg/0.2 mL |
Amjevita (available as disposable prefilled syringes) |
|||
|
20 mg/0.4 mL |
Amjevita (available as disposable prefilled syringes) |
|||
|
40 mg/0.4 mL |
Amjevita (available as disposable prefilled syringes and prefilled autoinjectors) |
|||
|
40 mg/0.8 mL |
Amjevita (available as disposable prefilled syringes and prefilled autoinjectors) |
|||
|
80 mg/0.8 mL |
Amjevita (available as disposable prefilled syringes and prefilled autoinjectors) |
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Parenteral |
Injection, for subcutaneous use |
40 mg/0.4 mL |
Hadlima (available as disposable prefilled syringes and prefilled autoinjectors) |
|
|
40 mg/0.8 mL |
Hadlima (available as disposable prefilled syringes, prefilled autoinjectors, and single-dose vial for institutional use only) |
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Parenteral |
Injection, for subcutaneous use |
20 mg/0.4 mL |
Hulio (available as disposable prefilled syringes) |
|
|
40 mg/0.8 mL |
Hulio (available as disposable prefilled syringes and prefilled injection pens) |
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Parenteral |
Injection, for subcutaneous use |
20 mg/0.2 mL |
Simlandi (available as a single-dose prefilled syringe) |
|
|
40 mg/0.4 mL |
Simlandi (available as a single-dose autoinjector and prefilled syringe) |
|||
|
80 mg/0.8 mL |
Simlandi (available as a single-dose prefilled syringe) |
AHFS DI Essentials™. © Copyright 2025, Selected Revisions June 10, 2025. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
† Off-label: Use is not currently included in the labeling approved by the US Food and Drug Administration.
Reload page with references included
Related/similar drugs
Biological Products Related to adalimumab
Find detailed information on biosimilars for this medication.
Frequently asked questions
- What medications are known to cause hair loss?
- What are the new drugs for rheumatoid arthritis (RA)?
- Can you take Humira with antibiotics?
- Cosentyx vs Humira: How do they compare?
- Skyrizi vs Humira for plaque psoriasis - How do they compare?
- Is Amjevita interchangeable with Humira?
- What is the difference between Cyltezo and Humira?
- What are the new drugs for plaque psoriasis?
- What are biologic drugs and how do they work?
More about adalimumab
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (748)
- Side effects
- Dosage information
- Patient tips
- During pregnancy
- Support group
- Drug class: antirheumatics
- Breastfeeding
Patient resources
Professional resources
- Adalimumab Injection prescribing information
- Adalimumab-aacf (FDA)
- Adalimumab-adaz (FDA)
- Adalimumab-adbm (FDA)
- Adalimumab-bwwd (FDA)
- Adalimumab-ryvk (FDA)
Other brands
Humira, Hyrimoz, Hadlima, Amjevita, ... +7 more